Introduction
Odontogenic keratocyst (OKC) are developmental, non- inflammatory odontogenic cysts derived from either the epithelial remnants of the tooth germ or the basal cell layer of the surface epithelium, first identified and described in 1876[1], and further characterized by Philipsen in 1956.[2] It’s one of the most aggressive odontogenic cysts of the oral cavity.[3] OKC most often occurs in 2nd and 3rd decades of life and shows a slight male predilection (male: female ratio is 1.3:1)[4]. It may occur in any part of the upper and lower jaw, with majority occurring in the mandible, most commonly in the angle, body and ramus of the mandible.[5],[6],[7],[8],[9].
OKCs are known to have a high recurrence rate ranging between 13 to 60 %.[10],[11],[12] This high recurrence rate has been attributed to the presence of epithelial remnants of satellite cysts in the osseous margin.[13],[14] Because of this, enucleation has usually been recommended with excision of a satisfactory margin.[15] However, there is no experimental evidence to reject marsupialisation as a definitive treatment.
In this case report, a 23 year old, unmarried, male patient with biopsy proven multiple OKCs was treated with marsupialisation followed by enucleation and chemical cautery. Conservative therapy was preferred as the patient opted for the same. Hence marsupialisation was performed, followed by careful enucleation and chemical cautery with Carnoy’s solution in the second stage (6 months later).
Case Report
A 23 year old male patient reported to departmental OPD with the chief complaint of swelling in lower right side of the face since 1 year. The swelling was small at onset, but gradually increased to the present dimensions, from mandibular right first molar to the mandibular left canine. The patient also gave history of pain in right lower posterior teeth since 4 months. There was a little heaviness and numbness in the right side of lower lip, owing to paraesthesia of the right inferior alveolar nerve.
Intra-orally there was a marked bone expansion of the buccal plate in right mandibular body region, with obliteration of the vestibule and slight expansion of the lingual cortical plate in the region of right first premolar. There was mild erythema but no raise in temperature, ulceration or fistula formation in overlying soft tissues. On palpation, there was tenderness and egg-shell crackling in the right mandibular body. There was varying degree of tooth mobility ranging from grade I to II, more in relation to the right canine, premolar and first molar. Mandibular right first molar was badly carious as well as non-vital. On left side of the face, there was no obvious swelling, but on radiograph there was presence of radiolucency in relation to left mandibular premolars and first molar, which may have been another focus of OKC. On aspiration, there was clear straw coloured fluid, thick and gelatinous in consistency.
Panoramic radiography revealed presence of a multilocular (soap-bubble like) radiolucency extending from right first molar to left canine, with a non sclerotic, scalloped border, cortical expansion and thinning of inferior border of mandible, and resorption of the roots of teeth involved in the radiolucency. There was another well-defined, unilocular, rounded radiolucency with smooth margins, about 2 cm in diameter, in relation to left mandibular first premolar and first molar(Fig.1).
 | Fig.1 : Panoramic radiograph showing multilocular radiolucency extending from right mandibular first molar to left canine and unilocular radiolucency in relation to left mandibular first premolar and first molar.
 |
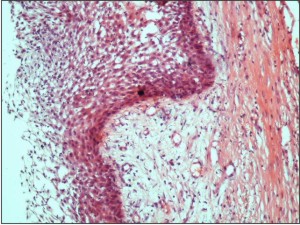 | Fig.2 : Histologic slide showing stratified squamous epithelium with areas of focal thickening.
 |
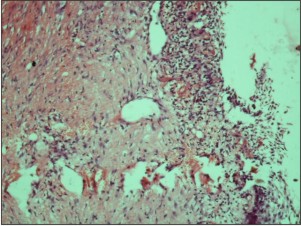 | Fig.3 : Histologic slide showing epithelial lining with epithelial remnant in connective tissue capsule.
 |
A provisional diagnosis of ameloblastoma or odontogenic keratocyst was made. The patient’s skull and chest radiographs were unremarkable. Dermatological consultation did not reveal any cutaneous abnormalities. Hematologic investigations were also within normal range.
An incisional biopsy was obtained during marsupialisation of the right mandibular lesion under local anaesthesia, and sent for histopathological examination. The smaller left mandibular lesion was enucleated and sent for histopathological examination in toto. The histopathological analysis by processing, sectioning and staining of histological slides with Haematoxylin and Eosin (H&E) revealed that the lining of the cystic lesions was stratified squamous keratinized epithelium with underlying connective tissue. The epithelium was thin, with a corrugated surface and palisading of the basal cell layers. The underlying connective tissue showed dense patchy infiltration of inflammatory cells. Some mucous cells could also be seen in the stroma (Fig. 2, 3).
All these features, co-related with clinical and radiographic findings, were pathognomic of diagnosis of an Odontogenic keratocyst.
The patient was followed up regularly for the period of next 6 months, and the resultant gradual reduction in the right mandibular lesion size was observed. The left side lesion had radiographic evidence of healing by appearance of new bony trabeculae. The time was then thought to be appropriate for the second part of the treatment plan, namely careful, extensive enucleation, and chemical cauterization with Carnoy’s solution of the right mandibular lesion.
The patient has been reporting for regular follow-up visits since the last 1 year, and has shown satisfactory healing with no signs of recurrence so far.
Discussion
Multiple OKCs usually occur along with nevoid basal cell carcinoma syndrome (NBCCS), also called Gorlin-Goltz syndrome[16],[27],[30], or Ehler-Danlos syndrome[17], or orofacial digital syndrome.[18] Our patient, however, was generally healthy, with no features suggestive of any syndromic entity.
The incidence of OKCs is higher in 2nd and 3rd decades of life, in males (with a male: female ratio of 1.3:1)[4], and in the mandible as compared to maxilla (with a mandible to maxilla ratio of 2:1)[19]. Patients with multiple keratocysts (syndromic or non - syndromic) are generally younger as compared to patient with single odontogenic keratocysts.[20] These features mostly coincide with our case presented in this report. Most common clinical feature presented by OKC is swelling, pain or both. Our patient presented with both these clinical features.
Radiographically, OKCs present as well-defined radiolucent lesions which maybe unilocular or multilocular, with smooth cortical or, more often, scalloped margins.[14], [21], [23], [31] Our patient had both a unilocular and a multilocular lesion each, with smooth as well as scalloped margins, respectively. Root resorption and paraesthesia are common phenomena in these relatively aggressive cystic lesions, as also evidenced by our case report. Unerupted teeth are involved in 25-40% keratocysts[21], which however, was not the case in this patient.
Histologically, our patient with OKCs (but non syndromic i.e. without NBCCS), revealed the presence of para-keratinized stratified squamous epithelium, in line with the pathognomic picture of OKCs.[21],[23],[31]
Treatment modalities for OKCs range from simple marsupialisation or enucleation, to enucleation with chemical cautery, cryotherapy, or peripheral curettage, to radical or segmental resection with reconstruction. Various authors have given various treatment and follow-up protocols for OKCs.[14],[15],[24],[25],[26],[28],[29],[30] However, many factors besides the lesion’s presentation, site, size etc are also important for decisions regarding treatment plan. The patient’s age, education, medical condition, availability for follow- up, and expected quality of life are all important. Our patient, who is a young, unmarried, well educated adult, can comprehend the requirements of his condition and the need for follow-up, and compromising his quality of life at such a young age by resection is not an immediate need, but can rather be taken up a later stage if necessary. Hence marsupialisation was performed, followed by careful enucleation and chemical cautery with Carnoy’s solution in the second stage i.e.6 months later.
Moreover, presence of multiple cysts does not necessarily mean that the patient has more than one cyst at a given time, but means occurrence of cysts over the patient’s lifetime.[22] This patient has already evidenced the incidence of two concurrent OKCs. The possibility of his developing further new cystic lesions cannot be entirely ruled out. Nor can it be categorically stated that this patient will not have any signs or symptoms of NBCCS in his near or distant future. Therefore a thorough examination and a lifelong follow-up is essential for such patients. Moreover, genetic counselling is also advisable if the possibility of a syndrome is visualized.
Conclusion
The possibility of NBCCS should always be considered in case of multiple OKCs. A complete clinical examination and thorough histopathological analysis must be performed to detect any features associated with the above syndrome. The absence of enough criteria to confirm the diagnosis of a syndromic entity at the time of presentation does not rule out the possibility of manifestation of syndromic features in future. Hence a long term follow up is essential. Moreover, conservative treatment of OKCs (such as marsupialisation followed by enucleation with adjunctive procedures) is more advisable in young patients, as more aggressive modalities can severely compromise the patient’s aesthetics, function and quality of life.
References
1. Voorsmit RA. The incredible keratocyst: a new approach to treatment. Dtsch Zahnarzti Z 1985; 40 (6): 641-4.
2. Philipsen HP. Om Keratocystedr (Kolesteratomer) and Kaeberne. Tandlaegebladet 1956; 60: 963-971.
3. Shear M. Developmental odontogenic cysts: an update. J Oral Pathol Med 1994; 23: 1-11
4. Daley TE, Wysocki GP. New developments in selected cysts of the jaws. J Can Dent Assoc. 1997; 63 (7): 526-7, 530-2.
5. Haring JI, Van Dis ML. Odontogenic Keratocysts; a clinical, radiographic and histopathologic study. Oral Surg Oral Med Oral Pathol 1988; 66: 145-53.
6. Brondum N, Jensen VJ. Recurrence of keratocysts and decompression treatment. A long term follow up of forty- four cases. Oral Surg Oral Med Oral Pathol 1991; 72: 265-69.
7. Woolgar JA, Rippin JW, Browne RM. A comparative study of the clinical and histological features of recurrent and non recurrent odontogenic keratocysts. J Oral Pathol 1987; 16: 124-28.
8. Ved tofte P,Praetorious F . Recurrence of odontogenic keratocyst in relation to clinical and histological features. Int J Oral Surg 1979 ; 8: 412-20.
9. Forssell K. The primordial cyst: a clinical and radiographic study. Proc Finn Dent Soc 1980; 76: 129-74.
10. Stoelinga PJW, Bronkhorst FB. The incidence, multiple presentation and recurrence of aggressive cysts of the jaw. J Cranio - Max- Fac Surg 1988; 16: 184-95.
11. Browne RM. The odontogenic keratocyst – clinical aspects. Br Dent J 1970; 128: 225-31.
12. Baenes L, Eveson JW, Reichart P, Sidransky D. Pathology and genetics of head and neck tumours, Lyon: IARC Press; 2005. WHO classification of tumours.
13. Ogunsalu C, Daisley H , Kamta A, Kanhai D, Manker M, Maharaj A. Odontogenic keratocyst in Jamaica : A review of five new cases and five instances of recurrence together with comparative analysis of four treatment modalities . West Indian Med J 2007; 56 (1): 90.
14. Avinash Tejasvi ML, Balaji Babu B, Malik Afroz M. Keratocystic odontogenic tumour mimicking Radicular cyst: A clinical dilemma. IJDA 2010; 2(4): 387-390.
15. Blanas N, Freund B, Schwartz M, Furst IM. Systematic review of the treatment and prognosis of the odontogenic keratocyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 90: 553-8.
16. McGrath CJ, Myall RW. Conservative management of recurrent keratocysts in basal -cell naevus syndrome. Aust Dent J 1997; 42(6):399-403.
17. Carr RJ, Green DM. Multiple odontogenic keratocysts in a patient with type II (mitis) Ehler –Danlos syndrome. Br J Oral Maxfacial Surg 1988; 26(3): 205 -14.
18. Linde boom JA, Kroon FH, De Vires J, Van den Akker HP. Multiple recurrent and de novo odontogenic keratocysts associated with oral – facial- digital syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003; 95(4): 458-62.
19. Brannon RB. The odontogenic keratocyst. A clinicopathologic study of 312 cases. Part I Clinical features. Oral Surg Oral Med Oral Pathol 1976; 42(1): 54-72.
20. Gonzalez – Alva P, Tanaka A, Oku Y, Yoshizawa D, Itoh S, Sakashita H et al. Keratocyst odontogenic tumour: A retrospective study of 183 cases. J Oral Sci 2008; 50:205-212.
21. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and Maxillofacial pathology. 2nd ed .Philadelphia: Saunders: 2002.
22. Woolgar JA, Rippin JW, Browne RM. The odontogenic keratocyst and its occurrence in the nevoid basal cell carcinoma syndrome. Oral Surg Oral Med Oral Pathol 1987; 64 (6): 727-30.
23. Chen C-H, Lin C-C. Clinical and histopathological study of the odontogenic keratocyst – a follow up study of 16 cases. Kaohsiung J Med Sci 1986; 2: 601- 07.
24. Voorsmit RACA, Stoelinga PJW, Van Haelst UJGM. The management of keratocysts. J Maxillofac Sur 1981; 9: 228- 236.
25. Irvine GH, Bowerman JE. Mandibular Keratocyst: surgical management. BrJ Oral Maxillofac 1985; 23: 203-209.
26. Pogrel MA. Treatment of keratocysts: The case for decompression and marsupialisation. J Oral Maxillofac Sur 2005; 63: 1667-73.
27. Kulkarni P, Brashear R, Charang T. Nevoid basal cell carcinoma syndrome in a person with dark skin. J Am Acad Dermatol 2003; 49: 332-5.
28. Zedan W, Robinson PA, Markham AF, High AS. expression of sonic hedgehog receptor ‘pathched’ in Basal cell carcinomas and odontogenic keratocysts. J Pathol 2001; 194: 473-7.
29. Kalia V, Kaushal N, Kalra G. The syndromic multiple odontogenic keratocyst in siblings: A familial study. Annals of Maxillofacial surgery 2011; 1(1): 77- 82.
30. MacDonald – Jankowski. Keratocystic odontogenic tumour: systematic review. Dentomaxillofacial Radiology 2011; 40: 1-23.
31. Rory O’Neill, Khalid AH. Identification of an odontogenic keratocyst and treatment with guided tissue regeneration: case report. J Can Dent Assoc 2011; 77: b6. |