Introduction
In 1895, German physicist Wilhelm Conrad Roentgen discovered the X-ray. Within two weeks after Roentgen made his discovery public, the first dental radiograph was made by German dentist Otto Walkoff, who placed in his own mouth small glass photographic plates wrapped in rubber dam and exposed them for 25 minutes, and henceforth emerged the field of Oral Radiology.[1] After about nine decades, Radiovisiography (RVG) marked the starting point of intraoral digital radiographic techniques in dentistry.
History
RVG was invented by Dr. Frances Mouyens, manufactured by Trophy Radiologie (Vincennes, France) in 1984 and described in the U.S. dental literature in 1989.[2] Dr. Mouyens invented a way to employ fiber optics to narrow down a large x-ray image onto a smaller size that could be sensed by a Charge Coupled Device (CCD) image sensor chip. Once the X-Ray imaging chip specifications were finalized, Trophy Radiologie contracted Fairchild CCD Imaging Company in Silicon Valley, California, USA to develop the actual CCD imaging chips. At Fairchild, a young Finnish physicist and CCD image sensor design engineer named Paul Suni, helped create the enabling CCD image sensor technology that was needed to make the RVG digital radiography system a reality. The first dental digital system was capable only of acquiring a radiographic image; the image could not be stored on disk but had to be printed. Shortly thereafter, another system was developed by Per Nelvig and colleagues (Sens-A-Ray, Regam Medical Systems, Sundsvall, Sweden), and within a decade many more manufacturers entered the market.[1]
Components Of Rvg
The RVG system is capable of rapidly displaying a digital radiographic image on a monitor which results in a lower patient radiation.[3] The "Radio" component is the conventional x-ray generator with a timer, capable of very short exposure time, along with image receptor. The "Visio" portion converts the output signal from a CCD to a digital format and displays it on a monitor. The "Graphy" component consists of data storage unit connected to a video printer.[4] (Figure 1). The most significant advantages of digital imaging, therefore, are computer aided image interpretation and image enhancement, in addition to the obvious options of standardized image archiving and image retrieval.
The CCD is a solid-state detector composed of an array of X-ray or light sensitive pixels on a pure silicon chip. A pixel or picture element consists of a small electron well into which the X-ray or light energy is deposited upon exposure. The individual CCD pixel size is approximately 40µ with the latest versions in the 20µ range. The rows of pixels are arranged in a matrix of 512 x
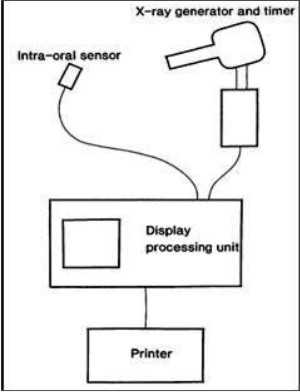 | Figure1- The total RVG system5
 |
512 pixels. There are two types of digital sensor array designs: area and linear. Area arrays are used for intraoral radiography, while linear arrays are used in extraoral imaging. Area arrays are available in sizes comparable to size 0, size 1, and size 2 films, but the sensors are rigid and thicker than radiographic film and have a smaller sensitive area for image capture. The sensor communicates with the computer through an electrical cable. Area arrays CCDs have two primary formats: fiberoptically coupled sensors and direct sensors. Fiberoptically coupled sensors utilize a scintillation screen coupled to a CCD. When X-rays interact with the screen material, light photons are generated, detected, and stored by CCD. Direct sensor CCD arrays capture the image directly without the intermediate scintillation layer.[3]
When exposed to radiation, the covalent bonds between silicon atoms are broken, producing electron whole pairs. The number of electron whole pairs that are formed is proportional to the amount of exposure that an area receives. The electrons are then attracted towards the most positive potential in the device, where they create "charge packets". Each packet corresponds to one pixel. The charge pattern formed from the individual pixel in the matrix represents the latent image. The image is read by transferring each row of pixel charges from one pixel to the next in a "bucket brigade" fashion. As a charge reaches the end of its row, it is transferred to a read out amplifier and transmitted as a voltage to analog-to-digital convertor located within or connected to the computer. Voltages from each pixel are sampled and assigned a numeric value representing a gray level.[6]
Image Formation
Data acquired by the sensor is communicated to the computer in analog form. Computers operate on the binary number system in which two digits (0 and 1) are used to represent data. These two characters are called bits (binary digit), and they form words eight or more bits in length called bytes. The analog-to-digital converter transforms analog data into numerical data based on the binary number system. The voltage of the output signal is measured and assigned a number from 0 (black) to 255 (white) according to the intensity of the voltage. The large number of gray values is reduced to 256 shades of gray with the advantage of controlling under or overexposed images.[2],[6]
Rvg Versus Conventional Imaging
1. Acquisition of images:
Film-based imaging consists of X-ray interaction with electrons in the film emulsion, production of a latent image, and chemical processing that transforms the latent image into a visible one. Based on the continuous density scale film-based images are called analogue images. The final result is a fixed image that is difficult to manipulate once captured.[2] Digital imaging is the result of X-ray interaction with electrons in electronic sensor pixels conversion of analog data to digital data, computer processing, and display of the visible image on a computer screen.
2. Rigidity:
The property of rigidity prevents distortion of the image, which is present in conventional imaging due to bending of the film intraorally. But this at the same time can be considered as a disadvantage as the rigidity may cause improper placement and pain to the patient.[7]
3. Radiation dose:
Radiation safety is an important issue in dental radiography. The desired amount of information must be obtained with the smallest possible amount of radiation. The dose per exposure is generally lower in digital intraoral radiography than in conventional film-based radiography.8 According to few articles the reduction in radiation offered by digital radiography is usually 70 to 80 percent, and at times even more-allows multiple periapical images for the same radiation exposure involved in a single periapical image obtained via conventional radiography.[7] This reduction in radiation is especially important in implant placement or difficult endodontic therapy, in which multiple images frequently are needed. Radiation exposure is reduced by 50% to 90% when compared with D-speed conventional film-based technology. The surface exposed with the CCD is approximately 50% less than what is exposed using film for a single image the total patient dose depends on the number of exposures required to cover the area.[9]
4. Image display:
The digital image is displayed on a monitor screen in much greater dimensions than the film image that is read on a viewing box. It allows for manipulation of the grey scale for variation in image presentation. Møystad et al demonstrated that high zooming sizes gave inferior detection levels of proximal caries and that one has to be aware of an upper limit of displayed image size.[10]
5. Image characteristics:
Brightness, contrast and many other image characteristics can be manipulated with digital radiographs, while contrast and density of a conventional radiograph is determined during the exposure and film processing procedure and cannot be corrected afterwards. Film displays higher resolution than digital receptors (6-10 lp/mm3) with a resolving power of about 16 lp/mm.2 The direct digital receptors have a wider dynamic range than that of film. Dynamic range or latitude is the range of exposures that will produce images within the useful density range.[2] Alternatively it is also defined as the range of exposures that result in a diagnostically acceptable image.[11] This reduces the number of retakes. Digital radiography allows the clinician to change contrast (to lighter or darker), enlarge images, place color enhancements or superimpose various textures on images. All of these changes of the original image facilitate easier detection of any pathosis that is present, and they also allow immediate and effective patient education.[7]
6. Working time:
In conventional radiographic techniques, the delay in reading the image usually forces the clinician to change gloves and do something else as the radiograph undergoes development. On returning to the patient, the clinician must wash his or her hands, don new gloves and reorient himself or herself to the clinical procedure at hand e.g.: endodontic therapy, implant surgery etc. RVG uses less time (0.5-2 min)[9] and manpower when compared to the conventional imaging (6 min).
7. Image storage , Image retrieval and Communication:
Pulling up specific stored radiographic images from a computer database is easy because of the highly organized nature of computer file storage. This form of storage also aids in electronic communication between dentists, which is made easier with digital networking. Also the patient education is highly improved and simplified with this modality. But the lack of universal use of digital imaging in the present scenario can be a hindrance to this form of communication.
8. Added features:
RVG also allows for perfect duplication of the images. It also facilitates the use of various tools for measurements of endodontic root length determination and for dental implant planning. (Figure 2)
 | Figure2- RVG image with measuring tool
 |
9. Cost of RVG:
RVG requires only an initial investment and eliminates the recurring expenses of film and processing solutions and hence at the same time eliminates the problem of disposal of spent solutions.
10. Initiation:
After receiving initial education to begin using digital radiography, one also has to upgrade the software from time to time.
11. Problems with Sensors:
With wired sensors, the presence of a wire attached to the sensor allows immediate observation of the image but initially the clinician needs to work around the wire. Careful handling of the sensor is paramount as breakage of the sensor can significantly affect the image quality.
12. Infection Control:
One and the same digital image receptor will be used in a dental clinic for years for all patients who need to have a radiograph, in contrast to film packages where a new package is used for every radiograph that is made. Therefore digital image receptors should be covered to prevent cross contamination.
13.Questionable use as an evidence in medico-legal case:
Currently juries view radiographs as photographs i.e., real evidence offered for jury inspection. Since a digital radiograph can be altered or manipulated, it is questionable whether digital radiograph can be used as legal evidence in a lawsuit. It is a possibility that digital radiographs can be manipulated to suggest pathological conditions when no pathology exists. Water marking a digital radiograph can prevent this manipulation to an extent.[12]
Generations Of Radiovisiography:
The First Generation:
The first commercial generation of the RVG, was introduced in Europe in 1987. It provided a basic grey scale image display without image processing capabilities.
The Second Generation:
The second generation included software driven central processing unit. Due to insufficient memory for storage and display of full resolution images, a four-to-one pixel averaging compression was utilized for display. Furthermore, the display reduced the internal 8-bit capacity to 6-bit.[13]
The Third Generation:
The third generation, RVG 32000 incorporated modifications which increased the sensitivity and dose dynamics of the sensor. In this model, the sensor was sealed and colour coded to indicate the X-ray sensitive side. It also provided image enhancement features including gradient contrast adjustment and black/white reversal, but added a steep gradient enhancement with only 8 grey levels displayed and the choice of full resolution image acquisition (high resolution zoom or ZHR). Only four 'normal' images or one ZHR image could be held in the RVG buffer without storage in an attached computer. Images were therefore printed using a thermal printer and archived as analogue 'hard copies'. The characteristics and diagnostic accuracy of this version of the RVG system reflected a reduction of two to three fold over the second generation. [13]
The Fourth Generation:
The fourth generation RVG-S has a more compact and ergonomic keyboard, a super VGA (video graphic array) colour monitor, a more powerful CPU and a more streamlined and visually presentable overall appearance. Twenty images can be stored in the buffer without down loading to the storage device. The personal computer based version (RVG-PC) includes a sensor, image acquisition board and application software which allows image capture and acquisition by any 386 or 486 IBM personal computer. Versions are now available which allow the use of any X-ray generator. These are designated by the suffix i (for example, RVG-PCi). The fourth generation RVG had an option of automatic exposure compensation (AEC), which compensated for exposure errors by stretching the pixel value range to increase the contrast of structures within the images.[13]
The Fifth Generation:
RVG-ui and the Dexis are the examples of this generation. The RVG-ui is a solid-state system for dental x-ray imaging combining a CCD of small pixel size (19.5µ) with a caesium iodide scintillator. It features two sizes of sensor with receptive areas that approach the size of No. 1 and No. 2 periapical x-ray films. The spatial resolution of the RVG-ui exceeds 20 lp/mm, rivaling conventional intra-oral x-ray film when the latter is optimally exposed and processed.[14]
The Sixth Generation:
The RVG 5000 System incorporates innovative KODAK sensor technology, the RVG 5000 System combines the best attributes of CCD and CMOS (Complementary Metal Oxide Semiconductor) sensors in a single component, allowing for the capture of high-quality radiographs at exceptional speed. It features excellent contrast perceptibility to support high standards of diagnostics and patient care.
The Seventh Generation:
KODAK RVG 6100 have rounded corners which help make the sensor more comfortable for patients. It has also introduced a new size 0 sensor for pediatric examinations and shock absorbing material protects the sensor from damage. It's fiber optic technology provides high resolution digital images enabling clinicians to make swift and accurate diagnoses. The system also employs a sensor remote control, allowing clinicians to capture and display images chair-side in less than two seconds.
Clinical Applications
A filmless environment allows rapid image acquisition, less expensive storage, multiple viewing, and remote exchange of images. Development of a filmless environment also facilitates the teaching and research responsibilities incumbent in an academic environment. Electronic teaching files, electronic conferences, teleconsultation, and other communication processes are enabled with the availability of electronic images.
1) Dental Caries Detection:
Digital intra-oral radiography seems to be as accurate as current dental films for the detection of caries in general. Only very few out of a relatively high number of in vitro studies have found the opposite. Sensitivities are fairly high (0.6 - 0.8) for detection of occlusal lesions extending into dentine.[15]
Computer aided diagnosis, is a unique software tool, developed to assist dentists in the difficult task of diagnosing radiographs for proximal caries. The software, called Logicon Caries Detector (Northrop Grumman Information Technology, Herndon), extracts image features and correlates them with a database of known caries problems. A study conducted by Gakenheimer (2002)[16], who used Logicon Caries Detector with RVG, found that the software enabled dentists to find 20% more cases of caries penetrating into dentin than they were able to find without it. Another study conducted by Navarro et al., (2008)[17], found that the application of the Logicon program increased sensitivity, especially in lesions with caries extending into the dentin. In contrast, conventional radiography yielded a higher specificity and positive predictive value. The negative predictive values were similar for both techniques.
2) Intrabony defects:
Talaiepour et al., (2005)[18] , conducted a study with an aim to evaluate the accuracy of RVG in the linear measurement of interproximal bone loss in intrabony defects and concluded that radiographic assessment by either the Cemento-Enamel-Junction or occlusal references overestimated bone loss as compared to the intrasurgical gold standard. Similarly Khocht et al., (2003)[19], compared bone levels from direct digital and conventional radiographic and found that digital radiographs showed a higher number of sites with bone loss than did conventional radiographs.
3) Periapical pathologies detection:
Versteeg et al., (1998)[20], found that 6% of dental films required retakes compared with 28% with the sensor. Hence it was concluded that periapical radiography with a CCD sensor leads to more errors and thus more retakes than conventional film. Sullivan et al., (2000)[21], conducted a study to compare the variable sized periapical lesions created in vitro in human jaws by the means of different bur sizes and concluded that conventional radiography tended to be more accurate in the no lesion condition, whereas RVG using variable contrast was somewhat more accurate in the smallest lesion condition.
Stavropoulos et al., (2007)[22] conducted a study to compare the accuracy of cone beam CT scanning (NewTom 3G) with intraoral periapical radiography (Dixi2, Planmeca CCD sensor and Insight film) for the detection of periapical bone defects. NewTom 3G was statistically, significantly better in terms of sensitivity (54%), positive (82.6%) and negative (44.5%) predictive values, and diagnostic accuracy (61%) when compared with digital radiographs (23%, 60%, 31%, 39%), and with conventional ones (28%, 70%, 35%, 44%)- except in the positive predictive value. Specificity was similar for all three methods. No difference was observed between the two periapical (digital vs conventional) radiographs. NewTom 3G may be useful in cases of immediate implants intended to replace teeth with suspicion for possible existing endodontic pathology, or in candidate implant sites neighboring such teeth.
4) Detection of root fractures:
Kositbowornchai et al., (2001)[23], compared the diagnostic potential of direct digital radiography with conventional film for detecting experimental root fractures and concluded that the performance of CCD-based digital radiography in detecting root fractures is similar to film-based radiography.
5) Detection of root canal lengths:
Pace et al., (2005)[24], carried out a comparative analysis of the visualization of small files using digital and conventional radiographs and found no significant differences between the results of the two systems studied.
6) Application in mentally retarded/developmentally disabled individuals:
Severely and profoundly mentally retarded and developmentally disabled patients are unable to communicate disease symptoms, and radiographic examinations are often difficult to perform on non-sedated patients. Solid-state intraoral X-ray detectors have several advantages over traditional films, namely that they result in: (1) an instant image to assess the adequacy of exposure, beam alignment and detector placement; (2) increased quantum efficiency permitting a significant radiation dosage reduction per exposure; (3) the ability to enhance low signal images to permit minimization of dose whilst producing a radiograph of diagnostic density; and (4) the attachment of the detector to a fixed cable making ingestion or inhalation of the device less likely than with unattached film packets. In a study by Farman et al., (2003)[25] , it was concluded that 91% of images by RVG were excellent to satisfactory in diagnostic quality and a majority of patient's treatments were modified because of the radiographic information.
7) Telemedicine
The practice of remote consultation in such institutions is referred to as telemedicine. Telemedicine serves as a model for delivery of health care to sites where the health care provider and recipient are not present simultaneously at the same location. Although there are various designs and implementations of telemedicine, the common requirements for a successful scenario are providing a (1) sufficient and (2) reliable and secure set of (3) data in a (4) timely manner. These four requirements are key issues for ensuring the same quality of care as a conventional clinician-patient interaction, driving clinical acceptance of telemedicine. The sufficiency of data is a function of several parameters, such as the case under investigation and prior knowledge and experience of the clinician with the patient or disease.[26]
Conclusion
Practitioners have four distinct choices regarding digital x-ray imaging integration, that is to stay Analog only, Hybrid (both digital system and analog films), Completely filmless (digital imaging, but not integrated with a digital practice management system) and Completely digital.[27] The advantage of a digital dental practice are improved efficiency and management of all clinical, administrative and communication practice applications. The disadvantages are the capital costs and ongoing maintenance and training costs. Therefore the future is moving towards computerized and digitalized work environment and if one does not adapt to the change, then one faces obsolation.
References:
1. Vanderstelt PF. Radiography in dental practice. Filmless imaging: The uses of digital. J Am Dent Assoc 2005;136;1379-1387.
2. Parks ET, Williamson GF. Digital Radiography: An overview. J Contemp Dent Pract 2002; 3(4): 23-39.
3. Macdonald R. Digital imaging for dentists. Australian Dental Journal 2001; 46:(4):301-305.
4. Weathers K. RadioVisioGraphy Comes of Age. Practical Endodontics 1993; January: 1
5. Walker A, Homer K, Czajka J, Shearer C, Wilson NHF. Quantitative assessment of a new dental imaging system. The British Journal of Radiology1991; 64:529-536.
6. White SC and. Pharoh MJ. Oral Radiology Principles and Interpretation, 6th ed, Elsevier Inc, Missouri, 2009, pp.78-99.
7. Christensen GJ. Why switch to digital radiography? J Am Dent Assoc 2004; 135:1437-39.
8. Berkhout WER, S anderink GCH and VanderStelt PF. Does digital radiography increase the number of intraoral radiographs? A questionnaire study of Dutch dental practices. Dentomaxillofacial Radiology 2003; 32: 124-127.
9. LuskLT. Comparison of Film-Based and Digital Radiography. Practical Hygiene 1998; March/April:45-50.
10. Haak R , Wicht MJ, Nowak G and Hellmich M. Influence of displayed image size on radiographic detection of approximal caries. Dentomaxillofacial Radiology 2003; 32: 242-246.
11. Petrikowski CG. Introducing Digital Radiography in the Dental Office: An Overview. J Can Dent Assoc 2005; 71(9):651.
12. Calberson FLG, Hommez GM, and De Moor RJ. Fraudulent Use of Digital Radiography: Methods To Detect and Protect Digital Radiographs. J Endod 2008; 34:530 -536.
13. Scarfe WC, Farman AG, Brand JW, Kelly MS. Tissue radiation dosages using the RVG-S with and without niobium filtration. Australian Dental Journal 1997; 42(5):335-42.
14. Farman AG, Farman TT. RVG-ui: a sensor to rival direct- exposure intra-oral x-ray film. Int J Comput Dent.1992; 2(3):183-96.
15. Wenzel A. Digital radiography and caries diagnosis. Dentomaxillofacial Radiology 1998; 27: 3-11.
16. Gakenheimer DC. The efficacy of a computerized caries detector in intraoral digital radiography. J Am Dent Assoc 2002;133;883-890.
17. Navarro LF, Llena Puy MC, Godoy FG. Diagnostic performance of radiovisiography in combination with a diagnosis assisting program versus conventional radiography and radiovisiography in basic mode and with magnification. Med Oral Patol Oral Cir Bucal. 2008; 13(4): 261-5.
18. Talaiepour AR, Panjnoush M, Soleimanishayeste Y, Abesi F, Sahba S. A Survey on the Accuracy of Radiovisiography in the Assessment of Interproximal Intrabony Defects. Journal of Dentistry, Tehran University of Medical Sciences, Tehran, Iran 2005; 2(1):29-32.
19. Khocht A, Janal M, Harasty L, Chang KM. Comparison of direct digital and conventional intraoral radiographs in detecting alveolar bone loss. J Am Dent Assoc 2003; 134: 1468-75.
20. Versteeg CH, Sanderink GCH, van Ginkel FC and van der Stelt PF. An evaluation of periapical radiography with a charge-coupled Device. Dentomaxillofacial Radiology 1998; 27:97 - 101.
21. Sullivan JE, DiFiore PM and Koerber A. Radiovisiography in the detection of periapical lesions. Journal of Endodontics 2000; 26(1):32-35.
22. Stavropoulos A & Wenzel A. Accuracy of cone beam dental CT, intraoral digital and conventional film radiography for the detection of periapical lesions. An ex vivo study in pig jaws. Clin Oral Invest 2007; 11:101-106.
23. Kositbowornchai S, Nuansakul R, Sikram S, Sinahawattana S and Saengmontri S. Root fracture detection: a comparison of direct digital radiography with conventional radiography. Dentomaxillofacial Radiology 2001; 30: 106-109.
24. Pace SRB and Habitante SM. Comparative analysis of the visualization of small files using digital and Conventional radiography. J Appl Oral Sci 2005; 13(1): 20-3.
25. Farman AG, Horsley B, Warr E, Ianke JL and Hood H. Outcomes of digital X-ray mini-panel examinations for patients having mental retardation and developmental disability. Dentomaxillofacial Radiology 2003; 32: 15-20.
26. Analoui M and Buckwalter K. Digital radiographic image archival, retrieval, and management. Dental Clinics of North America2000; 44(2):339-358.
27. Wenzel A, Moystad A. Work flow with digital intraoral radiography: a systematic review. Acta Odontol Scand. 2010 Mar; 68(2):106-14. |