Introduction:
Trigeminal neuralgia is one of the well-recognized oro-facial pains characterized by recurrent episodes of lancinating, sharp, stabbing, electric shock like pain in the Trigeminal nerve distribution.[1],[2] It is also known that some psychological factors are associated with every pain experience which in turn may compromise the physical and mental well-being of the person. The association of psychological factors has been studied in oro-facial pain. But there are few direct studies, especially in relation to trigeminal neuralgia, that have evaluated the role of psychological factors in Trigeminal neuralgia. Hence, the study was planned to evaluate the role of psychological factors in the patients afflicted with this disabling chronic facial neuralgia. The objectives of the study were to assess the sex, age, branch and side distribution in patients with Trigeminal neuralgia; and to evaluate the anxiety and depression scale in patients with Trigeminal neuralgia with an aim of having a better understanding behind the etiological role, these psychological factors might have in the further worsening of or, a decreased outcome to the conventional treatment modalities in patients suffering from Trigeminal neuralgia and to highlight the significance of directing the treatment towards eliminating or, minimizing the facial pain, simultaneously dealing with the psychological component of it which might actually lead to a decrease in response to the conventional therapy given in such pains.
Materials and Methods:
A hospital based cross sectional study was carried out on 60 patients over a span of one year starting from May 2011 to May 2012, which comprised of 2 groups, Group 1, n =30, diagnosed cases of Trigeminal neuralgia and sex and age-matched, controls (group 2, n = 30) between the ages of 40-60 years who had reported to the institutional set-up with a chief complaint not pertaining to chronic pain and were neither suffering from psychosomatic disorders and nor were on any psychoactive medications. These selected controls were actually the subjects who were not suffering from any chronic ailment and were otherwise healthy individuals and who presented with one of the acute inflammatory odontogenic pains that was being considered in their treatments.
Patients who were diagnosed with Trigeminal neuralgia, new or, the ones, who were being treated with carbamazepine, were included in the study. Patients who were diagnosed and / or, suffering from other neurological disorders; those who were in immune-compromised state; and patients with psychosomatic disorders and/or, who were on psychoactive medications were excluded. Patients with Trigeminal neuralgia were selected based upon the Sweet's criteria[3] and the current International Headache Society (IHS) criteria [3].
Sweet's diagnostic criteria for Trigeminal neuralgia (TN) [3]:
1. The pain is paroxysmal;
2. The pain may be provoked by light touch to the face (trigger zones);
3. The pain is confined to the trigeminal distribution;
4. The pain is unilateral;
5. The clinical sensory examination is normal.
International Headache Society criteria (IHS) for Trigeminal neuralgia (TN) [3]:
A - Paroxysmal attacks of pain lasting from a fraction of a second to 2 minutes, affecting 1 or more divisions of the Trigeminal nerve and fulfilling criteria B and C
B - Pain has at least 1 of the following characteristics: (1) intense, sharp, superficial or stabbing; or (2) precipitated from trigger areas or by trigger factors
C - Attacks stereotyped in the individual patient
D - No clinically evident neurologic deficit
E - Not attributed to another disorder
The criteria for symptomatic Trigeminal neuralgia vary slightly from the strict criteria above and include the following [3]:
A - Paroxysmal attacks of pain lasting from a fraction of a second to 2 minutes, with or without persistence of aching between paroxysms, affecting 1 or more divisions of the Trigeminal nerve and fulfilling criteria B and C
B - Pain has at least 1 of the following characteristics: (1) intense, sharp, superficial or stabbing; or (2) precipitated from trigger areas or by trigger factors
C - Attacks stereotyped in the individual patient
D - A causative lesion, other than vascular compression, demonstrated by special investigations and/or posterior fossa exploration
Before selecting the patients for study, details of the study were explained to the patients and written informed consents were obtained for inclusion in the study. The ethical clearance for the study was obtained from the ethical committee appointed by the governing body of the institution.
For each of the subject, a detailed structured case history was recorded and a thorough clinical examination was carried out. The findings were recorded in a prepared proforma which was also including a questionnaire related to Trigeminal neuralgia, the translated versions of General Health Questionnaire and the Hospital Anxiety and Depression scale, for assessment of the psychological morbidity. A shorter 28-item GHQ proposed by Goldberg and Hillier[4] was used as a screening instrument to detect those with a diagnosable psychiatric disorder, consisting of four subscales: somatic symptoms; anxiety and insomnia; social dysfunction; and severe depression. The GHQ-28 was used because of its simplicity in consultant settings and for detecting psychosocial stressors in those with a diagnosable psychiatric disorder. [4] The second scale which we used in our study was Hospital Anxiety and Depression scale which was developed by Zigmond and Snaith which was used for identifying and quantifying the two most common forms of psychological disturbances in patients, namely anxiety and depression. [5],[6] It is generally well accepted by the patients as well as the non-patient group with a 95-100 per cent acceptance rate. [6] The data was subjected to statistical analysis.
Statistical Analysis:
The statistical test used was Mann-Whitney test. The P-value was compared with the level of significance. If P<0.05, the null hypothesis was rejected and alternate hypothesis accepted and vice-versa.
Results:
In comparison between Trigeminal neuralgia patients and the control group, following results were seen:out of 30 Trigeminal neuralgia patients, 16 patients (53%) were males and 14 patients (47%) were found to be females. The mean age of Trigeminal neuralgia patients was estimated as 50.46 years, wherein in male patients, it was seen as 49 years as compared to 52 years for the female patients. The mean age of control was calculated as 44.3 years.
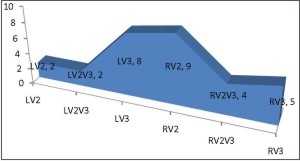 | GRAPH.1 Comparison of the involvement of various branches of the Trigeminal nerve in cases:
 |
In our study, out of 30 patients, 2 patients (7%) were seen to have Trigeminal Neuralgia involving LV2 [L-Left, V2-2nd division, Maxillary branch of Trigeminal Nerve] & LV2, V3 branch [L-Left, V2-2nd division, Maxillary branch of Trigeminal Nerve, V3-3rd division, Mandibular branch of Trigeminal Nerve], 8 patients (27%) LV3 branch [L-Left, V3-3rd division, Mandibular branch of Trigeminal Nerve], 9 patients (30%) involving RV2 branch [R-Right, V2-2nd division, Maxillary branch of Trigeminal Nerve], 4 patients (13%) involving RV2, V3 branch [R-Right, V2-2nd division, Maxillary branch of Trigeminal Nerve, V3-3rd division, Mandibular branch of Trigeminal Nerve] and 5 patients (17%) involving RV3 branch [R-Right, V3-3rd division, Mandibular branch of Trigeminal Nerve] [GRAPH.1]
Higher mean HADS-A [Hospital Anxiety and Depression scale, A= Anxiety],
 | TABLE.1 Comparison of various parameters between cases and controls:
 |
HADS-D [Hospital Anxiety and Depression scale, D= Depression], GHQ-A [General Health Questionnaire, A=Somatic symptoms], GHQ-B [General Health Questionnaire, B=Anxiety / Insomnia], GHQ-C [General Health Questionnaire, C=Social dysfunction], GHQ-D [General Health Questionnaire, D=Depression], and GHQ-T [General Health Questionnaire, T= Total], was observed in cases compared to controlsand the difference was found to be statistically significant (P<0.001), exact P values cited in Table.1 [TABLE.1]. No statistically significant difference was however observed in patients with <50 and ?50 years of age with respect to HADS- A [Hospital Anxiety and Depression scale, A= Anxiety], HADS-D [Hospital Anxiety and Depression scale, D= Depression], GHQ- A [General Health Questionnaire, A=Somatic symptoms], GHQ- B [General Health Questionnaire, B=Anxiety / Insomnia], GHQ- C [General Health Questionnaire, C=Social dysfunction], GHQ-D [General Health Questionnaire, D=Depression] and GHQ -T [General Health Questionnaire, T= Total] (P>0.05), exact P values cited in Table.2 [TABLE.2].
In comparison of various parameters between male and female patients in Trigeminal Neuralgia patients, the mean value of HADS-D [Hospital Anxiety and Depression scale, D= Depression] was found to be higher in the female patients compared to the male patients and the difference was found to be statistically significant (P<0.05), exact P values cited in Table.3. No statistically significant difference was however observed between male and female patients with respect to HADS- A [Hospital Anxiety and Depression scale, A= Anxiety], GHQ- A [General Health Questionnaire, A=Somatic symptoms], GHQ- B [General Health Questionnaire, B=Anxiety / Insomnia], GHQ- C [General Health Questionnaire, C=Social dysfunction], GHQ-D [General Health Questionnaire, D=Depression] and GHQ -T [General Health Questionnaire, T= Total] (P>0.05), exact P values cited in Table.3 [TABLE.3].
Discussion:
The International Association for the
 | TABLE.2 Comparison of various parameters between 50 and 50 age groups in cases
 |
Study of Pain defines Trigeminal neuralgia as 'sudden often unilateral, severe, brief, stabbing, recurrent pains in the distribution of one or more branches of the fifth cranial nerve. [1],[2] Trigeminal neuralgia is an excruciating neuropathic pain with unknown etiology, and it is considered one of the worst causes of suffering associated to pain.[7] There have been many hypothesis proposed on etio-pathogenesis of the neurological disorder. The most accepted theory is demyelination of the nerve resulting in short circuiting of impulses in the pathways of Trigeminal nerve. [2],[7],[8]
In our study, we found that Trigeminal neuralgia involving right side of the face was more common than the left side and the mean age of the patients was 50 years which was in accordance with the study conducted by Katusic et al [9] Cruccu G et al [10] and Neto HS et al [11].
Trigeminal neuralgia has been seen to be an extremely disabling illness but unfortunately the medical line of treatment does not give 100% relief and surgical approach has got its own inherited disadvantages, one of them being anesthesia on the involved side.Initially, administration of anticonvulsant drugs was the treatment of choice for trigeminal neuralgia. There are now a variety of other effective treatments, both pharmacologic and
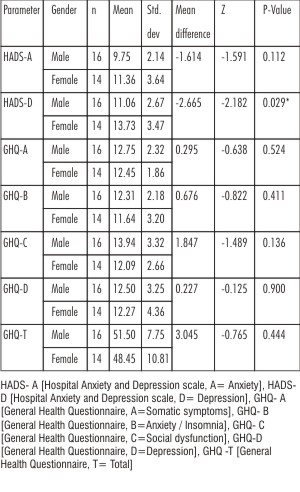 | TABLE.3 Comparison of various parameters between males and females in cases:
 |
surgical. However, none of them provides a permanent cure. [12],[13] So the prolonged stress of chronic pain may lead to learned helplessness, withdrawal, lethargy, feelings of worthlessness, and sometimes guilt and anxiety. [13],[14] Furthermore, it is estimated that as many as 50% of patients suffering from chronic pain are depressed. In the present study, GHQ and Hospital Anxiety and Depression scale [HADS] have shown significant findings in Trigeminal neuralgia patients which was in accordance with the study conducted by Castro et al [13] who concluded the association of psychological disorders with Trigeminal neuralgia.
Charlotte Feinmann [14] reported in his study the need for the evaluation of psychiatric and psychological considerations in the management of Trigeminal neuralgia patients. However, there are no such studies in the literature assessing the psychiatric or, personality problems or, disorders associated in patients suffering from this chronic pain syndrome.
Argoff et al [15] in their review suggested that the treatment of neuropathic pain may be complicated by co-morbid conditions such as depression, and anxiety. The interrelationship between the neuropathic pain state and these co-morbidities is however complex: co-morbid conditions exacerbate pain, and in turn, pain exacerbates the co-morbid conditions. Because co-morbidities can negatively impact response to pain treatment, healthcare providers should assess co-morbidities as part of the diagnostic work-up, and management strategies should be designed to treat the whole patient, not just the pain. Theoretically, therapies that not only reduce pain, but also improve sleep and reduce anxiety and depression can provide multiple benefits without the risk of increased side effects inherent in combination therapy.[14],[15] Anticonvulsants and antidepressants have demonstrated efficacy in improving neuropathic pain and positively impacting co-morbid sleep and mood disturbances. [12],[13]
Conclusion:
For patients suffering from recalcitrant, chronic pain syndromes, where surgical or, pharmacological treatment have not provided sustained pain relief or, the side effects associated with the pain relief are unacceptable, psychological approaches to pain management become the preferred option. This study highlights the significance of such additive therapy that should be considered in these sets of patients to improve response to conventional modes of treatments in addition to improving the overall well-being of the patients.
Recommendation(s):
The study also paves way for future studies with larger sample sizes and adequate representation of patients of both the genders from different age groups assessing the various psychological parameters in these patients.
The study also paves way for future studies with larger sample size that correlate the severity and duration of this disabling chronic facial neuralgia with the psychological parameters assessed in the study that could not be covered in the present study.
The study infact raises a question on the conventional modality of treatments underlying the significance of the simultaneous management of psychological factors of the patients suffering from chronic pains especially in the cases where age is a factor that rules out the possibility of surgical approaches and most of the patients are left to bear the enigma of chronic pains which further initiates a vicious cycle of an increasing psychological compromise and a never lasting and indeed worsening life bearing the burden of chronic pain. The study indeed paves way for future studies with a systematic approach with simultaneous psychological intervention in these patients for an effective and better management of these patients who are largely left to live a life full of the agony of pain.
Acknowledgement:
We thank all the people who directly and indirectly contributed in carrying out this study and in the preparation and revision of the manuscript.
References:
1. Krafft RM. Trigeminal Neuralgia. Am Fam Physician 2008;77(9):1291-1296.
2. Prasad S, Galetta S. Trigeminal Neuralgia: Historical notes and current concepts. The Neurologist 2009;15:87-94.
3. White JC, Sweet WH. Pain and the neurosurgeon. Springfield(111):Charles C.Thomas;1969. Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd ed. Cephalalgia. 2004;24(Suppl 1):9-160.
4. Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Psychol Med 1979;9:139-145.
5. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361-370.
6. Herrman C, Scholz KH, Kreuzer H. Psychologisches Screening Von Patienten einer kardiologische Akutlinik mit einer deutschen Fassung der "Hospital Anxiety and Depression" (HAD)-Skala. Psychother Psychosom Med Psychol 1991;41:83-92.
7. Benoliel R, Eliav E. Neuropathic orofacial pain. Oral Maxillofac Surg Clin N Am 2008;20:237-254.
8. Merskey H, Bogduk N. Classification of chronic pain. Descriptors of chronic pain syndromes and definitions of pain terms. Seattle: International Association for the Study of Pain Press, 1994;59-71.
9. Katusic S, Beard CM, Bergstralh E, Kurland LT. Incidence and clinical features of trigeminal neuralgia, Rochester, Minnesota, 1945-1984. Ann Neurol. 1990;27(1):89-95.
10. Cruccu G, Biasiotta A, Galeotti F et al. Diagnosis of trigeminal neuralgia: a new appraisal based on clinical and neurophysiological findings. In: Cruccu G, Hallett M, eds. Brainstem Function and Dysfunction. Amsterdam, the Netherlands: Elsevier; 2006:171-186.
11. Neto HS, Camilli JA, Marques MJ. Trigeminal neuralgia is caused by maxillary and mandibular nerve entrapment: greater incidence of right sided facial symptoms is due to the foramen rotundum and foramen ovale being narrower on the right side of the cranium. Med Hypotheses. 2005;65(6):1179-1182.
12. Siddiqui MN, Siddiqui S, Ranasinghe JS, Furgang FA. Pain management: Trigeminal Neuralgia. Hospital Physician 2003:64-70.
13. Castro AR, Siqueira SR, Perissinotti DM, Siqueira JT. Psychological evaluation and cope with trigeminal neuralgia and temporo-mandibular disorder. Arq Neuropsiquiatr. 2008 Sep;66(3B):716-9.
14. Feinmann C, Psychiatric and psychological management considerations associated with nerve damage and neuropathic trigeminal pain. Journal of Oro-facial Pain 2004;18:360-365.
15. Argoff, Charles E. The Coexistence of Neuropathic Pain, Sleep, and Psychiatric Disorders: A Novel Treatment Approach. Clinical Journal of Pain 2007;23(1):15-22. |