Introduction
Amelogenesis imperfecta (AI) is a term for a clinically and genetically heterogeneous group of conditions that affect the dental enamel, occasionally in conjunction with other dental, oral and extra-oral tissues.[1] Its main characteristic being the loss of tooth structure compromised esthetic appearance, and dental sensitivity.[2] The prevalence varies from 1:700 to 1:14,000 depending upon the population studied and the diagnostic criteria.[3] AI is caused by mutations in genes that control amelogenesis and follows autosomal dominant, autosomal recessive, sex linked or sporadic inheritance patterns. The other causes of amelogenesis imperfecta include febrile illness, vitamin deficiency, local infection, trauma, fluoride ingestion, congenital syphilis, birth injury, premature birth or idiopathic factors.[2]
According to the Witkop(1988) classification system, there are four main forms of AI: type I hypoplastic enamel, type II hypomatured enamel, type III hypocalcified enamel and type IV hypomatured-hypoplastic enamel with taurodontism. In the hypoplastic type, the enamel is well mineralized but its amount is reduced. In the hypomature type, the affected teeth exhibit mottled, opaque white-brown or yellow discolored enamel, which is softer than normal and detaches from dentin .The hypocalcified type shows pigmented, softened, and easily scrapable enamel.[3] Other dental anomalies associated with AI includes multiple impacted teeth, congenitally missing teeth, open occlusal relationship, and taurodontism.[4]
This case report presents a conservative esthetic and functional management of an adolescent patient affected by amelogenesis imperfecta.
Case Report
A 13 year old female reported to the Department of Pedodontics and Preventive Dentistry with the complaint of poor esthetics and severe discoloration of the teeth since childhood with generalized sensitivity (Fig 1). The medical history was not significant. The parents reported of consanguineous marriage and no case was reported in the family. The two younger female siblings except the youngest brother were also affected similarly. On clinical evaluation, teeth were in mixed dentition stage with permanent molars in Angle’s class I relationship. All the permanent canines were unerupted except the left mandibular canine. The teeth appeared dark yellow to dark brown in color with generalized spacing. The tooth surfaces were pitted, grooved, thin and scrapable (Fig 1). The primary dentition was also completely affected. Restorations were done on permanent mandibular first molar on right and left sided. Root canal treatment was done with permanent maxillary left first molar. Other relevant findings included generalized occlusal attrition and deep bite. Based on the phenotypic and radiographic presentation, a diagnosis of hypocalcification type of AI (HCAI) was rendered.
The treatment plan was directed based on patient’s age and needs. The preventive aspect included diet and parent counseling and oral prophylaxis using polishing brush. GC tooth mousse (GC asia dental pte. Singapore) was adviced twice daily for caries prevention and desensitization. All the permanent molars were restored with preformed stainless steel crowns (3M, Unitek, USA) of appropriate sizes. Crown preparation was done by minimal proximal reduction and odontoplasty of the enamel peaks of the occlusal surface. The crowns were tried in the quadrants and were cemented using a luting resin modified glass ionomer cement (RMGIC) (3 M ESPE, USA) after confirmation in occlusal relations.
After considering the age of the patient, the anterior affected teeth were decided to be restored with direct composite veneering. A compromised bonding in hypocalcification type of AI is reported in the literature. So a composite veneering was done with maxillary left lateral incisor to check the bonding using deproteinization technique (Fig 2 and fig 3). The teeth were prepared, conditioned by rubbing sodium hypochloride 5.25% for 1 minute and rinsed. Acid etching was done using 37% phosphoric acid (Scotchbond, Dentsply, USA) for 15 seconds. The single bottle adhesive (Prime and Bond NT, Dentsply Caulk) was applied and light cured for 40 seconds. The composite veneering (Esthet-X, Dentsply) was done using opaque composite to mask the dark discoloration. Resin veneering was done by appropriate shades using stratified layer technique. Complete oral rehabilitation was done conservatively (Fig 4, Fig 5 and Fig 6). Six monthly follow up was done till 18 months.
 | Fig 1. Preoperative clinical picture showing irregular dark yellow to brown discolored labial surface of maxillary and mandibular teeth
 |
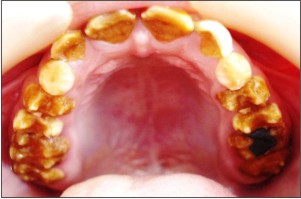 | Fig 2. Preoperative clinical picture showing attrited occlusal surface of maxillary teeth
 |
 | Fig 3. Preoperative clinical picture showing attrited occlusal surface of mandibular teeth
 |
 | Fig 4. Postoperative clinical picture showing composite veneering and stainless steel crowns in posterior teeth in maxillary arch
 |
 | Fig 5. Postoperative clinical picture showing composite veneering and stainless steel crowns in posterior teeth in mandibular arch
 |
 | Fig 6. Postoperative clinical picture showing esthetic composite veneering in maxillary and mandibular teeth
 |
Discussion
Management of a patient with AI is a challenge for a dental clinician. The treatment options vary considerably depending on several factors such as age of the patient, severity of disorder, socioeconomic status and most importantly patient's age and cooperation.[4] Numerous treatment modalities based on prognosis have been described for the rehabilitation of AI involving combination of extractions, adhesive restorations, stainless steel crowns, overdentures, porcelain crowns and veneers after crown lenghtening.[5] The crown lengthening is least advisable at young age.
The placement of direct composite veneers by means of adhesive techniques has various advantages over their indirect counterparts on account of easy repair, no laboratory stages, less working time, lower cost, and more conservative preparation. The indirect composite technique could not form proper proximal contact due to interdental spacing between many primary and permanent teeth.[6]
In the present case, age of patient, bonding problem with hypomineralized enamel, thickness of remaining dentin, affordability of the treatment precluded the restoration with ceramic veneers. The high mineral content in sclerotic dentine affects the formation of hybrid layer and results in lower bond strength. A few studies reported high failure rates in resin bonding to dentine of AI-affected teeth due to morphologically altered tooth structures.[7] The deproteinization of teeth remove the excess protein and leave carbonates and phosphates from the tooth surface to form strong bond with hypermineralised dentin and hypocalcified enamel. The bonding agent diffuses better within the deproteinized substrate, forming a more homogeneous bonding layer that may be potentially less sensitive to hydrolytic degradation over the course of time.[8]
The use of preformed stainless steel crowns decreased the need of occlusal and proximal preparations in highly attrited and soft teeth.[9] gingival finish line was conservative and caused less chance of sensitivity. They were and self adapting in the occlusion. The crowns were cemented with RMGIC to reduce post operative sensitivity.[10]
Conclusion
The prosthetic rehabilitation of AI patient is vital for restoring form, functions and esthetics. Minimal invasive technique for early correction is essential for psychological benefits and prevention of the dental damage. The severity and type of disease, expectations, affordability and acceptability is of prime concern for deciding the treatment plan. The more extensive treatment should be done after completion of growth and eruption of teeth.
References
1. Crawford PJM, Aldred M and Bloch-Zupan A. Amelogenesis Imperfecta. Orphanet Journal of Rare Diseases 2007, 2:17.
2. Oliveira IK, Fonseca J de F, do Amaral FL, Pecorari VG, Basting RT, França FM. Diagnosis and esthetic functional rehabilitation of a patient with amelogenesis imperfecta Quintessence Int. 2011 Jun; 42(6):463-9.
3. B. W. Neville, D. D. Douglass, C. M. Allen, and J. E. Bouquot. “Abnormalities of teeth,” inOral and Maxillofacial Pathology,pg. 89–94, Elsevier, Philadelphia, Pa, US, 2004.
4. Markovic D, Petrovic B, Peric T. Case series: Clinical findings and oral rehabilitation of patients with amelogenesis imperfecta. European Archives of Paediatric Dentistry 2010; 11: 4.
5. Sholapurkar AA, Joseph RM, Varghese JM, Neelagiri K, Acharya SR, Hegde V, Pai KM, Bhat M. Clinical diagnosis and oral rehabilitation of a patient with amelogenesis imperfecta: a case report. J Contemp Dent Pract. 2008 May 1; 9(4):92-8.
6. Reis A, Higashi C, Loguercio AD. Re-anatomization of anterior eroded teeth by stratification with direct composite resin. J Esthet Restor Dent 2009; 21:304–16.
7. Seow WK, Amaratunge A. The effect of acid-etching on enamel from different clinical variants of amelogenesis imperfecta. Pediatr Dent 1998; 20:37-42.
8. Saroglu I, Aras S, Oztas D. Effect of deproteinization on composite bond strength in hypocalcified amelogenesis imperfecta.Oral Dis. 2006 May;12(3):305-8.
9. Law Kwok-Tung, Nigel M King. The restorative management of Amelogenesis Imperfecta in the mixed dentition. J Clin Pediatr Dent 2006; 31(2):130-135.
10. V Chandrasekhar. Post cementation sensitivity evaluation of glass Ionomer, zinc phosphate and resin modified glass Ionomer luting cements under class II inlays: An in vivo comparative study. J Conservative Dent. 2010; 13(1): 23–27.
|