Introduction
Peripheral giant cell granuloma (PGCG) is a relatively common reactive exophytic lesion of the oral cavity [1]. The exact etiology of PGCG is not known, although it is thought that it may be due to an irritant or aggressive factor (trauma, tooth extraction, badly finished fillings, plaque, calculus, chronic infections, impacted food etc.) [2]. The influence of hormones has been suggested as contributory factor in PGCG development and predominance of these lesions in young females as well as some previously reported pregnancy related cases support this belief [3]. It has been observed that majority of lesions present in the first 4 decades of life, when hormonal changes are most pronounced [4]. Furthermore, peripheral giant cell granulomas are also considered in a group of lesions called “pregnancy tumors”. Clinically, PGCGs may present as polypoid or nodular lesions, predominantly bluish red with a smooth shiny or mamillated surface. They are variable in size, though reported rarely exceeding 2 cm in diameter, and are generally soft or rubbery to touch. Most commonly they are asymptomatic, but because of interference with occlusion they may ulcerate and become infected. They show site predilection for premolar and molar mandibular regions. Treatment is usually by surgical excision and elimination of possible irritant factors, with recurrence being infrequent (approximately 10%)[2]. The present report describes two cases of massive peripheral giant cell granuloma associated with pregnancy, an association which has been reported very rarely in literature.
Case Reports
Case -1
A 30-year-old female patient was referred to our center 3 months post-parturition with the chief complaint of painless enlargement in the lower right mandibular posterior region. Her history suggested that the lesion was present for the last ten months and there was sudden increase in the size during pregnancy. The lesion remained static in size post-parturition. Extraoral examination revealed diffuse swelling on right side of the face extending anteriorly from the oral commissure to body region of mandible posteriorly (Fig.1). On intraoral examination there was sessile, lobulated growth of the size 5 cm ×5cm in the mandibular premolar and molar area (Fig. 2). On palpation swelling was firm in consistency and skin over the swelling was normal in colour, texture and temperature. Lesion was reddish blue in color with patchy ulceration. Extensive lingual migration of second premolar was noted. Radiographically, bone resorption was found in premolar-molar region.
 | Fig.1 Pre-operative photograph showing extraoral swelling (Case 1)
 |
Calcium, phosphorus, alkaline phosphatase and parathyroid hormone levels were all within normal ranges. Surgical resection with extensive clearing of the base of the lesion was done under general anaesthesia (GA) (Fig. 3, 4). The histopathological study was consistent with the diagnosis of peripheral giant cell granuloma.
Case-II
A 32-year-old female in the second trimester of pregnancy reported with a painless swelling in the mandibular premolar molar region. Clinical examination revealed a sessile, nodular
 | Fig.2 Pre-operative photograph showing intraoral lesion (Case 1)
 |
 | Fig.3 Intraoperative photograph after surgical resection of the lesion (Case 1)
 |
 | Fig.4 Post-operative photograph (Case 1)
 |
 | Fig.5 Post-operative extraoral view (Case 1)
 |
 | Fig.6 Pre-operative photograph showing intraoral lesion on initial presentation (Case 2)
 |
swelling, bluish red in colour, measuring 1.5 × 2 cm in diameter, located in the mandibular premolar molar region (Fig. 6). The lesion was non tender and soft to firm in consistency and rubbery to touch. Patient was advised excisional biopsy but patient refused to undergo any kind of surgical intervention at that time. Oral prophylaxis was done and patient was advised to report after parturition. Patient reported back 3 months after parturition. Her history suggested that there was a sudden increase in the size of the lesion and it remained static after parturition. Extraoral examination revealed diffuse swelling on right side of the face extending anteriorly from the oral commissure to body region of mandible posteriorly. On palpation swelling was firm in consistency and skin over the swelling was normal w.r.t colour, texture and temperature. Intraoral examination revealed massive lesion in premolar molar region measuring approximately 5 cm × 4 cm obliterating the buccal and lingual vestibule (Fig. 7). Lesion was reddish blue in color, sessile, non tender on palpation and firm in consistency. Superior surface of the lesion was ulcerated with indentations of maxillary molars. Radiographic examination showed bone resorption in the form of a concave depression. Laboratory investigations (calcium, phosphorus, alkaline phosphatase and parathyroid hormone levels) were all within normal limits. Surgical resection with extensive clearing of the base of the lesion with curettage was done under GA. The histopathological study confirmed the diagnosis of peripheral giant cell granuloma.
The post operative course was uneventful and no sign of recurrence was observable at 16 months post-operatively in both the cases (Fig. 5, 8).
Discussion
Peripheral giant cell granuloma (PGCG) is not a true neoplasm but rather a benign hyperplastic reactive lesion caused by local irritation or chronic trauma. PGCG originates from the periodontal ligament or mucoperiosteum [5]. The etiology of peripheral giant
 | Fig.7 Intraoral photograph showing massive lesion on 2nd visit (Case 2)
 |
 | Fig.8 Post-operative intraoral view (Case 2)
 |
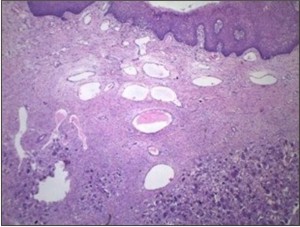 | Fig.9 Photomicrograph (H&E ×40) (Case 1)
 |
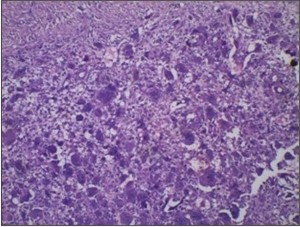 | Fig.10 Photomicrograph (H&E ×100) (Case 1)
 |
cell granuloma is still unclear. Some investigators suggested that a history of trauma might be related to the development of the lesions. Other possible factors that have been implicated, but not definitely proven, include hormonal disturbances, primary hyperparathyroidism, tooth extraction, poor dental restorations, food impactions, ill fitting dentures, orthodontic therapy, dental plaque, and calculus [6].
The etiology of peripheral giant cell granuloma in both our cases might be related to hormonal alterations during gestation period. Cailluette and Mattar [7] in their study found that peripheral giant cell granuloma and central giant cell granuloma are under the influence of the ovarian hormones. Chambers [8], suggested peripheral giant cell granuloma to be enhanced by pregnancy rather than being “pregnancy-dependent”. The responsiveness of the gingiva to these hormones along with the immunosuppressive actions of the hormones may have contributed to the growth of the lesion [8],[9]. Shirani G and Arshad M[4] stated that the ovarian hormones play no part in the development/growth of these lesions, but the evidence suggests that they may influence them only secondarily and their study results confirmed the role of poor oral hygiene in initiation of peripheral giant cell granuloma. Furthermore they concluded that the secondary influences of sex hormones with background of poor oral hygiene or other stimulation factors are important in etiology of peripheral giant cell granuloma. In their study they found that peripheral giant cell granuloma has predilection to females and occurs more frequently in first 4 decades of life when hormonal changes are prominent. Age and sex predilection in both of our cases is in accordance with the previous researches.
The two cases included in the present study showed the characteristic clinical appearance of PGCG, i.e. nodular growth, soft or rubbery to palpation, with a smooth shiny or mamillated surface. Most commonly, the cases reported in literature had lesion size varying from 1.0 to 2.0 cm in diameter but masses more than 5 cm have rarely been reported [5]. In our case report, the massive size of lesion (5 cm) may be attributed to hormonal influences during pregnancy and poor oral hygiene. Radiography revealed bone resorption w.r.t molar premolar region in both the cases. In the case series of PGCG reported by Chaparro-Avendano AV [5], two out of 5 patients showed radiographic evidence of bone resorption.
Histologically, PGCG consists of a non-encapsulated mass of tissue composed of a delicate reticular and fibrillar connective tissue stroma containing large numbers of ovoid or spindle shaped young connective tissue cells and multinucleated giant cells. Capillaries are numerous, particularly around the periphery of the lesion, and the giant cells sometimes may be found within the lumina of these vessels. Foci of hemorrhage, with liberation of hemosiderin pigment and its subsequent ingestion by mononuclear phagocytes as well as inflammatory cell infilteration, are also characteristics feature. Spicules of newly formed osteoid or bone are often found scattered throughout the vascular and cellular vascular lesion [10]. Both our cases presented with similar histo pathological findings with ill-defined mass composed of spindled mononuclear cells interspersed among numerous multinucleated osteoclast like giant cells in a fibrillar stroma. Small to medium sized vessels were seen at the periphery of the lesion admixed with chronic inflammatory infiltrate (Fig. 9, 10).
The peripheral giant cell granuloma should be differentiated from non ossifying fibromas, which differ in consistency and coloration; central giant cell granulomas, which are expansive and destructive intraosseous lesions that can perforate the cortex; chondrobl astomas and metastatic carcinomas, which when localized in the gingiva, may provoke irregular bone destruction below the exophytic lesion and hemangiomas, which, unlike PGCG lesions, are pulsatile and disappear under pressure. Pyogenic granulomas are difficult to differentiate from PGCG lesions on clinical grounds, but may be distinguished histopathologically [2],[11]. There was no sign of malignancy in both of our cases as indicated by lack of nuclear or cytological atypism on histopathological examination.
The surgical resection with elimination of the entire base of the lesion and removal of the underlying etiologic factors has yielded successful results in the treatment for PGCG. The superficial resection may lead to recurrence of the growth [12]. When the adjacent teeth are periodontally involved, their extraction may prove necessary to ensure full resection, though this is initially contraindicated[5]. In both our cases, lesions were surgically resected and the involved teeth were extracted because of they were periodontally involved and had poor prognosis. There has been reported wide variation of 5% to 70.6% in the recurrence rate of PGCG[13],[15].In both of our cases no recurrence was noted at one year post-operatively.
Conclusion
In conclusion, the hormonal influences during pregnancy may lead to the development of PGCG in patients with poor oral hygiene. This mandates the precise diagnosis of PGCG, based on the clinical, radiological and histological findings so that extensive damage to the underlying bone and consequent need for tooth extraction can be avoided.
References
1. Tandon PN, Gupta SK , Gupta DS et al. Peripheral giant cell granuloma. Contemp Clin Dent 2012; 3: 118-121.
2. Gandara-Rey JM, Pacheco Martins Carneiro JL, Gandara-Vila P et al .Peripheral giant-cell granuloma. Review of 13 cases. Med Oral 2002; 7: 254-259.
3. Gunhan M, Gunhan O, Celasun B et al. Estrogen and progesterone receptors in the peripheral giant cell granulomas of the oral cavity. J Oral Sci 1998; 40: 57-60 .
4. Shirani G, Arshad M .Relationship between circulating levels of sex hormones and peripheral giant cell granuloma. Acta Med Iran 2008; 46: 429-433 .
5. Chaparro-Avendano AV, Berini-Aytes L, Gay-Escoda C .Peripheral giant cell granuloma. A report of five cases and review of the literature. Med Oral Patol Oral Cir Bucal 2005; 10: 48-57.
6. Shadman N, Ebrahimi SF, Jafari S et al .Peripheral Giant Cell Granuloma: A Review of 123 Cases. Dent Res J 2009; 6: 47-50.
7. Caillouette JC, Mattar N .Massive peripheral giant-cell reparative granuloma of the jaw: a pregnancy dependent tumor. Am J Obstet Gynecol 1978;131: 176-9.
8. Chambers TJ, Spector WG .Inflammatory giant cells. Immunobiology 1982;161: 283-9.
9. Whitaker SB, Bouquot JE. Identification and semi-quantification of estrogen and progesterone receptors in peripheral giant cell lesions of the jaws. J Periodontol 1994; 65(3):280-3.
10. Rajendran R. Benign and malignant tumors of the oral cavity. In Shafer's (ed) Textbook of Oral Pathology. 7th ed .pp81-222. India: Elsevier; 2012.
11. Kaya G S, Yalcin E, Tozoglu U et al .Huge peripheral giant cell granuloma leading to bone resorption: a report of two cases. Cumhuriyet Dent J 2011;14(3):219-224.
12. Katsikeris N, Kakarantza-Angelopoulou E , Angelopoulos AP .Peripheral giant cell granuloma: clinico- pathologic study of 224 new cases and 956 reported cases. Int J Oral Maxillofac Surg 1988;17: 94-9.
13. Nedir R, Lombardi T, Samson J .Recurrent peripheral giant cell granuloma associated with cervical resorption. J Periodontol 1997;68(4):381-4.
14. Giansanti JS, Waldron CA .Peripheral giant cell granuloma: Review of 720 cases. J Oral Surg 1969;27:787-791.
15. Eversole LR, Rovin S .Reactive lesions of the gingiva. J Oral Pathol 1972;1:30-38. |