Introduction
Traumatic injury to a primary tooth has the potential to damage the underlying permanent tooth germ which may disturb its development. The extent of the malformation depends on the developmental stage of the permanent tooth and the intensity of the trauma.[1] Several developmental alterations, including white or yellow-brown discoloration, enamel hypoplasia, crown dilacerations, root duplication, vestibular root angulations, root angulations or dilacerations, sequestration of permanent tooth germs, disturbance in eruption, odontoma-like malformations and partial or complete arrest of root formation, have been reported in permanent teeth after dental and maxillofacial traumas.[1] The purpose of this paper is to report a rare case with simultaneous presence of odontoma, dilacerations, enamel hypoplasia and periapical cyst in a 14 year old female patient as a result of a trauma sustained in an accident, emphasizing the role of recent diagnostic modalities in its diagnosis and the management aspects to be taken into consideration while dealing with a combination of such clinical entities.
Case Report
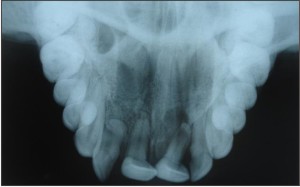
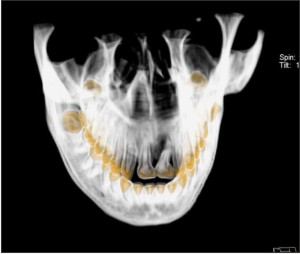
A 14 year old female patient reported with a chief complaint of pain in the upper front teeth since 1 year which is dull, intermittent, increases on eating food and is relieved on taking analgesics. She gave history of trauma in the same region at the age of 4 years. Intraoral examination revealed 11, 21 were labio-lingually tilted and had crossbite with 31, 41. Hypoplastic areas with white flecks and vertical streaks were seen on the labial surface of 11, 12, 21, 22. 12 was rotated mesio-labially and 11 and 21 were tender on percussion (Figure 1). 11 and 21 did not respond to electric pulp test. Intra oral periapical radiograph showed dilaceration of the roots of 11, 21. A well defined radiolucency at the apex of 21 and a radiopacity superimposed on the apical one third of 12 (Figure-2a) was present. Maxillary occlusal radiograph showed a radiopacity superimposed on the middle one third of the root of 12 along with the dilaceration of 11 and 21 (Figure-2b). Axial section of the CT Scan revealed the presence of an extra tooth like structure on the palatal aspect of 12 and was confirmed by 3 D reconstruction ( Figure 3a, 3b, 3c ).
Conventional root canal was attempted for 11, but ledge formation was felt while preparing the canal. So apicoectomy and root canal treatment was done together for dilacerated 11 and
 | Figure 1 - anterior crossbite, rotated right lateral incisor and hypoplastic areas seen on the labial aspect of maxillary anteriors.
 |
 | Figure 2a and 2b- dilacerated roots of maxillary central incisors, periapical radiolucency in relation to left maxillary central incisor, radiopacity superimposed at the apical one third of right maxillary lateral incisor.
 |
 | Figure 3a - axial section of CT scan shows extra tooth like structure palatal to right maxillary lateral incisor.
 |
 | Figure 4 - showing surgical procedure and the extracted odontome.
 |
21, the periapical cyst in relation to 21 was enucleated, and the odontome was extracted (Figure 4a, 4b). The endodontic procedure with metapex helped in resolution of the periapical pathology. The cystic lining and the odontome were sent for histopathological examination which was suggestive of periapical cyst and the odontome was confirmed to be a compound odontome. Oral prophylaxis was done and periodontal status was evaluated before starting the orthodontic treatment. In the maxillary arch straight wire technique using Roth brackets of slot size 0.022 inch was started with 0.014 inch Ni Ti round wire which was
 | Figure 5a and 5b - photograph showing during and after orthodontic treatment.
 |
replaced every 21 days with subsequent increase in wire size. (0.016, 0.018 and 0.020 inch). Later on, for finishing rectangular wire of 0.019 x 0.025 inches and 0.021 X 0.025 inches was used. In the mandibular arch removable posterior bite plane was given to relief the crossbite. The desired occlusion was obtained in six months, the patient is on retainer for the last 6 months and is under follow up (Figure 5a and 5b).
Discussion
Traumatic injuries to the primary dentition are very frequent, affecting from 4% to 30% of all children. The frequency varies according to the child's age at the time of the accident, gender,
 |
 |
 |
 |
type, and location of trauma.[2] The most commonly affected teeth in primary dentition are the upper central incisors. Children at the ages between 1 and 4 are the most affected since at this stage, they have insufficient motor control and fall quite often.[3] Developmental disturbances in the permanent teeth as a consequence of injuries to their predecessors vary from 12 to 69%.[4] Dental anomalies due to trauma include variations in normal number, size, eruption or morphology of the teeth. These anomalies can be divided into developmental abnormalities and acquired abnormalities. Given the complexities and interactions involved in tooth development, from initiation at about the sixth week in utero to eruption, the small number of various anomalies is surprising. This can range from a simple white or yellow brown discoloration to crown dilacerations, crown duplication, root dilacerations, root duplication, odontoma like malformation, partial or complete arrest of root formation, sequestration of the permanent tooth germ or disturbances in the eruption of the permanent teeth.[5] Usually one or two anomalies are seen, but in the present case, four anomalies were manifested which is very rare.
The term dilaceration describes an abrupt deviation of the long axis of the crown or root portion of the tooth. This deviation originates from a traumatic non-axial displacement of already formed hard tissue in relation to the developing soft tissue.[6] It is derived from a latin word dilacero which means tear up and was first used by Tomes and referred to as the 'forcible separation of the cap of the developed dentine from the pulp in which the development of dentine is still progressing'.[7] Generally, a history of trauma to the primary dentition at an early age is recorded as the etiological factor for the dilacerated teeth.[6]
The odontoma-like malformation is a rare sequelae which can occur as a consequence of a severe injury in a deciduous tooth, afflicting the successor germ in the initial stages of its mineralization, i.e., during Nolla's stages 1-3. The child's age at the time of trauma varying from 0 to 4 years, the maxillary incisors being the most affected teeth. The avulsion and intrusive luxation are the types of trauma that cause the bigger rate of this sequelae . The cleavage of the dental germ results in the development of separate elements of the tooth, featuring a structure similar to odontoma. A relevant factor in this high prevalence is the close anatomical relationship between the apices of the primary teeth and their developing permanent successors.[8] The odontome is characterized by the proliferation of hard dental tissues which can be classified into two types - compound which consists of a coalescent mass of multiple, deformed tooth like structures (denticles) and is most common in the younger age group and complex type which is mostly found in older individuals.[9] In the present case also, we could appreciate the presence of a compound odontome in relation to the palatal aspect of 11.
A high prevalence of enamel hypoplasia in permanent successors is observed when the dental trauma occurs in early childhood. During this period, the crown bud of the permanent successors are beginning their calcification, rendering them more susceptible to developmental disturbances.[2] The more frequent type of sequelae in the permanent teeth caused by the trauma of the antecessor is the hypoplasia of the enamel, which corresponds to approximately 12% of the disturbances.[8] In early ages, children tend to fall more often, and the close anatomic relationship between the apices of primary incisors and the successor's buds can cause more complex sequelae to the crowns of permanent successors.[10] Hypoplastic areas with white flecks and vertical streaks were seen on the labial aspect of 11, 12, 21, 22 in the present case.
In majority of the cases, periapical cyst is a consequence to pulpal necrosis following caries, with an associated periapical inflammatory response.[9] Other causes include any event that may result in pulpal necrosis such as trauma, tooth fracture and improper restorations. The first line of defence to pulpal necrosis in the periapical area is the formation of a granuloma. The presence of a cyst in relation to 21 may be attributed to the trauma during the period of odontogenesis.
The presence of dilacerations in relation to 11, 21 in the present case is due to trauma during the period in which the teeth were being formed, with the result that the position of the calcified portion of the teeth was changed and the remaining part of the teeth was formed at an angulation. Von Gool has emphasized that such an injury to a permanent tooth resulting in dilaceration often follows traumatic injury to deciduous predecessor in which that tooth is driven apically into the jaw.[7] An odontoma was seen on the palatal aspect of 12 which may be attributed to the cleavage of the dental germ after injury resulting in the development of separate elements of the tooth featuring a structure similar to the compound odontoma. The crown buds of permanent successors begin their calcification during early childhood, trauma at this stage renders them susceptible to enamel hypoplasia, which must have happened in the present case as well. The displaced epithelial cells of the developing tooth germ could be a source for forming epithelial lining of the cyst leading to the formation of a periapical cyst in relation to 21. Hence trauma may be considered as the etiology responsible for manifestation of all the four clinical entities.
The CT scan data can be very helpful where a series of radiographs may be taken at graduated depths in the region of interest. By viewing axial slices of the maxilla, the assessment of the exact location of the odontoma could be made. The sections were helpful in allowing the clinician to accurately assess the positions of crown and apex and the inclination of the long axis of the dilacerated teeth. Three-dimensional reconstruction of the images also helped in the confirmation of the presence of an odontoma. Recent diagnostic modalities assist tremendously in formulating the treatment plan for such malformations.
Since a tetrology of dental anomalies was present, a systematic well planned approach was essential while formulating the treatment plan. Since the dilacerated teeth had already erupted, and the patient wanted to improve the aesthetics, a conservative approach including apicoectomy with root canal treatment for 11, 21, followed by surgical removal of the odontome and enucleation of the cyst were carried out. Later the orthodontic treatment was planned and the patient is still under follow up.
Conclusion
Dilacerations, Enamel Hypoplasia, Odontome formations and Periapical cysts can occur collectively in the teeth, during their developing stage. Recent diagnostic modalities like computed tomography and its 3D reconstruction plays a crucial role in diagnosing and managing such malformations. The present case reinforces the importance of an early diagnosis, as well as of a proper clinical and radiographic examination which aids in formulating an appropriate treatment plan. By means of an adequate multidisciplinary approach, one can make it possible to provide a favorable prognosis and a satisfactory aesthetic treatment for the young patient.
References
1. Güngörmüs M, Yolcu U, Aras MH, Halicioglu K, Simultaneous occurrence of compound odontoma and arrested root formation as developmental disturbances after maxillofacial trauma: A case report, Med Oral Patol Oral Cir Bucal. 2010 Mar 1;15 (2):e 398-400.
2. S'ellos MC, Bader Sab TB, Souza Chagas MD, Campos V, Circular enamel hypoplasia in permanent maxillary incisors subsequent to trauma to their predecessors: A 10-year follow-up case report, Brazilian Journal of Dental Traumatology, 2009, 1(2): 50-53.
3. Ravn JJ, Developmental disturbances on permanent teeth after intrusion of their primary predecessors. Scand J Dent Res, 1976, 84: 137-41.
4. Andreasen JO & Andreasen FM, Textbook and color atlas of traumatic injuries to the teeth, 1994. Copenhagen: Mosby.
5. Asokan S, Rayen R, Muthu M. S, Siva Kumar N, Crown dilacerations of maxillary right permanent central incisor- A case report, J Indian Soc Pedo Prev Dent, 2004, Dec, 22 (4), 197-200.
6. Crescini A, Doldo T, Dilaceration and angulation in upper incisors consequent to dental injuries in the primary dentition: orthodontic management, Prog Orthod, 2002, 3, 29- 41.
7. Agnihotri A, Marwah N, Dutta S, Dilacerated unerupted central incisor: A case report, J Indian Soc Pedod Prev Dent - September 2006, 148-150.
8. Lenzi MM, Antero S, Monteiro A, Campos V, Odontoma-like malformation in permanent dentition due to severe trauma in deciduous dentition - case report, Brazilian Journal of Dental Traumatology, 2010, 2(1): 31-35.
9. Shafer WG, Hine. MK., Levy. BM, A Text Book of Oral Pathology, Elsevier 4th edition p- 265.
10. Smith RJ & Rapp RA. 1980. Cephalometric study of the developmental relationship between primary and permanent maxillary central incisor teeth. ASCD J Dent Child, 47: 36-41. |