|
|
|
| Methods Of Oral Cancer Detection - A Review |
Sunint Singh 1 , Mohit Bansal 2 , Urvashi Kukreja 3 , Shelja Vashisth 4
1 Lecturer, Department of Prosthodontics - Swami Devi Dyal Hospital & Dental College, Barwala, Distt. Panchkula, India.
2 Lecturer, Department of Public Health Dentistry, - Swami Devi Dyal Hospital & Dental College, Golpura, Barwala, Distt. Panchkula.
3 Senior Lecturer, Dept. of Prosthodontics, - MM College of Research and Dental Sciences, MM University (Mullana- Ambala)
4 Lecturer, Dept of Public Health Dentistry - Swami Devi Dyal Hospital & Dental College, Golpura, Barwala, Distt. Panchkula, India.
|
| Address For Correspondence |
Address For Correspondence:
Dr. Sunint Singh
House no. 2309, sector 48-C,
Astha Apartments, Chandigarh, 160047
Mobile- +919780928528
Email: sunintsingh@gmail.com |
| Abstract |
| Abstract
Most cancers of the oral cavity are oral squamous cell carcinomas (OSCC) accounting more than 95% of the oral cancers. The main etiology behind this is tobacco and other associated factors. Hence, the detection of oral cancer at an early stage, when it is most amenable to treatment is an important goal for the dental profession. It is the most effective means to improve the survival rate and reduce the morbidity. However it is generally accepted that prevention and screening of oral cancer are equally important. |
|
| Keywords |
| Key Words
Oral cancer, etiology, treatment, screening. |
|
| Full Text |
Introduction
Oral cancer is classically described as an ulcerated, indurated lump or sore that may or may not be associated with pain and often involves the regional lymph nodes. It is the sixth most common cancer in the world affecting 3,89,000 people each year. Oral cancer has a poor 5 year survival rate of 50% or less. The annual incidence of oral cancer in the United States is approximately 30,000 new patients, with close to 9,000 deaths per year [1].
Oral cancer is associated with chronic irritating factors such as tobacco, smoking, alcohol, and betel quid (BQ) use. While cigarette smoking and alcohol drinking are the major risk factors in Western countries, BQ use and smoking are major factors in the causation of oral cancer in South Asia, Southeast Asia and Taiwan relatively high prevalence of oral cancer in Taiwan is mainly because there is a high-risk group of 2.5 million people with the habits of smoking and betel nut chewing. Tobacco is the second major cause of death in the world and currently responsible for death of one in every ten adults worldwide. Oral mucosa diseases such as leukoplakia, oral submucous fibrosis, oral precancer lesions and oral cancer have been strongly associated with the use of BQ[2]. In India, about 5 million people suffer from this disease[3]. According to the WHO estimates, 194 million men and 45 million women use tobacco in smoked or smokeless forms in India[4]. Indians form the second largest consumer of tobacco and consume it in forms of bidi, gutka, khaini, paan-masala, hukka, cigarettes, chillum, chutta, gul, mawa, mishri and others[5]. In India, tobacco use is estimated to cause 0.8 million deaths annually. The World Health Organization predicts that tobacco deaths in India may exceed 1.5 million annually by 2020[6].
Methods Of Examination Of Oral Cancer [7]
There are many reports on the miscellaneous methods of oral cancer detection and screening. Physical examination includes self-examination and clinical examination. Clinicians have a responsibility to perform a thorough head and neck examination as part of the physical assessment of their patients. The goal of examination is to detect any nodules, swellings, mucosal alterations (ulcerations, textural or color changes) and unexplained neck lymph nodal adenopathy. While many routines exist for an oral examination, each clinician must develop his or her own method, use it in all patients, and carefully document positive findings.
Components Of Oral Cancer Examination [8]
1) Health history- Well prepared medical and dental history provides information to the examiner about the etiology and other risk factors causing oral cancer. This has a limitation that the patient can give wrong history or the examiner can under assess the patient's risk of oral cancer especially in cases where the patient has recently stopped using tobacco products.
2) Visual examination- Direct visualization of the mucosal surfaces is vital in detecting the cancer. To optimize the clinician ability to identify surface changes, the mucosal surfaces need to be dry and viewed under good illumination.
3) Palpation- It is significant for detection of primary lesions that are not readily visible. A lesion that appears superficial may be found upon palpation to be infiltrative and deep, suggesting a more extensive tumour.
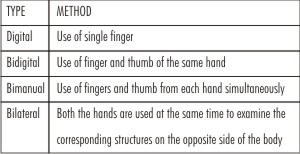
Types of palpation-
 |
 |
1) Examination of Face, Head and Neck-
Method - Visual Examination
Warning Sign- Asymmetry, colour and textural skin changes, strained breathing and facial paralysis.
2) Temporomandibular Joint (TMJ)-
Method- Place the fingers bilaterally just anterior to the tragus of ears. Have the patient open and close mouth several times and while the jaw is open move it from side to side and forward. Listen and feel the joints.
Warning signs- TMJ dysfunction. Normally the movements should be smooth, continuous and sound free, bilaterally symmetrical and should be free from pain.
3) Lips-
Method- Evert the lower lip so that the gingival and muccobuccal fold is visible. Dry the area with a gauge piece. Palpate with thumb and finger systematically from one side to the other.
Warning sign- Any change in colour, any lesion on the vermillion border and mucosal surface.
4) Labial and alveolar mucosa-
Method- Invert the labial tissue. Dry it with s gauge piece and inspect the mucosa. Palpate the labial mucosa using bilateral compression. Palpate the alveolar and gingival mucosa using digital compression.
Warning signs- Traumatic lesions, abrasions, tobacco pouch.
5) Buccal mucosa-
Method- Retract the cheek. Reflect light to inspect the mucosa from commissure to retromolar area. Use mouthmirror to inspect posterior area. Palpate with the thumb and first finger bimanually.
Warning signs- Any traumatic lesion, tobacco associated lesion, lichen planus, leukodaema.
6) Hard and soft palate and alveolar ridge-
Method- Patient is advised to tilt his head back. Use light to visualise the area.
Warning signs- Discolouration, patachiae, nicotine stomatits, abscesses.
7) Tongue-
Method- Inspect the dorsum of the tongue. Ask the patient to move the tongue side by side. Palpate the lateral borders and lingual tonsils. Inspect the vertical surface of the tongue also.
Warning signs-Papilla changes, swelling, mucosal lesions.
8) Floor of mouth-
Method- Ask the patient to touch the palate with the tip of the tongue. Palpate bimanually with one finger intraorally.
Warning signs-Enlargement, gland blockage, tenderness.
Identification Of Findings [9]
Changes in colour, symmetry, size, contour, need to be reviewed with a high degree of suspicion and is thoroughly evaluated. The suspicion area is then palpated to access the extent of invasiveness.
After palpating the area, the palpable sources of initiation should be removed. The patient should be reevaluated fro atleast 10 days to two weeks. If the lesion or the cause resists fro 10-14 days, then the diagnosis should be done. The various diagnostic aids such as biopsies, cytology brushes, toludine blue tests can be done to confirm the possibility.
Latest Diagnostic Tools For Detection Of Oral Cancer -
1) Vital Staining- Toluidine blue staining is a simple method, with the dye having an affinity to cancer cells. Commercial kits (Ora Screen) with protocol are available for large-scale screening of high-risk populations or in clinical patients by topical application or mouth rinsing. However, a significant percentage of false-negatives and false-positives exist. To overcome this drawback another staining kit Ora Test TM has been introduced which can clearly specify the oral dysplastic lesion [10].
2) Chemilumincence- Vizilite TM a new kit which is used to identify, evaluate and monitor white lesions [11]. The normal tissue will absorb the light and appear dark with blue hue while the abnormal tissue will appear white. This can only enhance visualization of intra oral white lesions but cannot distinguish between oral malignancies and malignant oral lesions [12].
3) Autofluorescence- VELSCOPE (Visually Enhanced Lesions Scope) an hand held device uses the principle of fluorescence for direct visualization of oral lesions. The normal tissue emits pale green fluorescence while the affected tissue appears dark green or black in color [13].
4) Cytopathology- Cytopathology is the microscopic study of cell samples collected from mucosal surfaces (via smears, scrapings or lavage) or from internal sites via fine-needle aspiration. The OralCDx Brush Test system uses a specialized brush that collects transepithelial cellular samples composed of free cells and clusters. These samples are fixed onto a glass slide and sent to a laboratory where they are stained (via a modified Papanicolaou technique), scanned and analyzed microscopically by means of a computer based imaging system that can rank cells on the basis of degree of abnormal morphology. A cytopathologist interprets the computerized results. Results are reported as "negative or benign," "positive" or "atypical." Abnormal OralCDx diagnoses have included "positive" defined as definitive cellular evidence of epithelial dysplasia or carcinoma) and "atypical" (defined as abnormal epithelial changes of uncertain diagnostic significance) results. Advantage of this technique is minimum discomfort and no bleeding [14].
5) Biopsy- The gold standard diagnostic test for oral mucosal lesions that are suggestive of premalignancy or malignancy remains tissue biopsy and histopathological examination. Biopsy procedure is carried out by a dentist who is well qualified in recognising potential of the lesion and is capable of obtaining appropriate and adequate biopsy [15].
Types of biopsy [16]
1. Excisional biopsy- A whole organ or a whole lump is removed (excised). Some types of tumours (such as lymphoma, a cancer of the lymphocyte blood cells) have to be examined whole to allow an accurate diagnosis, so enlarged lymph nodes are good candidates for excisional biopsies.
2. Incisional biopsy- Only a portion of the lump is removed surgically. This type of biopsy is most commonly used for tumours of the soft tissues (muscle, fat, connective tissue) to distinguish benign conditions from malignant soft tissue tumours, called sarcomas.
3. Fine needle aspiration cytology- This is an extremely simple technique that has been used in Sweden for decades but has only been developed widely in the US over the last ten years. A needle no wider than that typically used to give routine injections (about 22 gauge) is inserted into a lump (tumour), and a few tens to thousands of cells are drawn up (aspirated) into a syringe. These are smeared on a slide, stained, and examined under a microscope by the pathologist. Tumours can especially be diagnosed for FNA, as the only other way to sample them is with major surgery. Such FNA procedures are typically done by a radiologist under guidance by ultrasound or computed tomography (CT scan) and require no anaesthesia, not even local anesthesia.
4. Punch biopsy- This technique is typically used by dermatologists to sample skin rashes and small masses. After a local anesthetic is injected, a biopsy punch, which is basically a small (3 or 4 mm in diameter) version of a cookie cutter, is used to cut out a cylindrical piece of skin. The hole is typically closed with a suture and heals with minimal scarring.
5. Imaging- It includes
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
Computed tomography (CT)- CT has recently reached a new level of technological capability. With the development of faster detectors and helical mode scanning modern city scanners are capable of 1-2 scan times per slice or less permitting an entire study of neck or brain. The CT image is the computer generated cross-sectional representation of anatomy created by analysis of attenuation of X-ray beams pass through various points across the section of the body. Greater attenuation of X-ray by structures such as bone results in the areas of high density while soft structures that attenuate X-ray beam to a lesser degree appear as low density. A typical modern CT scanner is capable of obtaining 1-2, 5-10 ml thick sections 1-3 sec/section. Helical CT, recent development in CT technology produces 3-D CT information. A CT examination of head and neck requires rapid administration of intravenous iodinated contrast material, during scanning to differentiate vascular structures from lymph nodes. CT scan has an advantage of fast scan times and has great improved imaging of oral cavity and neck [17].
MRI technique - This technique continues to evolve as a reliable alternative for imaging head and neck anatomy and pathology. Each MRI image should include a T1 wait image which demonstrates normal anatomy with detail and soft tissue definition and T2 wait images which demonstrate tumor in comparison to adjacent muscle and soft tissues. MRI allows more accurate distinction between tumor and benign inflammatory disease. Small part ultra sonography may be of value for imaging salivary gland masses and for assessment of lymph nodes [18].
Conclusion
Early detection of high risk patients through oral examination and maintaining high risk of suspension are the basic three strategies which a dentist can apply in controlling oral cancer. By adopting one of these methods, one can diagnose and treat the lesion at an initial stage. Besides this one should do de- addiction counselling which would not only help the patients to stop his tobacco habit but also aids in maintaining strong patient-dentist relationship. Therefore the dentist must have a thorough knowledge of the precancerous lesions and conditions.
References
1) Donnell A, Jin S, Zavras A I. Delay in the diagnosis of oral cancer. J Stomatol Invest 2008; 2 (1):15-26
2) Pindborg JJ, Murti PR, Bhonsle RB, et al. Oral submucous fibrosis as a precancerous condition. Scand J Dent Res 1984; 92: 224-9.
3) Chiu CJ, Chang ML, Chiang CP. Interaction of collagen-related genes and susceptibility to betel quid induced oral submucous fibrosis. Cancer Epidemiol Biomarkers Prev 2002; 11: 646-53.
4) Sinha, D.N., Gupta, P.C., & Pednekar, M.S. Tobacco use in a rural area of Bihar, India. Indian J Commun Med 2003; 28: 167-70.
5) Rani, M., Bonu, S., Jha, P., Nguyen, S.N., & Jamjoum L. Tobacco use in India: Prevalence and predictors of smoking and chewing in a national cross sectional household survey 2003, 12th ed. Tobacco Control.
6) Murray, C J L and Lopez A D. Alternative projections of mortality and disability by cause 1990-2020: Global burden of disease study. Lancet; 349, 9064: 1498-1504.
7) CS Farah, MT Cullough. Oral cancer awareness for general practioners; new approaches to patient care. Australian Dental Journal 2008; 53: 2-10.
8) Burkitt's: Oral Medicine- Diagnosis and Treatment. 10th edition. Caepsons paper Ltd; Noida: 194-235.
9) Scott SE etal. Patient delay for potentially malignant oral symptoms. European Journal Sciences 2008; 116: 141-7.
10) Scully C, Hopper C. Oral cancer current and future diagnostic techniques. American Journal Dentistry 2008; 21: 199-209.
11) Epstein JB, Gorsky M, Lonky S, Silverman S Jr, Epstein JD, Bride M: The efficacy of oral lumenoscopy (ViziLite) in visualizing oral mucosal lesions. Spec. Care Dentist2006; 26(4): 171-4.
12) Kerr AR, Sirois DA, Epstein JB: Clinical evaluation of chemiluminescent lighting: an adjunct for oral mucosal examinations. J. Clin. Dent 2006; 17(3): 59-63.
13) Natarajan E. Contemporary Concepts in the Diagnosis of Oral Cancer and Precancer. Dental Clinics of North America; Ellen Eisenberg; 55 (1): 63-88.
14) Hall DL. Oral Brush Biopsy Technique Instruction Outcomes for Senior Dental Students. Journal of Dental Education 2006; 70(8): 820-25.
15) Crispton Sculty. Oral and Maxillofacial Medicine : The basis for Diagnosis and Treatment; Elseveir Publications: 231- 52.
16) Kao SY, Cau YW etal. Detection of screening and precancerous lesions. Journal of Chinese Medical Association 2009; 72(5): 227-33.
17) Available from : http://www.ndted.org/EducationResources/computedtomography. html. [last accessed on 2011 Dec 17]
18) Available from : http://www.netdoctor.co.uk/health_advice/examinations/mriscan.html. [last accessed on 2011 Dec 17] |
|
|
|
|
|
|