Introduction
Metals and alloys have been used to make part or whole of the dental prostheses in fixed,
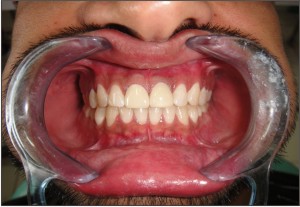
 | Figure 1 - Preparation of 11, 21 teeth for zirconia crowns
 |
 | Figure 2 - Zirconia crowns on 11, 21
 |
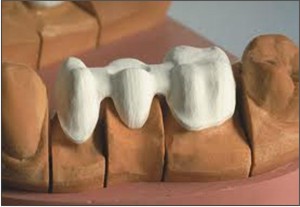 | Figure 3 - Zirconia 3- unit FPD framework made by CAD- CAM technique
 |
 | Figure 4 - Zirconia abutment
 |
removable and implant prosthodontics since years mainly because of their superior durability and high fracture resistance compared to other restorative materials. However, there have been concerns about their biocompatibility, corrosion and poor esthetics. Ceramics , on the other hand , exhibit many desirable properties including excellent esthetics, biocompatibility, diminished plaque accumulation, low thermal conductivity, high hardness which lead to their enormous use in metal- ceramic restorations. A great effort has been expended to overcome their principal deficiencies - brittleness, low fracture toughness and low tensile strength which has resulted in the evolution of newer high strength ceramic systems for construction of metal free restorations such as alumina, spinel, lithium-disilicate reinforced and zirconia based ceramics. While alumina based ceramics can be used safely for anterior restorations such as crowns and three unit FPD'S, it lacks the strength for usage in posterior restorations.[1] Zirconia, has been a material of increasing interest and has gained a dramatic rise in popularity as it exhibits high flexural strength(>1Gpa) and fracture toughness (9-10 MN/m 3/2) compared to other ceramic systems along with biocompatibility and enhanced esthetics. In the field of dentistry, Zirconia has been used for endodontic posts and orthodontic brackets since early 1990s and for fixed restorations since late 1990s.[2] Because of its properties, Zirconia seems to be a versatile material and its use is being evaluated in a variety of other clinical applications in dentistry.
Structure and Properties
Zirconia is a crystalline dioxide of zirconium and exhibits a polymorphic structure with monoclinic, tetragonal and cubic crystalline phases . Pure Zirconia at room temperature is monoclinic and stable till 1170°C. Above this temperature it transforms itself into tetragonal and then further into cubic phase at 2370°C. To control phase transformations and stabilize zirconia at room temperature, yttria (Y2 O3) is added to the crystal structure to form multiphase materials, called partially stabilized zirconia(PSZ) or Yttria-stabilized Tetragonal Polycrystals (Y-TZP). This material possesses a unique characteristic called tranformation toughening, which is the ability to stop the growth of cracks. Tensile stresses generated by an imminent crack induce a change from the tetragonal configuration to a monoclinic configuration and a localized volume increase of 3% to 5% . This volume increase results in a change of tensile stresses to compressive stresses generated around the tip of the crack. The compressive forces counter the external tensile forces and stop the crack from advancing.[3] This characteristic accounts for the material's low susceptibility to stress fatigue and high flexural strength of 900 MPa to 1200 Mpa. The material has about 2000MPa compressive strength and young's modulus of about 210Gpa (similar to stainless steel-193Gpa).These mechanical properties are highest ever reported for any dental ceramic.[3],[4]
Types of Zirconia
Three main types of zirconia are available for use in clinical dentistry - Green(non- sintered) , pre-sintered(partially sintered) and fully sintered.[2],[5] The most common method to fabricate a zirconia substructure is by CAD/CAM milling from a solid block. The fully sintered zirconia is milled at a 1:1 ratio, while the partially sintered zirconia is milled 20% to 25% larger than the desired final size due to shrinkage caused by the sintering process. The milling of green stage and partially sintered zirconia blocks is faster and causes less wear and tear on the hardware than the milling of fully sintered blocks. For both the partially sintered and the fully sintered techniques, the die is scanned, and then the computer program designs the framework or the coping. After the milling and any necessary sintering, the veneering porcelain is then hand-applied over the zirconia for the restoration's final shape and shade. For clinical success, the layering porcelain ideally should have the same coefficient of thermal expansion as the zirconia substructure, and therefore only specifically engineered porcelains are used. As an alternative to veneering, full contour zirconia crowns can also be made by milling.
Zirconia Fixed Partial Dentures
Clinical aspects
While other all ceramic systems can be used to replace anterior teeth with single crown restorations or maximum with three unit FPD'S , Zirconia restorations can be used in both anterior and posterior regions because of their superior strength.[2],[3],[5],[6] They have exhibited survival rates similar to metal ceramic FPDs.[2],[6]
Appropriate measures have to be taken while selecting the patient in addition to detailed intra oral examination as part of diagnosis. Criteria for patient selection are interocclusal space, para-functional habits and mobility of the tooth.[7] Contraindications are as follows.
a) As cantilever pontic
b) In class II div II malocclusions patients, due to deep bite there will be insufficient space for labo-lingual connector width.
c) Mesial tilting of abutment tooth with supra erupted teeth, which cannot be corrected with minimal enameloplasty.
d) Very short clinical crown that does not permit height of connector (occlusal-gingival).
Although some manufacturer allow obtaining full arch restorations, the maximum span of zirconia FPDs remains controversial. As supported by evidence, 5 units-FPDs are reported to be as maximal possible.[3],[8] Manufacturers suggest that two abutment FPDs can have a 38-mm span, and multiple abutment FPDs can have a span of 47 mm.[5]
The finish lines recommended during tooth preparation are rounded shoulder and chamfer. The 90o shoulder line angle should be avoided as the sharp axiogingival line angle is not captured well with the laser scanner used during CAD-CAM manufacturing.The finish line can be subgingival or even juxtagingval.[1],[5] (Figure -1,2)
Occlusal reduction of approximately 1.5-2mm and axial reduction of approximately 1.2- 1.5 mm is recommended. The axial taper of the preparation should be 4o-6o. Sharp angles in the preparation must be avoided.[3],[5],[7]
A higher fracture strength was found when Zirconia core thickness is optimized in order to obtain a uniform thickness of veneer ceramic. The minimum recommended core thickness is 0.5mm.[3],[8] (Figure 3)
The most common fracture pattern of tested Zirconia-based FPDs was at the loading point and through one or both connectors. Therefore the connector design is crucial for the fracture resistance and longevity of Zirconia-based FPDs.[2] The primary mode of failure is fracture, usually located in the area between the retainer and the pontic, emanating from the gingival surface of the connectors under high tensile stress, resulting in catastrophic loss. An in vitro test evaluating moduli of rupture with a three point bending test suggests that placing Zirconium on the intaglio surface of the pontic and connector area instead of veneering porcelain may increase the load bearing capacity of FPD upto 10 times. A minimum connector girth of 9 mm2 has been recommended for three unit FPDs.[9] In case of FPDs, the minimum clinical height of prospective abutment teeth (inter-proximal papilla to marginal ridge) should be 4mm.[3],[7]
Clinical Study Results
1. Zirconia based FPDs exhibited promising clinical results with a high survival rate (over 95%) in most of the studies indicating that zirconia ceramics could be a valid alternative to metal frameworks.[2],[10] Raigrodski et al in a systematic review of clinical studies in terms of survival and complications have concluded that the short term clinical data available so far suggest that zirconia-based fixed dental prostheses may serve as an alternative to metal ceramic fixed dental prostheses in the anterior and posterior dentition.[6]
2. Gonzalo et al found that marginal discrepencies for zirconia-based FPDs were significantly smaller than those for metal ceramics.[2]
3. The fracture toughness of zirconia based three unit FPDs has been found to be almost three times higher than those fabricated with the ceramic materials leucite- reinforced glass ceramics and Inceram alumina indicating that these have the potential to withstand occlusal forces even in the posterior region.[2],[3]
Aesthetics and colour :- Zirconia is opaque.This property can be an advantage when a dischromatic teeth or a metal post must be covered by a core and to mask metal implant abutments. However, if the preparation is inadequate or the coping is too thick, or the connectors are too large, the result will be an aesthetically unappealing crown that looks too bulky. Some manufacturers make provision for zirconia colored cores or staining of cores in order to enhance aesthetic outcomes.[3],[8] That allows layering of various tranclucencies of porcelain to develop a restoration that demonstrates 'color from within'.[5],[7] The radiopacity of zirconia is very useful for monitoring marginal adaptation through radiographic evaluation, especially when intrasulcular preparation is used.[3]
Cementation techniques :- Zirconia restorations can be cemented using Glass ionomer cements or adhesive bonding. However, a resin bond to tooth and ceramics that has sufficient durability is preferred and becomes necessary in some clinical situations , such as compromised retention with short abutments or extremely tapered preparations.[2],[5] Zirconia does not etch with hydrofluoric acid due to lack of a glass matrix, nor does it contain silica to allow silane coupling to occur. Conventional methods applied to the bonding to silica based ceramics (acid etching and silane application) are not successful for bonding to high strength ceramics. The methods to achieve superior bonding to zirconia framework include air borne particle abrasion ,using a chemical surface treatment with the trobochemical silica coating prior to bonding and using a specific adhesive with hydrophobic phosphate monomer (10-methacryl oxydecyl dihydrogen phosphate -MDP).[2],[11]
Potential problems :-
1. Chipping of veneer- The most commonly reported complication is chipping or cracking of the porcelain veneer. This is attributable to thermal incompatability, mechanical insufficiency of veneering porcelain, and inappropriate framework support for the veneer.[2],[12] The framework should be anatomically designed to provide support for the veneering porcelain. An 'overpressing technique' whereby a ceramic is pressed onto zirconia framework has also been introduced to overcome this problem.[2]
2. Ageing- The ageing of Y-TZP zirconia is a low-temperature degradation phenomenon. It is characterized by a progressive, spontaneous transformation of the tetragonal phase into the monoclinic phase (T-M), which results in diminished mechanical properties. Sato et al proposed that a slow T-M transformation occurs when Y-TZP is in contact with water or body fluid which leads to surface damage. The reaction of water with zirconia at the tip causes a formation of zirconia hydroxide, which accelerates crack growth of pre-existing flaws and promotes the T-M phase transition. The most critical temperature range for the development of aging is 200°C to 300°C. Grinding zirconia without a water coolant can produce a hot spot measuring up to 1500°C, which can induce a T-M phase change.[8] It is, therefore, recommended to use water cooling and avoid spot heating when trimming or poilishing zirconia restorations.
Inlay-retained or resin-bonded zirconia- based FPD'S
From the view point of minimum intervention, Zirconia - based three unit inlay retained FPDs with connector dimensions of between 9 and 12mm[2] can be used clinically by considering the maximum chewing forces in the posterior region.[2]
Inlays and Onlays
Edelhoff proposed inlays and onlays with a zirconium oxide core. An occlusal reduction of almost 2 mm and the axial reduction of 1.5 mm with a cavosurfacial angle of 100-120o has been
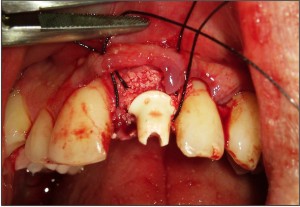 | Figure 5 - Zirconia abutment (placed on an immediate implant) before temporization.
 |
recommended.[3]
Zirconia Post And Core
The use of a zirconia post with an all-ceramic crown in patients who have high lip line and thin gingival tissue can help achieve good esthetics, while maintaining an adequate level of strength. In vitro studies indicated that direct heat-pressed ceramic cores instead of composite cores seemed to be more advantageous for zirconia posts because of improvement in fracture resistance as well as retentive strength to post.[13]
Zirconia Abutments
The dental implants and abutments are usually fabricated out of commercially pure Titanium primarily because of its well documented biocompatibility and mechanical properties.The titanium abutments, however, have the disadvantage of the metallic components showing through the thin soft tissue ,especially, in cases with thin gingival biotype.[14],[15] The use of ceramic abutments reduces this risk, allowing for optimal adaptation between the margins of the restoration and the soft tissue.[3] The use of zirconia abutments and 1-piece frameworks for dental implants has improved esthetics by eliminating the need to mask the dark oxide color of cast or milled alloys.These abutments are available in pre-fabricated or customizable forms and can also be prepared by CAD-CAM techniques. (Figure - 4, 5)
Butz et al. evaluated the survival rate and fracture strength of Zirconia abutment and concluded that Zirconia abutments were comparable to titanium ones (281 N as opposed to 305 N). The authors concluded that zirconia abutments can be used as an aesthetic alternative for the restoration of single implants in the anterior region.[3],[15]
Bacterial adhesion, which is an important aspect in order to maintain zirconia restorations without marginal infiltrations or periodontal alterations, proved to be satisfactorily slight; Scarano et al. reported a degree of coverage by bacteria of 12.1% on zirconia as compared to 19.3% on titanium.[16] Rimondini et al. confirmed with an in vivo study that Y-TZP accumulated fewer bacteria than Titanium in terms of the total number of bacteria and presence of potential putative pathogens. Moreover, Zirconium oxide creates less flogistic reaction in tissue than other restorative materials such as titanium. This result was also confirmed by a study about peri-implant soft tissue around zirconia healing caps in comparison with that around titanium ones.[3]
Zirconia Implants
Newly proposed zirconia implants seem to have good biological and mechanical properties. Kohal reported an all ceramic custom made zirconia implant system for the replacement of a single tooth. [17] Sennerby et al concluded that removal torque showed higher values for surface-modified zirconia implants than for the titanium implants inserted in the tibia and femur of rabbits.[14] There are currently few zirconia implant systems commercially available. Titanium implants with a coronal base in zirconia are also available, the aim of which is to combine the safety of titanium with the aesthetic features of zirconia.[3] Since the clinical use of zirconia implants lacks scientific support, prospective clinical investigations are needed before these implant systems can be recommended for clinical use.
Zirconia In Removable Prosthodontics
The use of zirconia for fabrication of a zirconia bar on implants and of a corresponding zirconia complete denture has also been reported.The technique utilizes a copy-milling unit, that is a manually operated machine for the manufacture not only of frameworks but also of complete removable dentures.[18]
Conclusions
In conclusion, Zirconia based restorations are a promising prosthodontic alternative to metal - based restorations and the biological, mechanical and clinical studies published to date seem to indicate that Zirconia restorations are both well tolerated and sufficiently resistant. Ceramic bonding , luting procedures, ageing and wear of zirconia restorations need to be further evaluated in order to guide the adequate use of this material. Appropriate patient selection, coupled with adequate clinical and technical protocols are imperative in order to obtain good performance of Zirconia restorations.
References
1. Raigrodski AJ. Contemporary materials and technologies for all-ceramic fixed partial dentures: a review of the literature. J Prosthet Dent. 2004 Dec;92(6):557-62.
2. Komine F, Blatz MB, Matsumura H. Current status of zirconia-based fixed restorations. J Oral Sci. 2010 Dec;52(4):531-9.
3. Manicone PF, Rossi Iommetti P, Raffaelli L. An overview of zirconia ceramics: basic properties and clinical applications. J Dent. 2007 Nov;35(11):819-26.
4. Guazzatoa M, Albakrya M, Ringerb S P, Swain M V. Strength, fracture toughness and microstructure of a selection of all-ceramic materials.Part II. Zirconia-based dental ceramics. Dental Materials (2004) 20, 449-456
5. Parker RM. Use of zirconia in restorative dentistry. Dent Today. 2007 Mar;26(3):114, 116, 118-9
6. Raigrodski AJ, Hillstead MB, Meng GK, Chung KH. Survival and complications of zirconia-based fixed dental prostheses: a systematic review. J Prosthet Dent. 2012 Mar;107(3):170-7.
7. Pilathadka S., Vahalová D., Vosáhlo T. The Zirconia: a New Dental Ceramic Material. An Overview Prague Medical Report / Vol. 108 (2007) No. 1, p. 5-12
8. Zarone F, Russo S, Sorrentino R. From porcelain-fused-to-metal to zirconia: clinical and experimental considerations. Dent Mater. 2011 Jan;27(1):83-96.
9. Sadowsky SJ. An overview of treatment considerations for esthetic restorations: a review of the literature. J Prosthet Dent. 2006 Dec;96(6):433-42.
10. Sailer I, Gottnerb J, Kanelb S, Hammerle CH. Randomized controlled clinical trial of zirconia-ceramic and metal-ceramic posterior fixed dental prostheses: a 3-year follow-up. Int J Prosthodont. 2009 Nov-Dec;22(6):553-60.
11. Thompson JY, Stoner BR, Piascik JR, Smith R. Adhesion/cementation to zirconia and other non-silicate ceramics: where are we now? Dent Mater. 2011 Jan;27(1):71-82.
12. Denry I and Holloway JA. Ceramics for Dental Applications: A Review. Materials 2010, 3, 351-368
13. Ozkurt Z, ?seri U and Kazazoglu E. Zirconia ceramic post systems: a literature review and a case report. Dental Materials Journal 2010; 29(3): 233-245
14. Kohal RJ, Att W, Bachle M, Butz F.Ceramic abutments and ceramic oral implants. An update. Periodontol 2000. 2008;47:224-43.
15. Gomes AL, Montero J. Zirconia implant abutments: a review.Med Oral Patol Oral Cir Bucal. 2011 Jan 1;16(1):e50-5.
16. Scarano A, Piattelli M, Caputi S, Favero GA, Piattelli A. Bacterial adhesion on commercially pure titanium and zirconium oxide disks: an in vivo human study. J Periodontol. 2004 Feb;75(2):292-6.
17. Kohal RJ, Klaus G. A zirconia implant-crown system: a case report.Int J Periodontics Restorative Dent. 2004 Apr;24(2):147-53.
18. Buhler NM, Teubner E, Marinello CP. Schweiz Monatsschr Zahnmed. Zirconia in removable prosthodontics. A case report 2011;121(7-8):659-78. |