Introduction:
Periodontal diseases represent mixed infections of the periodontal tissues caused by primarily anaerobic Gram-negative bacteria. The deepening of the periodontal sulcus which occurs during the course of these infections is concurrent with a marked bacterial proliferation, resulting in bacterial cell levels reaching 10[9] or 10[10] bacteria within a single pathological periodontal pocket.[1] The ulcerated epithelial lining of the periodontal pocket may constitute a substantial surface area in cases of generalized chronic periodontitis and provides a gate through which lipopolysaccharides (LPS) and other antigenic structures of bacterial origin challenge the immune system and elicit a local and systemic response[2].The local response includes swollen red gingiva, gingival bleeding, suppuration, periodontal pocket formation, gingival recession and loss of supporting alveolar bone, whereas systemic response includes bacteremia, which is directly related to the severity of the inflammation of the periodontal tissues. It has therefore been speculated that periodontitis results in a low grade systemic inflammation.[3]
A study by Hutter et al (2001) provides evidence that periodontitis, like other chronic conditions, may tend towards anemia as the number of erythrocytes and levels of hemoglobin are lower in affected individuals. These findings may be related to elevated levels of pro-inflammatory cytokines in plasma of periodontitis patients suppressing erythropoiesis. Anemia of chronic disease (ACD) has been described in the literature, and seems to one of the most common forms of anemia observed in clinical medicine. ACD is defined as the anemia occurring in chronic infections, chronic inflammatory processes or tumor formation that is not due to dysfunction of bone marrow cells or other diseases, and occurring despite the presence of adequate iron stores and vitamins.[4],[5]
A characteristic finding of the disorders associated with the ACD was the increased production of cytokines that mediate the immune or inflammatory response; such as tumor necrosis factor, interleukin-1 and the interferon.[6],[7],[8],[9]
All the processes involved in the development of ACD can be attributed to these cytokines, including shortened red cell survival, blunted erythropoietin response to anemia, impaired erythroid colony formation in response to erythropoietin, and the abnormal mobilization of reticuloendothelial iron stores. These cytokines are also released by periodontal tissues in response to bacterial infection, which suggests that periodontitis like other chronic disease may cause ACD. However, conflicting results have been reported regarding the association of periodontal disease and anemia[3],[10],[11]
The purpose of the present clinical trial was to compare the hematological parameters: Hemoglobin (Hb), Erythrocyte sedimentation rate (ESR) and Red cell indices (MCV, MCH, MCHC) in patients with moderate to severe chronic periodontitis with that of periodontally healthy subjects, and thereby evaluating the possible association between chronic perio dontitis and anemia.
Materials And Method:
Subject Selection
The study was carried out as a parallel two group clinical trial. The study design was approved by the Medical Ethical Committee. The study population consisted of 80 systemically healthy non-smoker subjects within the age group of 22-40 years visiting the Department of Periodontology and Oral Implantology. The criteria for inclusion were 1) presence of atleast 20 teeth, 2) no history of antibiotic intake for the last 3 months prior and during the course of the study 3) no history of any minor or major trauma, any oral or general surgical procedure, which could have resulted in blood loss, 4) no history of any periodontal treatment at least 6 months before the commencement of the study, 5) no history of blood transfusion and / or donation minimum 3 months prior to study, 6) no history of use of vitamin or iron supplementation within the previous 3 months.
The study subjects were categorized into 2 groups: Group A and Group B with 40 (20 males and 20 females) individuals each. Group A included subjects with moderate to severe periodontitis (test group) and Group B included periodontally healthy subjects (control group).
The selected subjects were verbally informed about the study protocol and a written consent was taken.
A full mouth periodontal examination was conducted for all the subjects using the following clinical parameters -
Gingival Index - Loe and Silness, 1963
Probing Pocket Depth - using William's Periodontal Probe
Relative Attachment Level (only for Group A) - using William's Periodontal Probe with customized acrylic stent.
Collection of Blood Sample
After recording the clinical parameters, 5 ml of venous blood was drawn under aseptic conditions, from the ante cubital fossa. The drawn blood was transferred immediately to EDTA containing vacutainers to be transported to the Medical Laboratory. The estimation of the following hematological parameters was done.
Hemoglobin level (Hb),
Erythrocyte Sedimentation Rate (ESR),
Mean Corpuscular Volume (MCV),
Mean Corpuscular Hemoglobin (MCH) and
Mean Corpuscular Hemoglobin Concentration (MCHC)
Statistical Analysis:
The data so obtained was compiled and analysed using Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, version 15.0 for windows). Mean and Standard deviation for all parameters were calculated. The statistical significance of differences in independent variables for the intergroup measurements over time were tested according to Student t test (two tailed, independent). A two tailed Probability value (p-value) < 0.01 was considered as significant. P-value > 0.01 was considered as non-significant.
Observations and Results:
The mean value of hemoglobin (Hb) in males was 10.65 in Group A (test) as compared to 12.84 in Group B (control), whereas in females, the mean value of Hb was 9.18 in Group A (test) as compared to 10.95 in Group B (control). The difference in mean between test and control groups in both males and females was statistically significant when compared (p<0.01). Similarly, the mean value of Mean Corpuscular Volume (MCV) and Mean Corpuscular Hemoglobin (MCH)were significantly lower in Group A (males: 78.88 and 27.12, females: 72.12 and 24.19, respectively) as compared to Group B (males: 86.14 and 30.49, females: 83.88 and 29.54, respectively). Themean value of Mean Corpuscular Hemoglobin Concentration (MCHC) was lower in Group A (males: 31.45, females: 30.73) as compared to Group B (males: 33.27, females 32.88) but the difference was not statistically significant. However, the mean value of ESR was significantly higher in Group A (males: 20.6, females: 37.2) as compared to Group B (males: 4.45, females: 9.60).
Discussion:
The mouth is the mirror of health or disease, as a sentinel or early warning system, as an assessable model for the study of other tissues or organs and as a potential source of pathology affecting other systems and organs. The concept of periodontal diseases
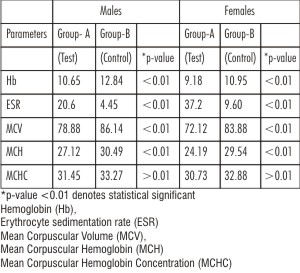 | TABLE-1: Mean and student's t-test significance values for systemic parameters within groups.
 |
as localized entities affecting only the teeth and supporting apparatus has been revised, as it has been seen that rather being confined to the periodontium, periodontal diseases have wide ranging systemic effects.[12] Periodontal disease has a proven relationship with several systemic conditions like cardiovascular diseases, diabetes mellitus, adverse pregnancy outcomes, obesity and stroke. One of the lesser-documented association has been the inter relationship between periodontal disease and anemia.
Anemia of chronic disease "ACD" is an immune driven process in which cytokines result in decrease derythropoietin production, impaired proliferation of erythroid progenitor cells and disturbed iron homeostasis.[4] This normocytic and normochromic anemia has been described in many chronic diseases like rheumatoid arthritis, renal failure, bacterial and parasitic infections, chronic periodontitis etc.
The present study was undertaken to study the possible association between the hematological parameters and the severity of periodontitis. The current study excluded smokers,[13] patients on antibiotics and with recent history of blood loss, systemic conditions such as cardiovascular disease, metabolic syndrome and diabetes, as these characteristics can act as possible confounding factors that could alter the haematological parameters.[14]
Clinical parameters viz. gingival index, probing pocket depth and relative attachment level were included in the study for the assessment of the inflammatory state of the gingival tissues and the severity of the periodontal disease. The hematological parameters viz. Hemoglobin (Hb), erythrocyte sedimentation rate (ESR), MCV, MCH and MCHC were selected for evaluation, as these are indicative of the anemic state of the patient and also the type of anemia based on morphology of the cell.
In the current study, both males and females were included, and it was observed that the hematological values for females in Group A (test) were less than reference range. The possible reason for this could be hormonal changes encountered in females during pregnancy, lactation, menstrual cycle, reproduction etc. as reported by Bentley ME and Griffiths PL in 2003.[15] Another reason could be there lack of awareness regarding the importance of balanced diet and nutrition as all these subjects belong to rural background.
The results of the study indicate that both test male and female groups showed a significant lower values of hemoglobin when compared to control, so periodontitis needs to be considered as a chronic disease which may cause lower number of erythrocytes and consequently lower hemoglobin levels.. The pathogenesis for the current findings is most likely similar as reported for rheumatoid arthritis, i.e. downregulation of the erythropoiesis in bone marrow by proinflammatory cytokines could be responsible for decreased blood counts. Systemic circulation of cytokines originating from local inflammation suppresses erythropoiesis.[3]
In our study, MCV, MCH, MCHC levels in both groups were within the reference values, indicating normocytic anemia, as commonly seen in ACD, although in test females these values were significantly lower than reference values indicating mildly hypochromic anemia. While hypochromia is commonly suggestive of iron deficiency anemia, a mildly hypochromic ACD has been reported in 30-40% of cases.[4]
In test group both males and females, ESR values had been increased, suggesting of chronic infection. If hematocrit is reduced, as in anemia, red cell aggregates sediment faster, thus the severity of anemia correlates with the ESR .The ESR is a traditional parameter in medicine of any given inflammatory process. It provides a multi-factorial measure of the systemic response to an infectious or inflammatory disease, i.e. a change in the plasma concentration of several inflammation related proteins, that affect the formation of rouleaux by erythrocytes, and which subsequently precipitate (sedimentation). However, this parameter of inflammation seems of limited use as diagnostic tool in periodontitis to measure the systemic involvement.[3],[16]
The results of the present study are in agreement with those conducted byHutter et al.[3](2001) and Thomas et al.[17] (2006)which also reported lower hematocrit, lower numbers of erythrocytes, lower hemoglobin levels and higher erythrocyte sedimentation rates in periodontitis patients when compared to healthy controls. Agarwal et al.[20] (2009) also, demonstrated a significant improvement in hemoglobin value and erythrocyte count after periodontal treatment, including surgery in patient with generalized chronic periodontitis with anemia. However, Wakai et al [10](1999) and Aljohani H A[19] (2010) failed to show any association between hemoglobin levels and periodontal status. Furthermore, Havemose-Poulsen et al.[11] (2006) failed to show any association between hemoglobin levels and periodontal status in patients with localized aggressive periodontitis, generalized aggressive periodontitis, juvenile idiopathic arthritis, and rheumatoid arthritis.
Within the limitations of the present study, it can be stated that chronic periodontal diseases are associated with alterations in the hematological parameters viz. hemoglobin, erythrocyte sedimentation rate and red cell indices. These findings may be related to the elevated levels of pro-inflammatory cytokines in plasma of periodontitis patients suppressing erythropoiesis. The present study has paved the path for future studies, with a larger study population for a longer period of time to further validate the association between periodontal disease and anemia.
Conclusion
A positive relationship was observed between the haematological parameters viz. Hb, ESR, MCV, MCH and MCHC and the severity of the chronic periodontal disease, suggesting that like other chronic conditions, periodontitis, may tend towards anemia.
References:
1. Haffajee A.D and Socransky S.S. Microbial etiological agents of destructive periodontal diseases. Periodontology 2000, 1994; 5: 78-111.
2. Ebersole J.L and Taubman M.A. The protective nature of host responses in periodontal diseases. Periodontology 2000, 1994; 5: 112-41
3. Hutter JW, Velden UVD, Varoufaki A, Huffels RAM, Hork FJ, Loos BG.Lower numbers of erythrocytes and lower levels of hemoglobin in periodontitis patients compared to control subjects. J Clin Periodontol 2001; 28: 930-6.
4. Weiss G, Goodnough LT. Anemia of chronic disease. N Engl J Med 2005; 352: 1011-23.
5. Means RT. Hepcidin and cytokines in anaemia. Hematology 2004; 9: 357-62.
6. Fuchs, D., Hausen, A., Reibnegger, G., Werner, E. R., Werner-Felmayer, G., Dierich, M. P. & Wacher, H. Immune activation and the anaemia associated with chronic inflammatory disorders. European Journal of Haematology 1991; 46, 65-70.
7. Katevas, P., Andonopoulos, A. P., Kourakli- Symeonidis, A., Manopoulou, E., Lafi, T., Makri, M. & Zoumbos, N. C. Peripheral blood mononuclear cells from patients with rheumatoid arthritis suppress erythropoiesis in vitro via the production of tumor necrosis factor alpha. European Journal of Haematology 1994; 53, 26-30.
8. Means, R. T., Dessypris, E. N. & Krantz, S. B. Inhibition of human erythroid colony-forming units by interleukin-1 is mediated by gamma interferon. Journal of Cellular Physiology 1992; 150, 59-64.
9. Vreugdenhil, G., Kroos, M. J., van Eijk, H. G., Lowneberg, B. & Swaak, A. J. G. Impaired iron uptake and transferring binding by erythroblasts in the anaemia of rheumatoid arthritis. British Journal of Rheumatology 1990; 29, 335-339.
10. Wakai K, Kawamura T, Umemura O, Hara Y, Machida J, Anno T, et al. Associations of medical status and physical fitness with periodontal disease. J Clin Periodontol 1999; 26(10): 664-672.
11. Havemose-Poulsen A, Westergaard J, Stoltze K, Skjødt H, Danneskiold-Samsøe B, Locht H, Bendtzen K, Holmstrup P. Periodontal and hematological characteristics associated with aggressive periodontitis, juvenile idiopathic arthritis, and rheumatoid arthritis. J Periodontol 2006; 77(2): 280-288.
12. Page RC. Periodontal diseases: a new paradigm. J dent edu 1998;2: 812-21.
13. Nordenberg D, Yip R, Binkin NJ.The effect of cigarette smoking on hemoglobin levels and anemia screening. JAMA.1990 26;264(12):1556-9.
14. Shi Z, Hu X, Yuan B, Hu G, Pan X, Holmboe-Ottesen G.Coexistence of anaemia and the metabolic syndrome in adults in Jiangsu, China.Asia Pac J Clin Nutr.2008; 17 (3):505-13.
15. Bentley ME, Griffiths PL. The burden of anemia among women in India. Eur J Clin Nutrition 2003; 57: 52-60.
16. Witte DL, Angstadt DS, Davis SH, Schrantz RD. Predicting bone marrow iron stores in anemic patients in a community hospital using ferritin and erythrocyte sedimentation rate. Am J Clin Pathol 1988; 90: 86.
17. Thomas B, Ramesh A, Ritesh K. Relationship between periodontitis and erythrocyte count. JISP 2006; 10: 288-91.
18. Rai B, Kharb S. Effect of Scaling and Root Planning in Periodontitis on Peripheral Blood. IJDS 2008; 6(1).
19. Aljohani HA. Association between Hemoglobin Level and Severity of Chronic Periodontitis. JKAU 2010 ; 17 (1):53-64 .
20. Agarwal N, Kumar VS, Gujjari SA. Effect of periodontal therapy on hemoglobin and erythrocyte levels in chronic generalized periodontitis patients: An interventional study. J Indian Soc Periodontol 2009; 13(1): 6-11. |