Introduction :
Laser technology has evolved in recent years and has been incorporated into most dental treatment modalities in different forms. Competition amongst the manufacturers of dental laser technologies has revolutionized the varied application and maneuverability of the laser handpiece for use during hard and soft tissue treatments. Lasers have transformed the working style and image of dentist clinician as a more precision oriented and efficient and updated clinician. However, the success of any procedure using laser is solely the result of knowledge, understanding and adequate experience regarding lasers[1],[8].
History :
Though the credit for discovering the therapeutic use of lasers goes to Mainman et al (1960), lasers were brought to general dental practice in 1989 by Dr. William and Terry Myers, who modified an ophthalmic Nd:YAG laser for dental use[3]. This unit pioneered the development of lasers dedicated to the field of dentistry. Since then, a number of laser wavelengths have been brought to the profession for various procedures.
Mechanism of Action:
The word laser is an acronym for Light Amplification by Stimulated Emitted Radiation. It is a device that transforms light of various frequencies into an intense, small, and nearly non-divergent beam of monochromatic radiation, within the visible range[3].
Light - Laser light used for dental procedures is a form of electromagnetic energy that has four characteristic features - monochromatic, collimation, coherency, and efficiency.
Amplification - This electromagnetic energy is generated by excitation of an active medium like argon ,CO2, yttrium, aluminum, gallium ,neodymium, or erbium that provide the source of energy which is then amplified by mirrors and emerges as laser light.
Stimulated Emission - The term 'stimulated emission' has its basis in the quantum theory of physics and is further conceptualized as relating to atomic architecture by Niels Bohr. The mirrors at each end of the active medium reflect the photons back and forth to allow further stimulated emission of the laser beam.
Radiation - Radiation refers to the light waves produced by the laser as a specific form of electromagnetic energy[2],[3].
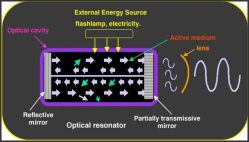 | Fig.1: Laser Unit
 |
Laser-tissue interaction:
Photobiological effects of laser light with tissue include absorption, transmission, scattering, and reflection. The amount of energy that is absorbed by the tissue depends on the tissue characteristics, such as pigmentation and water content[3]. Argon lasers are highly attenuated by hemoglobin, Diode and Nd:YAG by melanin. Lasers of CO2 and Erbium family are readily absorbed by hydroxyapatite and water, hence has great affinity for tooth structure and bone. Argon, diode and Nd:YAG lasers have greater penetration into the tissues as compared to CO2 and erbium lasers which act on the outer surface[2]. These properties of lasers are exploited for performing hard and soft tissue procedures. The property of reflection is utilized in caries detection to measure the degree of sound tooth structure. The fourth effect is a scattering of the laser light, which is useful in facilitating the curing of composite resin. It is essential, therefore, for the clinician to choose the laser wavelength that will be absorbed maximally by the target tissue and to regulate the power parameters to create maximal surgical effect while not producing any unwanted collateral damage[11].
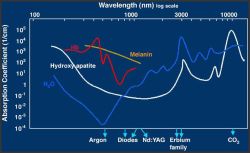 | Fig.2: Relative Absorption Levels Of Different Lasers
 |
Application of lasers in prosthodontics :
1. Pre-prosthetic surgeries during prosthetic reconstruction
2. Laser tooth preparation
3. Soft tissue management
4. Laser scanning
5. Implant recovery
6. Lasers used in dental lab procedures
7. Laser sintering[4]
Pre-Prosthetic Surgeries:
The successful fabrication of removable full and partial dentures mainly depends on the preoperative evaluation and preparation of the supporting hard and soft tissue structures. Lasers can be used to perform most preprosthetic surgeries[11].
These procedures include -
-tuberosity reduction,
-osseous recontouring of residual ridge and sockets ,
-removal of bony spicules, tori and exostoses,
-removal of inflamed and hyperplastic tissue or any soft tissue lesions,
Wigdor et al[9] described the advantages of lasers over conventional surgical procedures as follows:
1. Dry and bloodless surgery
2. Instant sterilization of the surgical site
3. Reduced bacteremia
4. Reduced mechanical trauma
5. Minimal postoperative swelling scarring
6. Minimal postoperative pain.
 | Fig.3: Pre-prosthetic Surgery Using Laser
 |
Laser Tooth Preparation :
The new age dentistry and today's patient demands painless and stress free dental treatment, and lasers for tooth preparation is the answer to this. The procedure is as follows -
1. Crown preparation is done at maximum setting for cutting enamel (6 watts, 90% air, 10% water), defocused for 30 seconds to 1 minute to anaesthetize the tooth first.
2. Preparation is begun by starting on the buccal surface and making depth cuts of 2- 2.5mm , and then these reference points are connected .
3. The laser power is then further reduced to smoothen the surface of the prepared tooth[4].
Advantages of laser tooth preparation include[5] -
-
No local anaesthesia
-
Reduced clinical time
-
More comfortable procedure
-
Heat generated is minimal
-
No vibration
-
No smear layer formation
-
Precise , pin-point accuracy
-
Conservative preparation
Soft Management :
The pivotal step of gingival retraction before making an impression for fixed prosthesis is made simple, easy , pain free, quick with the use of quartz fibre of 200-320um wavelength at sublative power levels - 100mJ per 10-20 pulses per second. The laser tip is placed below the height of the gingival crevice, and the tissue is 'ledged' to expose the margin of the preparation. This procedure is technique sensitive and must be done carefully to prevent inadvertent damage to the tooth[5],[10].
Also, the use of soft tissue diode laser is advocated for gingival recontouring of ovate ponitc site / implant-supported fixed prosthesis to create an appropriate emergence profile. This helps improve aesthetics and increases the ease of postoperative oral hygiene maintenance. The laser (2 to 10pulses per second) is used in the focused mode and aimed vertically down the tooth surface towards the tissue avoiding contact with the tooth surface[11].
Implant Recovery :
The two staged implant placement method necessitates making of the final impression for the prosthesis after flap reflection. Instead, erbium/ holmium family of lasers can be used to perform dry mucosal ablation needed to expose the implant ensuring minimal bleeding, trauma to the flap reflected and minimal tissue shrinkage[11]. One of the most interesting uses of lasers in implant dentistry is the possibility of salvaging ailing implants by decontaminating their surfaces with laser energy. Diode lasers were used in a study by Bach et al , who found a significant improvement in the 5-year survival rate when integrating laser decontamination into the approved treatment protocol[7].
 | Fig.5: 2nd Stage Surgery Using Laser
 |
Laser Scanner :
Optical scanner is a hand held acquisition camera which uses highly visible blue light LED (light emitting diode) to capture digital impressions. These intra-oral scanners capture the 3D geometry of tooth preparation and other relevant structures with the help of a camera placed in a wand which is just 13mm wide, thus maximizing the maneuverability inside the mouth[8].
Laser Welding :
Laser welding is an effective and routinely used method for various dental lab procedures against the conventional soldering. Advantages of laser welding:
1. High bond strength and corrosion resistance
2. Reduced oxidation when argon gas is used for welding.
3. Minimal heat generation and greater precision in processing than with soldering or other techniques[6].
Laser Sintering :
The face of the next generation maxillofacial prosthodontics is aptly described by laser sintering. This technology is a powder base layer-by-layer manufacturing technique in which a substrate is locally heated by laser radiation so that the particles solidify to form a 3D structure. This technology is being used nowadays for plastics, metals, metal alloys, and ceramics to fabricate any prosthesis[12]. Laser sintering technology is pandora box that opens up more complex and high-tech tools like rapid prototyping and streolithography for making maxillofacial prosthesis, surgical and radiographic stents[13].
Conclusion :
The potential for laser dentistry to improve dental procedures rests in the dentist's ability to control the power output and the duration of exposure on both hard and soft tissues, allowing for treatment of a highly specific area of focus without damaging surrounding tissues. Each wavelength and each device has specific advantages and disadvantages.The clinician who understands these principles can take full advantage of the features of lasers and can provide safe and effective treatment[1].
References :
1. Aesthetic dentistry :A clinical approach to techniques and materials. - Ascheim and Dale ; 2nd edition.
2. Robert A. Convissar . 'The biologic rationale for the use of lasers in dentistry.' Dent Clin N am 2004; vol48, pg.771-794.
3. Donald J.Coluzzi . ' Fundamentals of dental lasers : science and instruments.' Dent Clin N am 2004; vol48, pg.751-770.
4. Steven D.Spitz. 'Laser in Prosthodontics: Clinical Realities of a Dental Laser in a Prosthodontic Practice.'; Alpha Omegan , Vol101, number4, pg188-194.
5. Steven Parker. 'The use of lasers in fixed prosthodontics.' Dent Clin N am 2004; vol48, pg.971-998.
6. N.Baba, I.Wantanabe. ' Penetration depth into dental casting alloys by Nd:YAG Laser.' Journal of Biomaterials Materials Research (PartB) : Applied Biomaterials ; Vol72 B ; Issue 1, pg 64-68.
7. Emile Martin. 'Laser in dental implantology.'; Dent Clin N am 2004; vol48, pg.999-1015.
8. Timothy C.Adams. 'Lasers in aesthetic dentistry.' Dent Clin N am 2004; vol48, pg.833-860.
9. Gabi Kesler. 'Clinical Applications of laser during removable prosthetic reconstruction.' Dent Clin N am 2004; vol48, pg.963-969.
10. B.Gokce, B.Ozpinar ,C.Artunc , G.Aksoy. 'Laser use vs. handpiece for tooth preparation : A preliminary in vitro study.'; Journal of Laser Applications, May 2009, Vol21, Issue 2, pg63-66.
11. Pick RM , Colvard MD. 'Current status of lasers in soft tissue dental surgery.' J Periodontol 1993, Vol64 , Issue 7, pg.589-602.
12. F.Klocke, C.Ader. 'Direct Laser Sintering of Ceramics.' ;Prod. Eng. Res. Develop. 2007, vol1, pg279-284.
13. Peter Regenfuss, Robby Ebert , Horst Exner . 'Laser Micro Sintering: a versatile instrument for the generation of microparts.' ;Laser Technology Journal, Jan 2007, Vol 1; pg 26-31.
14. Lingfei Ji, Yijian Jiang . 'Laser sintering of transparent tantalum pentoxide dielectric ceramics.' Dental Materials, June 2006, Vol60, Issue 12, pg1502-1504.
15. Deppe H, Horch HH, Henke J, Donath K. 'Peri-implant care of ailing implants with carbon- dioxide layer.'; Int J Oral Maxillofac Implants 2001, Vol 16, Issue5 , 659-667. |