Introduction
Gingival recession is characterized by the displacement of the gingival margin apically from cementoenamel junction (CEJ), it could be localized or generalized, or associated with one or more surfaces of tooth[1]. Gingival recession has long been a major concern of many patients. The common gingival recession associated problems include plaque retention, gingival bleeding, and abrasion, pain due to cervical dentine hypersensitivity, root caries and fear of tooth loss.
In the past various treatment modalities have been used in the treatment of gingival recession. But all these procedures resulted in repair involving a combination of connective tissue adhesion and formation of long junctional epithelium which is a weak barrier and is prone for recurrence of periodontal pocket disease. Thus minimal periodontal regeneration is seen following this conventional method of periodontal therapy [2].
One of the treatment modalities for periodontal regeneration includes guided tissue regeneration (GTR). GTR is based on the principle so as to guide the epithelial cell proliferation, and prevent the ingress into the sites where it is desired to achieve regeneration of periodontal tissue[3].
Earlier the non-resorbable barrier membranes (the first generation membranes ) which required the second surgical intervention for their retrieval were available viz.thin aluminium foil, millipore (ethyl cellulose filter), d-PTFE (dense polytetrafluoroethylene), e-PTFE (expanded poly tetra fluoroethylene), rubber dam material etc. To eliminate the need for second surgical procedure and potential morbidity associated with it the resorbable membranes were introduced. These membranes are classified as secondgeneration membranes and include atelocollagen, polylactic acid, polyurethanes, oxidized cellulose, polycaprolactones, poly hydroxy butyrate, polycarbonate, polyglactin 910, type I-III collagen (Bio-Gide)® etc. [4].
The rationale for selecting type I-III collagen membrane (Bio-Gide)® is, this membrane has two layers, one compact and other porous. The compact layer has a smooth cell occlusive surface which is turned towards soft tissue where as porous layer which stabilizes the blood clot and encourages the integration of bone forming cells is turned towards the bone [5].Moreover collagen is the major extracellular macromolecule of the periodontal connective tissue. It has shown to be chemotactic to fibroblasts, acts as a barrier membrane for migrating epithelial cells, serves as a fibrillar scaffold for early vascular and tissue in growth and facilitates early wound stabilization and maturation , possess hemostatic properties and is weakly antigenic, therefore biocompatible. It might augment the tissue volume as it is absorbed and replaced by host tissue[6],[7].
The aim of this study was to evaluate the results of highly purified collagen membrane barrier in the treatment of human gingival isolated buccal recession.
Subjects And Methods:
Materials and methods:
Patient selection:Fifteen patients were selected from amongst the patients reporting G.D.C Amritsar, OPD.
The inclusion criteria of the patients in this study were as follows:
a) Presence of Miller's Class I and II bilateral localized buccal gingival recession defect on a non molar tooth.
b) Patients not suffering from any systemic or debilitating disease which may influence the outcome of the treatment.
c) Non-smokers and non-alcoholic.
d) Patients with no known history of allergy.
Presurgical Treatment
Prior to study, the ethical clearance from Institutional ethical committee was obtained. After an explanation of the proposed study criteria, including alternative treatments and potential risks and benefits, the participants were asked to sign the informed consent. For every case, oral prophylaxis was carried out and the patients were instructed to adopt meticulous home care measures.
In a split mouth design, the pairs of defects were randomly assigned for treatment with either coronally repositioned flap alone or coronally repositioned flap in conjunction with resorbable collagen membrane.
Measurements
One examiner was validated for recording of clinical parameters viz. probing depth (PD), clinical attachment level(CAL), gingival recession (GR) at baseline, 3 months and 6 months post-operative.
Surgical Procedure:
The area to undergo surgery was anesthetized with local anaesthetic solution (lignocaine hydrochloride 2% with adrenaline 1:200, 000).
GROUP B:
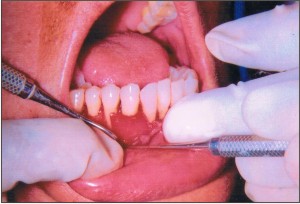
Full-thickness mucoperiosteal flap was raised to gain access and clean the designated area. With the help of curettes and burs the exposed root surface of the tooth .was planed to obtain a flattened or concave profile (Figure1). Following the procedure, the entire surgical area was irrigated. A relieving incision was given at the base of the flap so as to facilitate its coronal positioning.
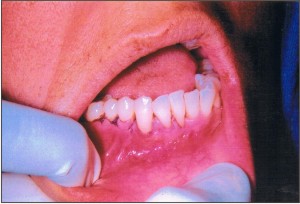
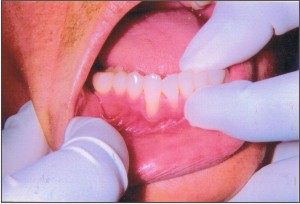
Placement of collagen membrane: Resorbable bilayer collagen membrane of porcine origin [(Bio-Gide)®, Geistlich Inc.,Switzerland] was cut to obtain the required size with the help of a template and was placed over the denuded root surface/surfaces extending from CEJ to 2-3 mm beyond the bony margins both laterally as well as apically (Figure 2). The membrane was secured by suturing to the periosteum with 4-0 resorbable vicryl suture and flap was coronally repositioned at CEJ to cover the membrane completely and the facial and lingual flaps were approximated in interproximal area (Figure 3).
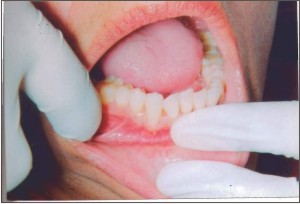
Post-operative assessments were done and measurements were recorded at 3 and 6 months post-operative (Figure 4-6).
GROUP A:
Same surgical procedure was followed to facilitate the coronal repositioning of the flap and flap was sutured interproximally using 4-0 resorbable sling sutures.
Results:
It was observed that the material exhibited excellent handling character istics and easy manipulation. It was well tolerated by all the patients without any adverse tissue reaction, infection or delayed healing during the course of the study. The control group Group A was treated with coronally repositioned flap alone and test group Group B was treated with coronally repositioned flap combined with resorbable collagen membrane.
During the course of study wound healing was uneventful and no membrane exposure occurred in test group. None of the patient dropped out before
 | Figure 1-Showing root planning and flattening of the root surface being done with rotary instruments
 |
 | Figure 2- Showing the dehiscence defect covered with collagen membrane
 |
 | Figure 3- Showing the sutured coronally repositioned flap
 |
 | Figure 4- Showing pre-operative site with gingival recession in relation to right lower canine
 |
 | Figure 5- Showing the operated site 3 months post-operative
 |
 | Figure 6- Showing the operated site 6 months post-operative
 |
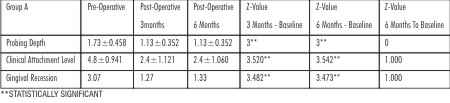 | Table 1- Comparison of clinical parameter between baseline value, 3 months and 6 months follow-up value in control group (Mean± SD; in mm)
 |
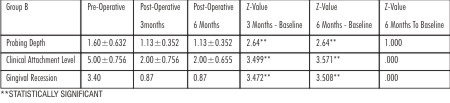 | Table 2- Comparison of clinical parameter between baseline value, 3 months and 6 months follow-up value in test group (Mean± SD; in mm)
 |
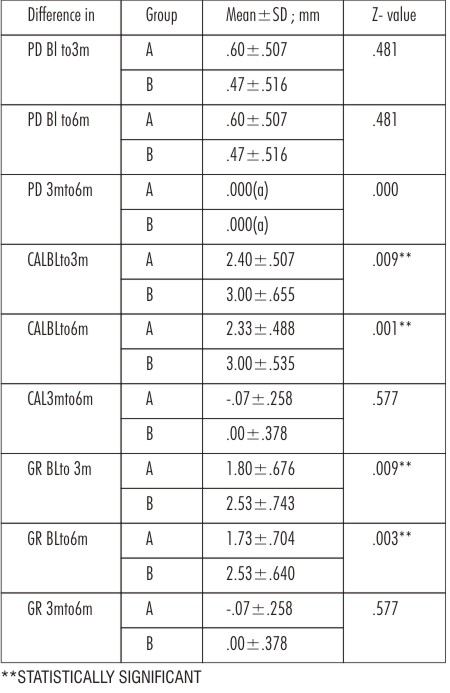 | Table 3- Comparison of clinical parameters between control (Group A) and test (Group B) groups at baseline, 3 months and 6 months follow-up
 |
termination of the study.
At baseline mean gingival recession was 3.40±0.961 in test group and 3.07± .961 in the control group. Similarly probing pocket depth was 1.60±0.632 in the test group and 1.73±0.458 in the control group. Mean clinical attachment level (CAL) was 5.00±0.756 in the test group and 4.81±0.941 in control. At the baseline, no statistical differences in any of the investigated parameters were observed between test and control group, indicating randomization was effective.
At 3 months follow-up, probing depth in the test group was 1.13±0.352 and 1.13±0.352 in the control group. At 6 months follow-up it was 1.13±0.352 and1.13±0.352 respectively.
Similarly CAL at 3 months follow-up was 2.00±.756 in the test group and 2.4±1.121 in the control group. At 6 months follow-up it was 2.00±.65and 2.4±1.060 respectively.
Gingival recession was 0.87±.743 in the test group and 1.27±1.100 in the control group at 3 months follow-up. At 6 months follow-up it was 0.87± 0.743 and 0.87±640 respectively (Table1, 2).
Discussion
The aim of present study was to evaluate the efficacy of highly purified bilayer collagen membrane in the treatment of human gingival isolated buccal recession.
This material was easy to manipulate and was well tolerated by the patients with no unusual findings with regard to post-operative healing as well as sign or symptoms of any other allergic manifestations. These findings concur with the findings of Blumenthal 1993[8], Swol et al 1993 [9], and Wolf et al 2000[10], who reported no untoward reaction with collagen membrane.
Both Group A and Group B showed a statistically significant reduction in pocket depth from baseline to 3 months and 6 months post-operative. But reduction was non-significant from 3 months to 6 months post-operative (Table 1,2). Difference in pocket depth reduction between Group A and Group B from baseline to 3 months, 6 months post-operative and between 3 and 6 months post-operative was non- significant (Table 3).Mean gain in clinical attachment level in both the groups was statistically significant from baseline to 3 months and 6 months post-operative and was non-significant from 3 to 6 months post-operative (Table 1, 2). Difference in CAL gain from baseline to 3 months post-operative in Group A 2.40±0.507 and in Group B 3.00±0.655 and from baseline to 6 months post-operative 2.33±0.488 and 3.00±0.535 respectively which was statistically significant (Table 3). These findings concur with the findings of Quietish et al 1992[11], Al-Arrayed et al 1995[12], Zahedi et al 1998[13].The plausible explanation may be that collagen membrane stabilizes the wound or inhibits or retards the rapid migration of epithelium during healing via contact inhibition thereby providing sufficient time for clot organization and maturation which culminates in greater attachment level[14].
Gingival recession coverage in both Group A and Group B was statistically significant from baseline to 3 months and 6 months post-operative and was non- significant from 3 to 6 months post-operative (Table - 1,2). Difference in gingival recession coverage from baseline to 3 months post-operative in Group A 1.80±0.676 and in Group B 2.53±0.640 and from baseline to 6 months post-operative 1.73±0.704 and 2.53±0.640 respectively which was statistically significant (Table 3). These findings are concurrent with that of Zahedi et al 1998[13], Sheih et al 1997 [15].The resorption of this collagen membrane falls well with in time specified by a study , which has reported that during GTR procedure , bone and / or periodontal cell migration reach their peaks in 2-7 days after surgery , with a decrease in mitotic activity to almost normal levels by the end of 3-4 weeks[16] . Therefore, the length of time that the collagen membrane retains its integrity should be sufficient (3-4 weeks) to allow selective cell repopulation.
Conclusion
Within the limitations of this study bilayer collagen membrane combined with coronally repositioned flap can be used for the treatment of human gingival isolated buccal recession.
References:
1. Kassab MM, Cohen RE.The etiology and prevelance of gingival recession .J Am Dent Assoc 2003;134:220-5.
2. Gottlow J, Nyman S, Karring T, Lindhe J.Treatment of localized gingival recession with coronally displaced flap and citric acid. J Clin Periodontol 1986; 13:57-63.
3. Trombelli L,Minenna L,Farina R,Scabbia A.Guided tissue regeneration in human gingival recessions. A 10 year follow-up study. J Clin Periodontol 2005; 32:16-20.
4. Al-Hamdan K, Eber R, Sarment D, Kowalski C, Wang HL. Guided tissue regeneration based root coverage:Meta analysis. J Periodontol 2003;74:1520-33.
5. Bio-Gide Product Catalogue. Geistlich Biomaterials Innovation of Geistlich. Regeneration by nature.
6. Bunyaratavej P, Wang HL . Collagen membranes . A review . J Periodontol 2001; 72:215-29.
7. Patino MG, Neiders ME, Andreana S, Noble B, Cohen RE. Collagen as an implantable material in medicine and dentistry. J Oral Implantol 2002;28:220-5.
8. Blumenthal NM. A clinical comparison of collagen membrane with e- PTFE membranes in the treatment of human mandibular buccal ClassII furcation defects. J Periodontol 1993;64:925-33.
9. Van Swol RL, Ellinger R, Pfeifer J, Barton NE, Blumenthal N. Collagen membrane barrier therapy to guide regeneration in class II furctions in humans.J Periodontol 1993;64:622-9.
10. Wolff LF, Mullally B. New clinical materials and techniques in guided tissue regeneration. Int Dent J 2000;50:235-44.
11. Quteish D, Dolby AE. The use of irradiated cross linked human collagen membrane in guided tissue regeneration . J Clin Periodontol 1992 ;19:476-84.
12. Al-Arrayed F, Adam S, Moran J. Clinical trial of cross linked human type I collagen as a barrier material in surgical periodontal treatment. J Clin Periodontol 1995;22:371-9.
13. Zahedi S, Bozon C, Brunel G. A 2 year clinical evaluation of a diphenyl phosphorylazide - cross linked collagen membrane for the treatment of buccal gingival recession. J Periodontol 1998; 69:975-81.
14. Minabe M. A critical review of the biologic rationale for guided tissue regeneration . J Periodontol 1991;62:171-9.
15. Shieh AT, Wang HL, O'Neal R,Glickman GN, MacNeil RL. Development and clinical evaluation of a root coverage procedure using a collagen barrier membrane. J Periodontol 1997; 68:770-8.
16. Iglhaut J, Aukhil I, Simpson DM, Johnston MC, Koch G. Progenitor cell kinetics during guided tissur regeneration in experimental periodontal wounds. J Periodontal Res 1988;23:107-17. |