INTRODUCTION
Marble bone disease (Osteopetrosis; Osteosclerosis Fragilis Generalisata) is an inherited, rare autosomal bone disorder of unknown etiology. It was first described in 1904 by Albers Schonberg2, hence the disease also gets a name Albers Schonberg disease. This disorder includes impaired osteoclast function and marked increase in bone density.
The estimated prevalence of osteopetrosis is 1 in 100,000–500,000. It takes 2 major clinical forms-the autosomal dominant adult (benign) form is associated with few or no symptoms and the autosomal recessive infantile (malignant) form, if untreated, is typically fatal during infancy or early childhood.
A rarer autosomal recessive (intermediate) form presents during childhood with some signs and symptoms of malignant osteopetrosis. In especially rare cases, osteopetrosis may exist as lethal, transient infantile and post infectious forms. Most children born with the malignant form of osteopetrosis die during infancy. Due to better medical care the life expectancy of these patients has increased in recent years.
Most studies of osteopetrosis have concentrated on medical aspects (hepatosplenomegaly, anemia, increased susceptibility to infections most common is respiratory tract infections, cardiac disorders, multiple fractures etc) 3.
With increasing age, however, dental development and tooth eruption become a practical and medical problem4. In these patients to improve oral hygiene, especially in areas of exposed mandibular bone, 0.2% chlorhexidine formulations can be used. Fluoride applications can be done to decrease the susceptibility to dental caries.
This paper discusses a rare case of osteopetrosis with mandibular osteomyelitis with the purpose to review the entity and to reemphasize an important, less obvious, clinical presentation of osteopetrosis with mandibular osteomyelitis.
CASE REPORT:-
A 13yr old girl reported with the chief complaint of missing teeth. A detailed history was taken; patient had loss of vision and hearing impairment. Intraoral examination showed pale oral mucosa [fig.1],
 | Fig 1
 |
small sequestrum on left side of the mandible [fig.2].
 | Fig 2
 |
Investigations revealed following results: Abdominal sonography was suggestive of spleenomegaly (16.28×8.6 cm), homologous echo texture. Portal vein 12.6mm, whereas the size of liver, gall bladder, kidney were normal, no evidence of lymphadenopathy was seen.
The soft tissue attached to malformed tooth was sent for histopathologic examination which was suggestive of dentigerous cyst (possibility of follicle attached to the partially formed tooth) [fig.3]
 | Fig 3
 |
The laboratory test revealed Hb 9 mg%, WBC 2.3×109/L, DLC showed neutrophils 70% and lymphocytes 30%. Serum chemistry revealed Cl 106 mg/l and alkaline phosphatase 8.0 KA unit/dl.
The skull radiograph and radiograph of left mandible (oblique lateral view) showed increased bone density. The O.P.G X-ray [fig.4]
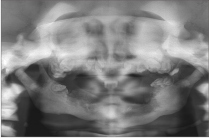 | Fig 4
 |
showed that all permanent tooth bud remained totally or partly embedded in basal bone. Vertical growth of alveolar ridge was very limited. Where a fenestration of overlaying mucosa had occurred, a localized, progressive osteitis developed, leading to soft tissue inflammation.
It has been documented that classical features of osteopetrosis can be misdiagnosed in cases of Kaffey’s disease, Myelofibrosis, Skeletal fluorosis, hypoparathyroidism. The confirmatory test would be using brain iso-enzyme of creatine kinase which is a biochemical marker of osteopetrosis.2The patient was diagnosed as a case of osteopetrosis with superadded mandibular osteomyelitis.
DISCUSSION
Osteopetrosis is a rare metabolic disease characterized by a generalized increase in skeletal mass. This inherited disorder results from a congenital defect in the development or function
of the osteoclast. Orthopedic problems in the intermediate and autosomal dominant forms include bone pain (26% of patients), increased fractures (40%) coxa vara, long bone bowing, hip and knee degenerative arthritis and osteomyelitis.
Dental abnormalities may be attributed to the pathological changes in osteopetrosis. Patients with the disease seem to be especially susceptible to caries. Constriction of canals housing neurovascular bundles that supply teeth and jaws, along with obliteration of the marrow cavities and the dental pulp chambers, is the most likely contributing factor to bone necrosis and dental caries. Other dental changes may include delayed eruption and early loss of teeth, enamel hypoplasia, malformed roots and crowns, and thickening of the lamina dura.5
Osteomyelitis, due to dental caries (10%), is well recognized hazard in osteopetrosis due to reduced blood circulation to bone as a result of obliteration and fibrosis of the marrow. It is a potentially severe infection that runs a protracted course, due to the accompanying severe anemia and neutropenia.6
The most common complication of the osteopetrosis is pathologic fractures; those with congenital presentation are likely to have the most fractures. Femoral shaft fractures either with transverse or short oblique pattern are most common. Other common locations are inferior neck of femur and posterior tibia. Upper extremity fractures are also reported. Fracture healing seems to occur at a normal rate but the onset of callus formation after injury is variable.7 Nonunion & delayed union of fractures may occur. Management of the patients with osteopetrosis requires a comprehensive approach to characteristic clinical problems including hematological and metabolic abnormalities, fractures, deformity back pain, bone pain, osteomyelitis and neurological sequalae. Medical management of osteopetrosis is based on efforts to stimulate host osteoclasts on provide in alternate source of osteoclasts. Stimulation of host osteoclast has been attempted with calcium restriction, calcitriol, steroids, parathyroid hormone and interferon. Hyperbaric oxygen has been shown to be beneficial in the treatment of mandibular osteomyelitis8 .It has a bactericidal and bacteriostatic effect in vitro and in vivo but the bone infection is not the only factor but reduced tissue resistance due to avascularity of the marrow spaces and the partial obliteration of the mandibular canal appeared to be the basic problem. The beneficial effect is probably resulted from the improved vascular supply and increased oxygen perfusion to the ischemic areas of infection.9
Bone marrow transplantation is the only permanent cure for osteopetrosis, but an appropriately matched donor is usually available for only about 50% of those affected, and engraftment is successful in about 45% of transplants.10 As osteopetrosis likely represents a spectrum of underlying etiologies resulting in osteoclast dysfunction, effective therapies need to be individualized. These patients should receive increased attention and prophylactic dental treatment to maintain their fragile oral health status. Frequent oral hygiene procedures with emphasis on chlorhexidine mouthwash should be advocated.2 Preventive measures must be continuously and rigorously maintained in patients of
osteopetrosis for the prevention against dental caries. Fluorides and diet counseling would be the mainstay for long term maintenance of oral health. Presence of bony sequestrum and cysts are common findings of this entity. Soft tissue infections, periodic exacerbations and remission of pus through numerous sinus tracts often make surgical intervention necessary. Complete dentures continue to have an important role in the treatment of edentulous patients. Edentulous ridges though the feature of old age can be seen in pediatric dental patients being affected by certain syndromes and as seen in this case also. Prior to treatment, diagnostic casts were obtained using irreversible hydrocolloid (putty) [fig.5].
 | Fig 5
 |
Custom tray was fabricated using self cure acrylic which was used later to make secondary/final impression [fig.6].
 | Fig 6
 |
Conventional border molding procedure with modeling plastic impression compound sticks was done on the fabricated custom trays. After border molding was completed secondary impression was made with the help of zinc oxide eugenol impression pastes and casts were poured. Occlusal rims were fabricated [fig.7] and jaw relations were recorded in centric
 | Fig 7
 |
relation. Complete denture is verified for esthetics, phonetics and necessary correction were made [fig.8]. Denture was
 | Fig 8
 |
delivered and patient recalled next day for post insertion. Prosthetic treatment includes partial or complete dentures. The maxillary dentures are well retained and well accepted by the children. The mandibular dentures often have poor stability and retention due to mandibular destruction both because of the pathology and the surgical intervention. In practice only the maxillary dentures are used.4
CONCLUSION
Complete prevention of this complication is not currently possible. Normal growth is a balance between osteoblastic (cells that create new bone tissues) and osteoclastic (cells that destroy old bone tissue) activity. In osteopetrosis, the osteoclasts do not function properly, leading to fragile bone status. So, the aim of our therapy should be not only to treat the oral complaints of patient but to provide a complete physical, mental, psychological rehabilitation of the patient so that he/she may lead a normal healthy life.
REFERENCES
1. I Ahmad, Sz Abbas, F Haque, M Rashid, SA Ahmad; "Osteomyelitis of Mandible"-A Rare Presentation of Osteopetrosis. Ind J Radiol Imag 2006 16:2:253-256.
2. David K. Lam, George K.B. Sándor, Howard I. Holmes, Robert P. Carmichael, Cameron M.L. Clokie; Marble Bone Disease: A Review of Osteopetrosis and Its Oral Health Implications for Dentists; JCDA ; November 2007, Vol. 73, No. 9:839-843.
3. Callum J Wilson; Autosomal recessive osteopetrosis; orphanet encyclopedia march 2003.
4. Kjell Bjorvatn, Ole Gilhuus-Moe and Dagfinn Aarskog; Oral aspects of osteopetrosis; Scand. J. Dent. Res. 1979: 87: 245-252.
5. Dick HM, Simpson. J Dental changes in osteopetrosis. Oral Surg 1972 sept; 34:408.
6. Lawoyin DO, Daramola JO, Ajabge HA, Nyako EA, Lawoyin JO. Osteomyelitis of the mandible associated with osteopetrosis: Report of a case.Br J of oral and max surg.1988; 26:330-5.
7. Stoker DJ.Osteopetrosis.Semin musculoskel radio.2002dec; 6(4):299-305.
8. Mainous EG, Boyne PJ, Hart GB. Hyperbaric oxygen treatment of mandibular osteomyelitis: Report of three cases. J am dent assoc1973; 87:1426.
9. Mainous EJ, Hart GB, Soffa DJ, Graham GA. Hyperbaric oxygen treatment of mandibular osteomyelitis in osteopetrosis. J oral surg 1975 April; 33:288-291.
10. Neville BW, Damm DD, Allen CM, and Bouquot JE. Bone pathology. In: Oral and maxillofacial pathology. 2nd ed. China: Saunders; 2002.p. 533–87. |