Introduction:
Lupus erythematosus panniculitis is an uncommon variant of lupus erythematosus characterized by a specific involvement of the subcutaneous fat[1]. In this type of LE, deep dermal and subcutaneous nodules 1 to 3 or 4 cm in diameter, rubbery firm, sharply defined, and non-tender, occurs most often beneath normal skin of the head, face or upper arms. The chest, buttocks, and thighs may also be involved. This form of LE is characteristically chronic and occurs most often in women between ages 20 and 45[2]. It may appear in patients with discoid lupus erythematosus and systemic lupus erythematosus[2]. The lesions may heal with deep depressions from loss of the panniculus, which usually take years to fill in. The lupus panniculitis generally has a favorable prognosis. This report describes a classical case of Lupus erythematosus panniculitis with a brief review of literature.
Case Report:
A 26 year old married female presented with complaints of deep subcutaneous nodules with erythematous, bound down atrophic over lying skin, over bilateral cheeks of five to six months duration.(Fig.1) This was followed by progressive scarring alopecia of the scalp and oral ulcerations of around four to five months duration.(Fig. 2 & 3) Initially, the lesion on the face started as
 | Fig. 1 - Bilateral erythematous rash
 |
 | Fig. 2 - scalp skin - before treatment
 |
 | Fig. 3 - scalp - alopecia with scarring and fat inflammation
 |
asymptomatic red nodules which was initially diagnosed as nodulo-cystic acne by a physician. The patient was put on oral Isotretinoin following which the lesions continued to progress and in period of almost 15 days resulted in indentation of the affected skin. Soon after the patient developed bald patches on her scalp which were rapidly progressive. At the same time the patient also noticed small oral ulcerations on the hard palate. There were no acne lesions, seborrhoea anywhere else on the body. There was no family history of any autoimmune diseases. There was no history of fever, joint pains, Photo sensitivity, chest pain or cough, urinary or neurological problems. Also there was no history of preceding drug intake.
Clinical examination revealed a moderately built and moderately nourished middle-aged woman. The general physical as well as systemic examination did not reveal any findings. Cutaneous examination revealed a well to ill defined 1 to 1.5 cm erythematous, indurated, atrophic nodules with central indentation over bi-lateral cheeks. (Fig.4) Perilesional erythema and telengiectasias were also noticed. There was however no classical butterfly rash or oedema of the skin.
Scalp examination revealed diffuse scarring alopecia on the fronto-parietal scalp with multiple atrophic yellowish plaques along with crusting which were associated with erythema, depigmentation and atrophy of the surrounding skin[3]. (Fig.3) Hair pull test was positive. However no follicular plugging or comedowns were noticed in the scalp. Examination of the oral cavity revealed erosions and shallow ulcerations with surrounding erythema on the hard palate and associated gingivitis. Examination of the eyes and nails was within normal limits.
Patient's investigations revealed a haemoglobin level of 10g/dl with total leucocyte count 6500 cells/ mm[3]. Liver function test (LFT), Renal Function Test (RFT), Serum electrolytes, Random blood sugar and Urine analysis were normal. The serology of the patient's ANA was positive and showed a speckled pattern.
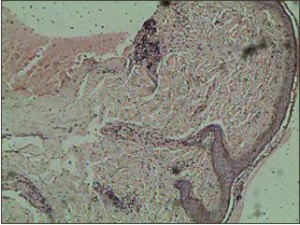
Routine Histopathology of the lesional facial skin showed atrophic squamous lining with pigmentation.(Fig.5) There is sub epidermal oedema with mild mixed inflammatory infiltrate comprising of lymphoid cells, neutrophils and plasma cells.(Fig.6) Peri-follicular inflammatory cell infiltrate is seen in the deep dermis extending into the subcutaneous adipose tissue in the interstitial pattern.(Fig.7) Focal areas of fatty degeneration are also seen. There is increase in collagen matrix with entrapped adipocytes and nerve bundles along with the areas of haemorrhage. Immunofluorescence could not be done as the patient could not afford it. Patient was treated with oral hydroxy chloroquine 200 mg twice daily. However her total leucocyte count dipped to 3500 cells/ mm[3] in one month's time. The Patient was then started on low dose oral steroids initially 20 mg daily for 3 weeks and now maintained on 20 mg alternate day for past two months. Following addition of the steroids, her TLC picked up to normal and her skin and scalp erythema also subsided. However
 | Fig. 4 - Erythematous skin with indentation and atrophy
 |
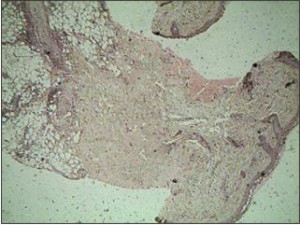 | Fig. 5 - Showing atrophic squamous epithelium with pigmentations
 |
 | Fig. 6 - Showing sub epidermal oedema with mixed inflammatory infiltrate
 |
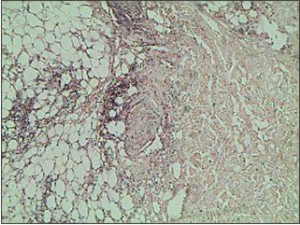 | Fig. 7 - Showing inflammatory cell infiltrate extending in to subcutaneous adipose tissue
 |
 | Fig. 8 - After treatment - erythmatous skin and indentation
 |
 | Fig. 9 - After treatment - decreased inflammation and regrowth of hair
 |
hair loss was still significant and the skin lesions were also quite bothersome to the patient. Following this we added intralesional triamcinolone in to the skin, scalp and oral lesions which resulted in healing of the oral lesions in one session and significant improvement in skin and scalp lesion in 3 to 4 sessions repeated at 15 days interval.(Fig.8 & 9)
Discussion:
Kaposi first described lupus erythematosus panniculitis, also known as lupus panniculitis and lupus profundus in 1869. Arnold established it as a subtype of lupus erythematosus in 1956. Lupus erythematosus panniculitis, an uncommon variant in the clinico-pathological spectrum of lupus erythematosus (LE), is characterized by chronic inflammation and hyaline necrosis of subcutaneous tissue[1].
It usually affects middle-aged women, though cases of pediatric patients have been published[4]. The lesions are most frequent on cheeks but other sites of predilection are face, upper arms, hands, chest, buttocks and thighs. In most of the patients with lupus panniculitis, there will be preceding, subsequent, or concomitant lesions of discoid lupus erythematosus. Approximately 2%-7% of patients with systemic lupus develop lupus panniculitis. It has generally been observed that patients with lupus erythematosus lesions occasionally develop systemic manifestations and present abnormal test results[5]. Clinical findings include indurated subcutaneous plaques and nodules that, although initially movable, adhere to deep layers. These are persistent lesions that do not usually become ulcerated, though when ulceration does occasionally occur, they are painful[5]. The overlying skin may be intact or show discoid lupus erythematosus lesions in 20%-70% of cases.
The present case involves a middle-aged woman presenting erythematous, indurated, atrophic nodules with central indentation over bilateral cheeks along with peri-lesional erythema and telengiectasias. The reported case also revealed scarring alopecia on the fronto-parietal scalp with multiple atrophic yellowish plaques along with erythema, depigmentation and skin atrophy but there were no findings compatible with chronic discoid lupus erythematosus[6].
The principal problem in these atypical cases is confusion essentially with neoplastic processes and connective-tissue diseases. The main differential diagnosis in the present case is subcutaneous panniculitis-like T-cell lymphoma (SPTCL). Histopathologic features of lupus panniculitis reveals atrophy of the epidermis, vacuolar change at the dermo-epidermal junction, thickened basement membrane, and superficial and deep perivascular inflammatory infiltrate of lymphocytes involving the dermis. The present case revealed atrophic squamous lining with sub epidermal oedema. Mild mixed inflammatory infiltrate comprising of lymphoid cells, neutrophils and plasma cells were noted in the present case[7]. Fatty degeneration was also seen at places. Laboratory assays for antinuclear antibodies are positive in 70% of patients, as was the case with our patient.
Clinical Features of Classical SLE were however absent in our patient except for laboratory findings such as a low TLC and ANA positivity .There was no butterfly facial rash, photo sensitivity, nonscarring alopecia, arthritis or any systemic manifestations classical of SLE.
Treatment is most effective if initiated during the active phase of the disease and often requires systemic therapy because of the location of the inflammation. Antimalarials are the initial treatment of choice for most cases of lupus erythematosus panniculitis, whereas corticosteroids in combination with other steroid-sparing immunosuppressive agents are the first-line treatment for panniculitis in patients with dermatomyositis[8],[9],[10]. The advent of topical calcineurin inhibitors has contributed substantially to the armamentarium of external treatment options. By specifically interfering with intracytoplasmic signal transduction to activate the nuclear factor of activated T-cells (NF-AT), they are able to modulate various inflammatory mechanisms. The two available compounds, pimecrolimus and tacrolimus, do not induce the skin atrophy characteristic of corticosteroids. They have been studied in a number of case reports, but only in a few randomized, comparative studies. Both are well-tolerated, but differentially effective in the various subsets of CLE. Further studies are needed to directly compare the two compounds to each other, as well as to topical corticosteroids, before final recommendations can be made[11]. In the reported case, patient improved rapidly following administration of oral hydroxy chloroquine, low dose oral steroids topical tacrolimus and intralesional triamcinolone. The present case throws light on this uncommon variant of lupus erythematosus, oral manifestations of the disease, its confusion with other skin diseases such as nodular acne especially in the early stages and the chances of its progression to a more systemic form of LE.
Conclusion:
Thus, the present report is concerned with the clinicopathological description of lupus panniculitis but further systematic and extensive analyses of many more cases is important for the better understanding of the lesion.
References:
1. Arai S, Katsuoka K. Clinical entity of Lupus erythematosus panniculitis/lupus erythematosus profundus. Autoimmun Rev. 2009 May; 8(6):449-52. Epub 2009 Jan 20.
2. Ng PP, Tan SH, Tan T. Lupus erythematosus panniculitis: a clinicopathologic study. Int J Dermatol 2002 Aug; 41(8):488-90.
3. Kossard S. Lupus panniculitis clinically simulating alopecia areata. Australas J Dermatol. 2002 Aug; 43(3):221-3.
4. Guissa VR, Trudes G, Jesus AA, Aikawa NE, Romiti R, Silva CA. Guissa VR, Trudes G, Jesus AA, Aikawa NE, Romiti R, Silva CA. Acta Reumatol Port. 2012 Jan;37(1):82-5.
5. Patel RM, Marfatia YS. Lupus panniculitis as an initial manifestation of systemic lupus erythematosus. Indian J Dermatol. 2010;55(1):99-101
6. Chen YA, Hsu CK, Lee JY, Yang CC Linear lupus panniculitis of the scalp presenting as alopecia along Blaschko's lines: A distinct variant of lupus panniculitis in East Asians? J Dermatol. 2011 Dec 16. doi: 10.1111/j.1346-8138.2011.01455.x. [Epub ahead of print]
7. Massone C, Kodama K, Salmhofer W, Abe R, Shimizu H, Parodi A, Kerl H, Cerroni L. Lupus erythematosus panniculitis (lupus profundus): clinical, histopathological, and molecular analysis of nine cases. J Cutan Pathol. 2005 Jul;32(6):396-404.
8. Hansen CB, Callen JP. Connective tissue panniculitis: lupus panniculitis, dermatomyositis, morphea/scleroderma. Dermatol Ther. 2010 Jul-Aug;23(4):341-9.
9. Martens PB, Moder KG, Ahmed I. Lupus panniculitis: clinical perspectives from a case series. J Rheumatol. 1999 Jan; 26(1):68-72.
10. Chung HS, Hann SK. Lupus panniculitis treated by a combination therapy of hydroxychloroquine and quinacrine. J Dermatol 1997 Sep; 24(9):569-72.
11. Sticherling M. Update on the use of topical calcineurin inhibitors in cutaneous lupus erythematosus. .Biologics. 2011;5:21-31. Epub 2011 Feb 14. |