Introduction
Periodontology has a rich background of research and scholarship. The substantial and extensive periodontal information base, developed over the years, has provided a rational basis for choosing the best treatment for patients. Appraisal of this information has being an on-going and continuous effort by the American Academy of Periodontology (AAP) to ensure that the most accurate and efficacious concepts and technologies are used to provide care and stimulate innovation [1]. Evidence-based dentistry (EBD) is the integration and interpretation of the available current research evidence, combined with personal experience. It allows dentists, as well as academics researchers, to keep update of the new developments and to make decisions that should improve their clinical practice. The term "Evidence-based Medicine" (EBM) from which evidence-based dentistry has followed, is relatively new (started in early 1900's) and is defined as "the integration of the best research evidence with clinical expertise and patient values [2]." The term was coined by the clinical epidemiology group at McMaster University in Canada. American Dental Association has defined EBD as: "an approach to oral health care that require the judicious integration of systematic assessments of clinically relevant scientific evidence, relating to the patients oral and medical condition and history, together with the dentist's clinical expertise and the patient's treatment needs and prefernces [3]." The need of EBD is important for the dentist, especially with regards to patient safety, and for dentists to be able to keep up to date with developments in diagnosis, prevention and treatment of oral disease, and newly discovered causes of disease. Advances in dentistry are usually first reported in dental journals, and in order to keep up with new research, healthcare professionals need to feel confident that they can read and evaluate dental papers. EBD is founded on clinical research. The ultimate beneficiaries of EBD are members of the public, who will reap the rewards of better care. The internet allows patients, as well as professionals, access to health care information. The public, however, does not have the tools to evaluate the data adequately and must rely on their educated dentists to help sort fact from fiction. Patients will be more educated, more involved in their treatment decisions, and more appreciative of quality care. Dentists will also be benefitted from EBD. Instead of conducting free product testing for dental product manufacturers, practitioners will have at their disposal more valid research on which to predicate their clinical decisions. Researchers will benefit by being called upon to do the clinical testing necessary before new products are placed on the market.
Evidence-based periodontology aims to facilitate the efficient use of research data, accelerating the introduction of the best research into patient care. A useful definition of evidence-based health care has been proposed by Muir Gray: "An approach to decision making in which the clinician uses the best evidence available in consultation with the patient, to decide upon the options that suits that patient best [4]." It is a tool to support decision making and integrating the best evidence available with clinical practice, and is composed of various levels, which starts with the recognition of a knowledge gap. From the knowledge gap comes a focused question that leads on to a search for relevant information. [5].
Evidence-based periodontology is the application of evidence-based health care
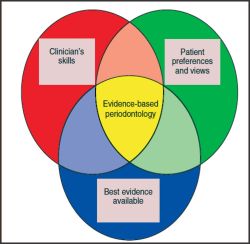 | Fig. 1 Evidence Based Dentistry for Effective Practice
 |
to periodontology. It is a tool to support decision making and integrating the best evidence available with clinical practice (Fig.1). Evidence based periodontology is an approach to patient-care and nothing more. It cannot provide answers if research data do not exist (other than using expert opinion) and it cannot substitute for highly developed clinical skills.
Advantages of evidence-based approach (EBA) compared with other assessment methods
The EBA is: [6]
-
Objective.
-
Scientifically sound.
-
Patient-focused.
-
Incorporates clinical experience.
-
Stresses good judgement.
-
Is thorough and comprehensive.
-
Uses transparent methodology.
Terminologies used in evidence-based approach [7]
Systematic review: Review of a clearly formulated question that attempts to minimize bias using systematic and explicit methods to identify, select, critically appraise and summarize relevant research.
Interpretation: It is the process by which qualitative methods seek to identify subjective meaning of a phenomenon.
Process: Qualitative methods used to identify the social processes that underlie healthcare.
Interaction: Encounter between physician and patient helps in bringing together conflicting views of health and illness.
Bias: Bias is a systematic error. It leads to results which are consistently wrong in one/other direction. Bias leads to incorrect estimate of the effect of a risk factor/exposure.
Confounding: Describes the situation where an estimate of the association between an exposure and the disease is mixed up with the real effect of another exposure on the same disease, the two exposures being the same.
Confidence Interval: A method of statistical inference that allows statement to be made about the publication using data from the sample.
Odds ratio: Ratio of exposure among cases to exposure among controls.
Chance: Chance/sampling error plays a role in most studies of humans, since it is rarely if ever possible to include an entire population in an investigation. We therefore attempt to infer information about the population on the basis of information obtained from representative samples drawn from the population.
Naturalism: Qualitative methods seek to understand health and health-related behaviour in its every day or natural context [7].
The Development of Evidence Based Periodontology
Evidence-based periodontology is built upon developments in clinical research design throughout the 18th, 19th and 20th centuries [8],[9],[10],[11]. EBM has only been known for just over a decade One of the earliest to take up the challenge in periodontology (in fact in oral health research overall) was Alexia Antczak Bouckoms in Boston, USA. She and her colleagues challenged the methods and quality of periodontal clinical research in the mid-1980s and set up an Oral Health Group as part of the Cochrane Collaboration in 1994. The editorial base of the Oral Health group subsequently moved to Manchester University in 1997 with Bill Shaw and Helen Worthington as co-ordinating editors. The first Cochrane systematic review in periodontology was published in 2001 and researched the effect of guided tissue regeneration for infrabony defects [11]. Periodontology held by the American Academy of Periodontology included elements of evidence-based healthcare, supported by Michael Newman at UCLA. The 2002 European Workshop on Periodontology became the first international workshop to use rigorous systematic reviews to inform the consensus. The workshop was organized by the European Academy of Periodontology for the European Federation of Periodontology, under the chairmanship of Professor Klaus Lang. Most recently, the International Centre for Evidence-Based Oral Health was launched in 2003 to produce high quality evidence-based research with an emphasis on, but not limited to, periodontology and implants and to provide generic training in systematic reviews and research methods [5].
Clinical Relevance
One of the barriers to the application of research findings in clinical practice is the way that results are often presented. Typically, a mean value will be published, based on a statistical analysis comparing experimental groups. Such a value in conjunction with its associated 95% confidence interval is useful to determine whether there is a statistically significant difference between groups and will often be a requirement of a study designed for regulatory approval. However, this type of analysis is not designed to provide information about the probability of achieving a certain outcome were the reader to apply it in practice. Such an outcome could include achieving a health benefit or preventing further disease [5]. One approach to analysing and presenting data in a more clinically useful format is to calculate the number needed to treat (NNT). This is the number of patients that would need to be treated to achieve a stated benefit (NNTb) or to avoid a stated harm (NNTh). It is derived from a dichotomous outcome such as the proportion of sites achieving at least two mm gain in attachment. For the GTR meta-analysis, and using this benefit, the NNTb is eight. In other words, for every eight patients treated with GTR, you can expect one to have at least two mm more gain in clinical attachment than if you had used an access flap (95% confidence interval) [5].
Evidence-Based Periodontology v/s Traditional Periodontology
Evidence-based periodontology uses a more transparent approach to
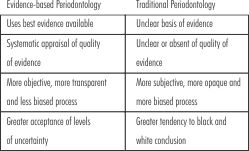 | Table 1: Comparison Of Evidence-based Periodontology V/s Traditional Periodontology
 |
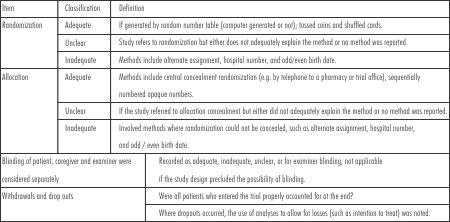 | Table 2: Quality Assessment Checklist For Randomized Controlled Trials In Periodontology
 |
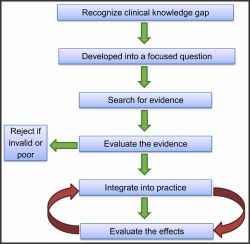 | Fig. 2 Steps of Evidence-Based Periodontology
 |
acknowledge both the strengths and the limitations of the evidence. An appreciation of the level of uncertainty or imprecision of the data is essential in order to offer choices to the patient regarding treatment options. Evidence-based periodontology also attempts to gather all available data and to minimize bias in summarizing the data. Furthermore, evidence-based periodontology acknowledges explicitly the type or level of research on which conclusions are drawn. However, one aspect that influences the reliability of the data is the control of bias. Bias is a collective term for factors that systematically distort the results of research away from the truth. Different research designs offer different possibilities for the control of bias and therefore vary in their reliability [5]. The comparison between evidence based periodontology and traditional periodontology is shown in Table 1.
The similarities between the two are: [12]
-
High value of clinical skills and experience
-
Fundamental importance of integrating evidence with patient values.
The Components of Evidence-Based Periodontology
Evidence-based periodontology starts with the recognition of a knowledge gap (Fig.2). From the knowledge gap comes a focussed question that leads on to a search for relevant information. Once the relevant information is located, the validity of the research needs to be considered in two broad areas. Firstly, is the science good (internal validity)? Internal validity focuses on the methodology of research. Secondly, can the findings be generalized outside of the study (external validity)? External validity might be affected by the way treatment was performed. After locating and appraising the research, the results then need to be applied clinically, or at least included in a range of options. Finally, the results in clinical practice need to be evaluated to reveal whether the adopted technique achieved the expected outcome[5]. For rigorous systematic reviews, independent reviewers usually undertake quality appraisal in duplicate and checklists are frequently employed for this purpose. An example by Montenegro et al (2002) is shown in Table 2 [12].
Evidence-based approach (EBA) in periodontal therapy will be dealt under the following topics:
-
EBA and mechanical nonsurgical pocket therapy
-
Effect of smoking on Non-surgical pocket therapy (NST)
-
EBA in periodontal regeneration
-
EBA and mucogingival surgery
-
EBP and open flap debridement
Evidence-based approach and mechanical nonsurgical pocket therapy
-
A total of nine reviews were searched for the best evidence [14].
-
NST was found to have a positive effect with the exception of pockets <3 µm.
-
Patient, environmental, and operator factors affect therapy delivery.
-
No difference was found between the effect of hand and machine-driven instruments.
-
Machine-driven instruments were faster than hand-driven instruments.
Conclusions from 1996 world workshop on periodontics
Chemical Plaque Control [15]
-
The various antiplaque and/or antigingivitis agents do not offer a substantial benefit for the treatment of periodontitis.
-
They may however contribute to the control of gingival inflammation that exists with periodontitis.
-
Supragingival irrigation may be used as an adjunct to tooth-brushing and has been shown to aid in the reduction of gingival inflammation.
-
Even when subgingival irrigation is used, the evidence shows that there are no clear substantial long-term benefits for the treatment of periodontitis.
Antibiotic Therapy and Periodontics
The risk-benefit ratio indicates that systemic antibiotics should not be used for the treatment of gingivitis and common forms of adult periodontitis. But evidence suggests that systemic antibiotics may be useful in aggressive forms of periodontitis [15].
Local Delivery of Antimicrobial Agents [15]
-
There was modest gain in clinical attachment level and decrease in probing depth and gingival bleeding.
-
A few side effects were demonstrated namely, transient discomfort, erythema, recession, allergy, and rarely candida infection.
Effect of smoking on nonsurgical therapy
Systematic review of the effect of smoking on NST was conducted by Labriola et al. [16] Search strategy included Medline, Embase and Central. Study design was controlled clinical trial.
The outcomes were:
-
There was reduced pocket depth reduction in smokers, compared with non-smokers.
-
There was no significant difference in the change of Clinical Attachment Level (CAL) between smokers and non-smokers.
-
The reason could be that the increased vasoconstriction in peripheral blood vessels of smokers leads to decrease in bleeding and edema. Also, smokers would have less potential for resolution of inflammation and edema within the marginal tissues and therefore less potential for gingival recession.
Evidence-based approach in periodontal regeneration
Guided Tissue Regeneration
The study population included chronic periodontitis patients in subjects 21 years or older. The outcomes assessed were:
Short-term clinical outcomes
It included soft tissue changes such as increased CAL and decreased PPD.
Long-term clinical outcomes
It included disease recurrence and tooth loss.
Patient-centered outcomes
It included various factors such as ease of maintenance, change in esthetics, p/o complications, cost/benefit ratio, and patient well-being.
The meta-analysis done by Needleman et al [17] and Murphy et al [18], revealed that:
1. When compared with open flap debridement (OFD), guided tissue regeneration (GTR) showed increase in CAL, decrease in PPD, and defect fill.
2. When GTR with bone substitutes was compared with GTR alone, the results were similar.
3. No evidence was found for difference in use of ePTFE versus bioabsorbable membranes.
4. Long-term clinical outcomes/patient-centered outcomes could not be determined due to lack of available data. Heterogeneity was large and bias could not be eliminated.
Evidence on mucogingival therapy
Carlo Clauser [19] in his meta-analysis found that:
All the surgical procedures allow complete root coverage.
Connective tissue grafting achieves complete root coverage more frequently than does GTR.
The probability of complete root coverage is high if the initial recession is shallow, irrespective of the surgical procedure employed.
The probability of achieving complete root coverage decreases dramatically as the initial recession depth increases.
Evidence-based approach and open flap debridement
Systematic reviews were conducted by Heitz Mayfield et al [20] and Antczak et al [21].
Clinical implications of the whole review regarding open flap debridement
If pocket depth reduction is the main aim, surgical treatment is the treatment of choice. If increase in clinical attachment level gain is the main aim, nonsurgical therapy is of more benefit for shallow and moderate pockets and surgical therapy is the treatment of choice for deep pockets. Predictability of treatment outcome at sites with furcation involvement or angular defect is unclear.
Need for studies reporting individual patient data [19]
Individual patient data (IPD) is considered the gold standard for the following reasons:
-
Only IPD can provide the information needed to investigate the role of various factors in different clinical situations.
-
If data are only available on a trial level and not for individual sites, it is impossible to individually relate the baseline recession depth of a site to the treatment results of that specific site.
What is the significance of individual patient data? [19]
The clinical trial usually answers yes or no, but the rest of the information remains unused. The lost information would be very valuable in exploring data in order to raise few sensible questions and to design new trials. Therefore at least the following issues are relevant:
-
The possibility of exploring data from different viewpoints.
-
The possibility of analysing the same data in different ways.
-
The possibility of replicating the study to reduce the margin of doubt that cannot be eliminated.
-
The possibility of an in-depth check of the reliability of the data collection and analysis.
-
The possibility of sizing new experiments in an economically sound way by saving or designing expensive pilot studies more rationally.
-
The possibility of computing the confidence intervals of some statistics those are of interest to the reader.
New pathway for scientific articles [19]
-
Submittal of a 'conventional' paper with summarized data.
-
Provisional acceptance: The author could even choose between submitting the original set of data prior to publication or accept the challenge of confronting the editor's criticism of the published paper.
-
The conventional paper is published in the journal. The original data and other elaborations by the authors are published on the journal's internet site.
-
A forum to promote discussion of the article via email could be created and new ideas could certainly be a valuable by-product.
How to Critically Appraise?
-
It is necessary to consider those factors that may affect the outcome of a study, will vary according to both the topic of research and the study designs employed, so it is not possible to devise a single system that will be appropriate for every occasion.
-
Some reviewers have attempted to devise composite scales that give scores for the various quality domains [22]. These scores are then summed to an overall summary measure for the study as a whole.
-
An alternative approach is to appraise each quality component separately [23]. The results of the quality appraisal are used to assess the value of the evidence and to aid clinicians and reviewers in their efforts to place the evidence into context.
Conclusions
The principles of evidence-based healthcare provide structure and guidance to facilitate the highest levels of patient care. There are numerous components to evidence-based periodontology including the production of best available evidence, the critical appraisal and interpretation of the evidence, the communication and discussion of the evidence to individuals seeking care and the integration of the evidence with clinical skills and patient values. Evidence-based healthcare is not an easier approach to patient management, but should provide both clinicians and patients with greater confidence and trust in their mutual relationship.
References
1. Micheal G Newman, Jack G Caton, John C Gunsolley: The use of evidence-based approach in a periodontal therapy contemporary science workshop. Ann Periodontol 2003; 8:1-11.
2. Sackett DL, Strauss SE, Richardson WS, et al: Evidence-based medicine: how to practice and teach EBM, London, 2000, Churchill Livingstone.
3. Berthold M. Association moves on EBD. Available at: http://www.ada.org/prof/resources/topics/evidence based.asp. Accessed October 22, 2003.
4. Gray JAM. Evidence-based Healthcare. Edinburgh: Churchill Livingstone, 1997.
5. Needleman I, Moles DR, Worthington H. Evidence-based periodontology, systematic reviews and research quality. Periodontology 2000 2005; 37:12-28.
6. Newman M, Caton J, Gunsolly J. Evidence?based periodontology. Ann Periodontol 2003; 8:1.
7. Evidence-based approach. Dent Clin North Am 2002; 46:54-62.
8. Mathews JR. Quantification and the Quest for Medical Certainty. Princeton: Princeton University Press, 1995.
9. Needleman IG. Introduction to evidence based dentistry. In: Clarkson, J, Harrison, JE, Ismail, AI, Needleman, IG, Worthington, H, eds. Evidence Based Dentistry for Effective Practice. London: Martin Dunitz, 2003; 1-17
10. Rangachari PK. Evidence-based medicine: old French wine with a new Canadian label? J R Soc Med 1997; 90:280-284.
11. Swales J. The troublesome search for evidence: three cultures in need of integration. J R Soc Med 2000; 93:402-407.
12. Montenegro R, Needleman I, Moles D, Tonneti M. Quality of RCTs in periodontology - a systematic review. J Dent Res 2002; 81:866-870.
13. Needleman IG, Giedrys-Leeper E, Tucker RJ, Worthington HV. Guided tissue regeneration for periodontal infra-bony defects (Cochrane Review). The Cochrane Library. Oxford: Update Software. http://www.update-software.com/clibhome/
14. Suvan JE. Effectiveness of mechanical nonsurgical pocket therapy. Periodontology 2000; 37:49-50.
15. Jeffcoat MK, McGuire M, Newman MG. Evidence based periodontal treatment: Highlights from the 1996 World Workshop in Periodontics. J Am Dent Assoc 1997; 128:713-23.
16. Labriola A, Needleman I, Moles DR. Systematic review of the effect of smoking on nonsurgical periodontal therapy. Periodontology 2000 2005; 37:124-37.
17. Needleman IG, Giedrys-Leeper E. Guided tissue regeneration for periodontal infra?bony defects. Cochrane Database Syst Rev 2001; 2:CD001724.
18. Murphy KG, Gunsolley JC. GTR for the treatment of periodontal intrabony and furcation defects: A systematic review. Ann Periodontol 2003; 8:266-302.
19. Clauser C, Nieri M, Franceschi D. Evidence-based mucogingival therapy, Part 2: Ordinary and individual patient data meta-analysis of surgical treatment of recession using complete root coverage as the outcome variable. J Periodontol 2003; 74:741-56.
20. Heitz-Mayfield L, Trombelli L, Heitz F. A systematic review of the effect of surgical debridement Vs non-surgical debridement for the treatment of chronic periodontitis. J Clin Periodontol 2002; 29:92-102.
21. Antizack A, Joshipura K, Burdick E. Meta-analysis of surgical Vs nonsurgical methods in the treatment of periodontal diseases. J Clin Periodontol 1993; 20:259-68.
22. American Academy of Periodontology. Proceedings of the 1996 World Workshop in Periodontics. Lansdowne, Virginia, July 13-17, 1996. Ann Periodontol 1996; 1:1-947.
23. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996; 17:1-12. |