Introduction
Dentinal hypersensitivity is a common painful condition of the teeth. It is associated with exposure of dentine due to loss of enamel by processes such as abrasion, erosion or denudation of the root surface by gingival recession or periodontal treatment.
Dentinal hypersensitivity has been shown to peak in 20 to 30 year olds and rise again when in their 50s. The condition generally involves facial surfaces of teeth near the cervical aspect. Patients undergoing periodontal treatment are particularly susceptible to this condition because of recession following periodontal surgery or loss of cementum following non-surgical periodontal therapy.[1]
It has become essential that the clinicians understand the cause, the diagnosis and the management of the condition. Dentinal hypersensitivity has been extensively researched through the years and many authors express an agreement that dentinal hypersensitivity is either under-reported by the dental patient population or misdiagnosed. This review aims at building a better understanding of the condition and thereby, providing a more comprehensive care to the patient.
Definition And Etiology
Dentinal hypersensitivity is defined as pain arising from exposed dentine typically in response to thermal, chemical, tactile or osmotic stimuli.[2]
Dentine may become exposed via several means:
The most common clinical cause for exposed dentinal tubules is gingival recession[3], which in turn may be caused by:
1. Inadequate attached gingiva
2. Prominent roots
3. Toothbrush abrasion
4. Pocket reduction periodontal surgery
5. Oral habits resulting in gingival laceration, i.e., traumatic tooth picking, eating hard foods
6. Excessive tooth cleaning
7. Excessive flossing
8. Gingival loss secondary to specific diseases, i.e., NUG, periodontitis
9. Crown preparation
Other causes include[4]:
1. Loss of enamel
2. Denudation of cementum
3. Attrition
4. Abrasion
5. Abfraction
6. Erosion (intrinsic and extrinsic)
7. Thinning, fenestration, absent buccal alveolar bone plate
8. Bleaching[5]: occurs as a result of a reversible pulpitis that is caused by the flow of dentinal fluid from osmolarity changes in the pulp. These changes occur when the bleaching material rapidly penetrates enamel and dentin to the pulp. Usually higher concentrations of peroxide results in a greater degree of sensitivity.
9. Scaling and rootplaning[5]: Removes 20-50µm of cementum and expose the dentinal tubules to a variety of stimuli. Von Troil et al found 50% of patients undergoing scaling and root planing had dentine hypersensitivity after treatment.
Once dentinal tubules become exposed, there are often oral processes or habits that keep them exposed[3]:
1. Poor plaque control, i.e., acidic bacterial byproducts
2. Excess oral acids, i.e., sodas, fruit juice, swimming pool chlorine, bulimia
3. Cervical decay
4. Toothbrush abrasion
Theories For Dentinal Hyper sensitivity [2]
Odontoblastic transduction theory
According to this theory, odontoblastic processes are exposed on the dentine surface and can be excited by a variety of chemical and mechanical stimuli. This causes the release of neurotransmitters and impulses are transmitted towards the nerve endings. However, no such neurotransmitters have been found to be produced or released by odontoblastic processes.
Neural theory : This concept advocates that thermal, or mechanical stimuli, directly affect nerve endings within the dentinal tubules through direct communication with pulpal nerve fibres. Although observations like the presence of unmyelinated nerve fibres in the outer layer of root dentine and the presence of putative neurogenic polypeptides support this theory, it is still considered theoretical with little solid evidence to support it.
Hydrodynamic theory : Hydrodynamic theory proposed by Brannstrom and co-workers is the most widely accepted theory for dentinal hypersensitivity. This theory postulates that fluids within the dentinal tubules are disturbed either by temperature, physical or osmotic changes and that these fluid changes or movements stimulate a baroreceptor which leads to neural discharge. The basis of this theory is that the fluid filled dentinal tubules are open to the oral cavity at the dentine surface as well as within the pulp.
Clinical Features : The teeth most commonly affected by dentinal hypersensitivity are the upper premolars followed by the upper first molars with the incisors being the least sensitive teeth.[6], [7], [8], [9], [10], [11], [12], [13]
It has been reported that there is a slightly higher incidence of dentine hypersensitivity in females compared to males.[6],[8],[9] This difference is, however, not statistically significant.[10]
The pain arising from dentinal hypersensitivity is extremely variable in character, ranging in intensity from mild discomfort to extreme severity. It may emanate from one tooth or several teeth and it is sometimes felt in all quadrants of the jaws.[14] Most patients describe the pain arising from dentinal hypersensitivity as being rapid in onset, sharp in character, and of short duration. The external stimuli eliciting dentinal pain can be thermal, osmotic, chemical, physical, or mechanical in nature. The thermal stimuli include hot and cold food and beverages and warm or cold blasts of air entering the oral cavity. Osmotic stimuli include sweet food and beverages. Acid stimuli include grapefruit, lemon, acid beverages, and medicines. Common mechanical stimuli are toothbrushes, utensils used for consuming food, and dental instruments.[14],[15]
Diagnosis
Following are the important points that have to be evaluated during the diagnosis of dentine sensitivity:
1. History and nature of the pain
2. Number and location of the sensitive teeth
3. Area of origin of sensitivity from tooth
4. Intensity of pain, frequency and duration of each episode
5. Triggering factor or stimulus for dentinal hypersensitivity
Differential Diagnosis
There are also a number of clinical conditions that may provide clinical features similar to that of dentinal hypersensitivity and it is important to distinguish between these in order to provide a correct diagnosis and successful management of the problem.[4] Clinical and radiographic examination is necessary to elucidate the cause.
These include:
Cracked tooth syndrome
Fractured restorations
Fractured teeth
Dental caries
Post-operative sensitivity
Acute hyperfunction of teeth
Atypical facial odontalgia
Palatal-gingival groove
Hypoplastic enamel
Congenitally open cementum-enamel junction
Improperly insulated metallic restorations
Assessment Of Dentinal Hyper sensitivity
Recommendations by Holland et al. [16] suggest that dentinal hypersensitivity may be evaluated either in terms of the stimulus intensity required to evoke pain (stimulus-based assessment), or as the subjective evaluation of the pain produced by a stimulus (response-based assessment).
Stimuli used to assess dentine hypersensitivity/ root dentine sensitivity in the clinical setting:
Mechanical (tactile) stimuli: In this, the dentinal surface is rubbed with either sharp tipped probe, mechanical pressure stimulators or Yeaple probe. In Yeaple probe, force variation is controlled by an electromagnetic device. Generally, a tooth is said to be non- sensitive when a force equivalent to 70g is reached without eliciting pain sensation.[17]
Chemical (osmotic) stimuli: In this, hypertonic solutions of glucose and sucrose are used, which creates osmotic pressure that induces intratubular fluid movement. A chemical stimulus for assessing dental hypersensitivity is not preferred, as the response obtained by this method is difficult to control. [17]
Electrical Stimulation: This is more complex and usually consists of progressive elevation of the magnitude of the stimulus until a slight sense of pain is felt. However, due to current loss through the periodontium and the subsequent stimulation of the periodontium, false positive results can occur. [17]
Cold air blast from a dental air syringe: An air current is applied for 1 second at a pressure of 45psi and at a temperature of 19-240C through dental chair. Air current technique is generally used for screening. [17]
Cold water testing: It is suggested to use a series of syringes containing water at different temperatures (between 0 and 200C), starting with the warmest water and gradually lowering the temperature. A gap of three minutes should be maintained before performing the next test at a lower temperature. The temperature of the water is decreased by 50C and the test is terminated when a painful response is recorded or when 00C is reached. [17]
Thermo-electric devices: A fine-tipped thermal probe is used in this method. It is placed on the surface of the tooth wherein heat or cold is continuously applied that allows quantification of the applied stimulus. The test is performed when temperature is 250C; subsequently the temperature is reduced by every 50C until the patient experiences the pain.
The other stimuli include:
Mechanical pressure stimulators
Scaling procedures
Single-tufted brush
Electrical pulp testers
Dental pulp stethoscope
Evaporative stimuli
Air jet stimulator
Temptronic device (microprocessor temperature-controlled air delivery system)
Thermal stimuli
Electronic threshold measurement device
Heat
Management Of Dentinal Hyper sensitivity
Review of literature on Dentinal hypersensitivity provides with a general guideline to be followed in the management of dentinal hypersensitivity. The various steps to be followed includes[4]:
History and examination to establish diagnosis
Identification of cause
Treatment based on severity of problem
Incorporation of preventive measures- remove etiological and predisposing factors Review the patient regularly for signs of attrition, abrasion, erosion, and abfraction
Give dietary advice in line with current thinking particularly in view of the potential effect of erosive materials (food and fizzy drinks) and brushing immediately after meals.
Give oral hygiene instruction and recommend an atraumatic toothbrushing technique to avoid potential damage to both hard and soft tissues
Mild generalized sensitivity-use of OTC desensitizing products (toothpastes, gels, etc)
Localized moderate to severe sensitivity-use of In-office products (primers, varnishes, sealants, etc)
Avoid placing subgingival restorations that may retain plaque
Avoid violating the biological width when placing crown margins
Use of periodontal flap surgery (including GTR) in the treatment of exposed root dentin
In severe cases, pulpal extirpation and extraction may be the treatment of choice
Review on an appropriate basis and reassess if pain persists
Treatment Strategies For Dentinal Hypersensitivity
Current techniques for treatment may be only transient in nature and results are not always predictable.[5] There are two main approaches for the treatment of dentinal hypersensititvity, namely,
(a) Tubule occlusion,
(b) Blocking nerve activity through direct ionic diffusion
The most common form of management is the placement of a topically applied agent applied either by a dental professional or by the patient at home.[2]
Self- applied treatments to reduce sensitivity consist of materials that occlude dentinal tubules, coagulate or precipitate tubular fluids, encourage secondary dentine formation, or obstruct pulpal neural response. It takes 2 weeks with twice a day usage to get a reduction in dentine sensitivity while using desensitizing toothpaste. Instead of having patients brush with the toothpaste, the paste could be placed in a soft tray to increase the contact time. Haywood et al recommended placing 5% potassium nitrate in bleaching trays to minimize sensitivity that may occur as a result of bleaching. The desensitizing toothpaste should not have sodium lauryl sulfate because a large amount of this ingredient may cause tissue irritation.[5]
The various methods for management of dentinal hypersensitivity include (Table 1)
1. Nerve desensitization
Potassium nitrate
2. Anti-inflammatory agents
Corticosteroids
3. Cover or plugging dentinal tubules
a) Plugging (sclerosing) dentinal tubules
Ions/salts
Calcium hydroxide
Ferrous oxide
Potassium oxalate
Sodium monofluorophosphate
Sodium fluoride
Sodium fluoride/stannous fluoride combination
Stannous fluoride
Strontium chloride
Protein precipitants
Formaldehyde
Glutaraldehyde
Silver nitrate
Strontium chloride hexahydrate
Casein phosphopeptides
Burnishing
Fluoride iontophoresis
b) Dentine sealers
Glass ionomer cements
Composites
Resins
Varnishes
Sealants
Methyl methacrylate
c) Periodontal soft tissue grafting
d) Crown placement/restorative materials
e) Lasers
Dentine Hypersensitivity: Restorative Considerations For Successful Management
A diagnosis of the cause of tooth sensitivity can be an abscessed or cracked tooth, dental decay or some form of hypersensitivity. Once the cause is determined, treatment options can be considered.
Options can be reversible or non- reversible or a combination of both depending upon the severity and extent of the condition[19] (Table 2)
Different conditions and their treatment options
Abscessed teeth, cracked teeth or dental caries: Removing the cause can involve endodontic therapy, extraction, root resection or apical surgery, or replacing the restoration and broken cusp.
Restoration: Preventing sensitivity can take the form of base placement ( such as vitrebond for thermal sensitivity) or sealing dentine tubules with a prime and bond system. Sensitivity can be reduced by cleaning the cavity preparation with a chlorhexidine solution to reduce bacterial insult, sealing tubules with a HEMA and gluteraldehyde material (eg. Gluma) or selecting materials that have no history of inducing this condition.[19]
Crown Cementation: Techniques which preclude over drying of the tooth where glass ionomer cements are employed may be helpful in avoiding sensitivity. Depending on the cement used, dentine tubules can be sealed under crowns with prime and bond, HEMA/ gluteraldehyde or simple copal varnish.
Occlusal trauma: Adjusting the occlusion or inserting a splint may be beneficial.
Cervical lesions from abrasion or abfraction : May require restorations for thermal protection
Composite restorations: Sensitivity is due to placement techniques and bulk cure of high polymerization shrinkage materials. The 'C' factor can help determine the potential for sensitivity and suggest a possible change in placement techniques to minimize the effects of polymerization shrinkage. Techniques that can minimize the chance for post operative sensitivity include; avoid bulk filling, placement of a stress breaker liner such as Optibond II or Vitrabond and soft start curing lights.
Abfraction lesions: May require adjustment of the occlusion followed by placement of a microfilled composite, which offers some flexibility with the tooth movement.
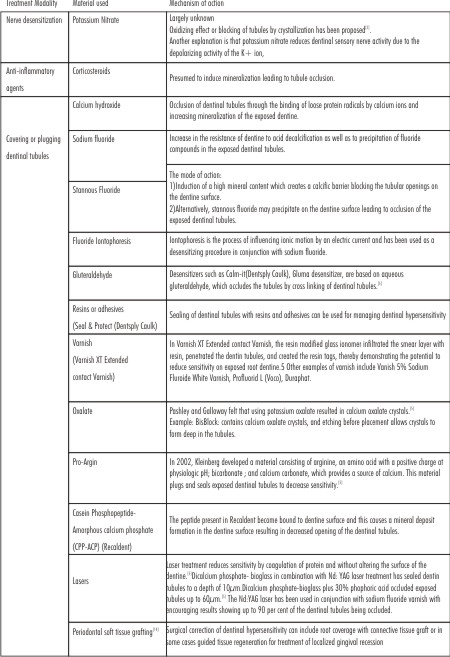 | Table 1
 |
Dental Hygiene And Periodontal Considerations In Dentine Hypersensitivity
Gingival recession resulting in exposure of dentinal tubules is the most common cause of dentine hypersensitivity. In periodontal patients, dentine hypersensititvity has been reported to be between 72.5-98.0 percent.
Genetic influence can play an important role in dentinal hypersensitivity since the presence of thin peridodontium and teeth that erupt outside the bony housing of the arch can result in fenestrations and dehiscence. Over time, this will result in areas that are more vulnerable to destruction of soft and hard tissues, which in turn result in hypersensitivity.
Other causes of gingival recession include a past history of periodontal therapy including scaling and root planing and pocket elimination surgery[18]. Literature shows that dentine sensitivity following scaling and root planing lasts for days to weeks . Sensitivity following periodontal surgery, particularly crown lengthening or pocket elimination surgery results in prolonged sensitivity that may last for months and require definitive treatment.
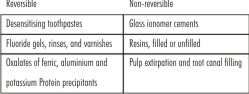 | Table 2
 |
Prevention Of Dentine Hypersensitivity [18]
Suggestions for Patients
Avoid gingival recession due to poor plaque removal by practicing good oral hygiene techniques
Avoid using large amounts of dentifrice, or reapplying additional dentifrice during brushing
Avoid hard bristled toothbrushes without end rounded bristles
Avoid brushing teeth immediately following ingestion of acidic food or beverages
Avoid over brushing with excessive pressure for prolonged periods of time
Avoid excessive flossing or incorrect use of other interproximal cleaning devices
Avoid 'picking' at the gums or using toothpicks inappropriately
Suggestions for Professionals
Avoid over instrumenting the root surfaces during calculus removal and scaling and root planing
Avoid over polishing the exposed roots during stain removal
Avoid violating the biologic width when placing crown margins causing subsequent recession
Avoid 'burning' the gingival tissue during in-office tooth whitening or bleaching procedures
Desensitizing Toothpaste
In clinical trials, the desensitizing effect of anti- sensitivity toothpaste generally takes about two weeks of application twice per day to show reduction in sensitivity, and greater effect develops with continued use.[19] Applying the desensitizing toothpaste in a tray for 10-30 minutes prior to the prophylaxis appointment has been reported to reduce discomfort during and after the procedure.[19]
Discussion
Evaluation of treatment is hampered by the lack of knowledge of the mechanism of dentine hypersensitivity, including its natural history and apparent tendency to natural desensitization by, as yet, hypothetical processes, the absence of clinical signs and the difficulty of accurately measuring the only symptom, namely pain.[15]
Occlusion of dentinal tubules appears to be of prime importance to desensitization. Uptake onto or into the dentine surface of treatment agents would, therefore, seem necessary.[15] Large number of very different compounds delivered by a variety of methods has been shown effective in the management of dentine hypersensitivity. Despite the considerable number of clinical studies, the apparent desensitizing effect of only a very few compounds, has been scientifically explained. Perhaps more importantly no single agent appears to fulfill the requirements suggested by Grossman (1935).[15]
Future research should attempt to fill in the considerable gaps in our knowledge of the interaction of specific compounds alone and in their varied formulations with dentine both in vitro and within the complex environment of the oral cavity.[15]
The expected increase in the longevity of dentition suggests that dentine exposure and the sometimes associated sensitivity will increase as a clinical problem. Consideration should be given now to preventing or reducing such dentine exposure. [15]
A proper co-ordination between the various specialities to assess and plan treatment strategies will help in addressing all causes and predisposing factors to reduce or eliminate the sensitivity.
Conclusion
The goal of treatment of dentinal hypersensitivity ideally should be the restoration of the original impermeability of the dentinal tubules and the relief of dentinal hypersensitivity experienced by the patient or at least to reduce the level of discomfort to enable the patient's quality of life to be maintained. The dental practitioner should be aware of the importance of a preventative strategy, particularly with a view to the removal of any etiological factors and minimizing the effects of erosion and altering the timing of tooth brushing relative to meals and snacks, etc.
There are many causes of and treatment for tooth sensitivity. The dentist must explore all possibilities, form a definitive diagnosis, then, implement management strategies that will help reduce or eliminate the sensitivity. Treatments may range from simple topically applied medicaments at home by the patient to restorations, pulp removal or mucogingival surgery.
The management of the condition should be based on the proper diagnosis and the severity of the condition. Practitioners should use their clinical judgment in determining the appropriate agent based on the severity of the condition and monitor the patient's progress over time within the constraints of the practice environment.
In future, gene therapy may be used to block the increased production of nerve growth factor (NGF) by pulpal fibroblasts near the lesion which are thought to contribute to tooth hypersensitivity after restorative procedures.[18]
References
1) Patricia A Walters. Dentinal hypersensitivity: A review. The Journal of contemporary dental practice. 2005;6(2)
2) PM Bartold. Dentinal hypersensitivity: a review. Australian Dental Journal 2006;51:(3):212-218
3) Peter L. Jacobsen, Gretchen Bruce. Clinical Dentin Hypersensitivity: Understanding
the Causes and Prescribing a Treatment. The journal of contemporary dental practice 2001;2:(1)
4) D.G. Gillam & R. Orchardson. Advances in the treatment of root dentine sensitivity: mechanisms and treatment principles. Endodontic Topics 2006, 13, 13-33
5) Richard D Trushkowsky, Anabella Oquendo. Treatment of dentin hypersensitivity. Dent Clin N Am 55(2011) 599-608.
6) Fischer C, Fischer RG, Wennberg A. Prevalence and distribution of cervical dentine hypersensitivity in a population in Rio de Janiero. Brazil. J Dent 1992;20:272-276.
7) Rees JS, Addy M. A cross-sectional study of dentin hypersensitivity. J Clin Periodontol 2002;29:997-1003.
8) Flynn J, Galloway R, Orchardson R. The incidence of "hypersensitive"teeth in the west of Scotland. J Dent 1985;13:230-236.
9) Orchardson R, Collins WJN. Clinical features of hypersensitive teeth. Br Dent J 1987;162:253-256.
10) Addy M, Mostafa P, Newcombe RG. Dentine hypersensitivity: the distribution of recession, sensitivity and plaque. J Dent 1987;15:242-248.
11) Rees JS. The prevalence of dentine hypersensitivity in general dental practice in the UK. J Clin Periodontol 2000;27:860-865.
12) Chabanski MB, Gillam DG, Bulman JS, Newman HN. Prevalence of cervical dentine sensitivity in a population of patients referred to a specialist periodontology department. J Clin Periodontol 1996;23:989-992.
13) Chabanski MG, Gillam DG, Bulman JS, Newman HN. Clinical evaluation of cervical dentine sensitivity in a population of patients referred to a specialist periodontology department: a pilot study. J Oral Rehab 1997;24:666-672.
14) Abel I. Study of hypersensitive teeth and a new therapeutic aid. Oral Surg Oral Med Oral Pathol 1958: 11: 491-495
15) Addy M, Dowell P. Dentine hypersensitivity - a review.II: clinical and in vitro evaluation of treatment agents. J Clin Periodontol 1983: 10: 351-363
16) Holland GR, Na¨hri MN, Addy M, Gangarosa L, Orchardson R. Guidelines for the design and conduct of clinical trials on dentine hypersensitivity. J Clin Periodontol 1997: 24: 808-813.
17) Ricarte JM, Matoses VF, Llacer VJF. Dentinal Sensitivity: Concept and methodology for its objective evaluation. Med Oral Patol Oral Cir Buccal. 2008; 13(3): E 201-E 206
18) Connie Hastings Drisko. Dentine hypersensitivity - dental hygiene and periodontal
Considerations. International Dental Journal.2002;52,385-903.
19) Van B Haywood. Dentine Hypersensitivity: Bleaching and restorative considerations for successful management. International Dental Journal.2002; 52,378-384. |