Introduction
Long term success in implant dentistry requires the evaluation of more than 50 dental criteria, many of which are unique to this discipline.[1] The dentist should determine the prosthodontics needs and desires of the patient first, relative to the missing teeth. If natural teeth are in proper position to serve as potential abutment support, the traditional methods must be followed for restoring the dentition. If no teeth are present in the area of the abutment for the intended prosthesis, dentist determines the implant ideal and optional positions. The most important criteria for implant placement are available bone. Greenfield already appreciated the importance of available bone in implant region in 1913.[2] The amount of available bone for implant, however, is difficult to evaluate exactly since the bone resorption process occurs soon after tooth extraction, particularly in the posterior maxilla region.
Characteristic bone changes occurs after tooth loss[3],[4],[5].The amount of bone loss that occurs during the first year after tooth loss is almost 10 times greater than in the following years. A 25% decrease in bone width occurs within the first year and 40% within the first 1 to 3 years. [6] As a result, the residual ridge shifts palatally in the maxilla and lingually in the mandible at the expense of the buccal cortical plate. Ratio of anterior maxillary bone loss to anterior mandibular bone loss is 1:4. The posterior edentulous mandible resorbs at a rate about 4 times faster than the anterior edentulous mandible.
Once the final prosthesis type has been determined, the next consideration is the required size, number, and location of endosseous implants necessary to satisfy the prosthodontic requirements. The primary criterion for proper implant support is the amount of available bone and is evaluated during the clinical examination and radiographic assessment.
Material And Methods
An exhaustive search was undertaken to identify published litereature related to evaluation of available bone by using key words .The search of MEDLINE database included all publications from 1983-2005. Selected articles were then obtained and reviewed.
Discussion
Available bone describes the volume of bone in the edentulous area considered for implant placement. It represents the external architecture of the bone.
Evaluation of Available Bone
The available bone for implant placement is evaluated in terms of the following parameters (Fig 1):
I) Height
ii) Width
iii) Length
iv) Angulation
v) Crown height / Bone Height (Implant body) ratio
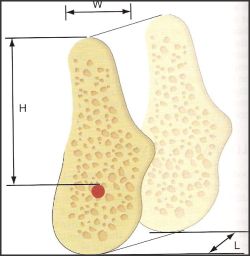 | Fig 1 : available bone at the implant site is evaluated in terms of height (H), width (W), and length (L)
 |
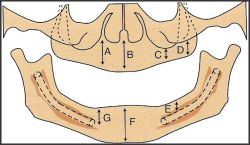 | Fig 2 : height of available bone is measured from the crest of the edentulous ridge to the opposing landmark
 |
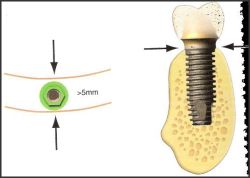 | Fig 3 : minimum bone width for a 4 -mm root-form implant is 5-mm in midfacial and lingual region
 |
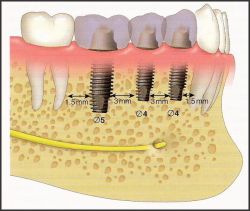 | Fig 4 the ideal mesiodistal length between an implant and tooth is 1.5 mm or more and 3 mm between each implant
 |
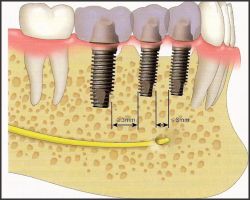 | Fig 5 the ideal mesiodistal length between an implant and tooth is 1.5 mm or more and 3 mm between each implant
 |
Available Bone Height
The available bone height in an edentulous site is an important consideration because it governs the selection of the height (or length) of the implant fixture. It also influences the available crown height space and, consequently, force considerations and esthetics.
The available bone height is measured from the crest of the edentulous ridge to the opposing limiting anatomical landmark during radiographic assessment (Fig 2). These limiting structures include the inferior alveolar canal in the mandible and the floor of the nasal cavity and maxillary sinus in the maxilla.
The anterior regions of the jaws have the greatest bone heights available. Specifically, the maxillary canine eminence region offers the greatest bone height in the maxilla and the mandibular first premolar region provides the most vertical column of bone in the mandible. [7]
In posterior regions, opposing landmarks such as the inferior alveolar canal and maxillary sinus prove to be more limiting for implant placement. This may necessitate use of narrower and shorter implants in these regions where greater forces are routinely generated. As a result, prognosis for implants placed in the posterior edentulous regions is regarded as being more guarded in comparison to anterior regions and the treatment plan may need to be modified to improve long term success.
A 2-mm of bone height between a critical structure (inferior alveolar canal or maxillary sinus) and the implant is considered as a guideline to guard against surgical error.
The height of implant also affects its total surface area. An implant 3mm longer provides more than 10% increase in surface area. The advantage of increased height does not express itself at the crestal bone interface but rather in initial stability of implant, the overall amount of bone implant interface, and a greater resistant to rotational torque during abutment screw tightening. The suggested minimum bone height for predictable long term endosteal implant survival is 9mm before 1981. The Branemark screw type implant body and osseointegrated approach was provided only in 3.75mm width and 9mm length and was used only in completely edentulous anterior maxilla and mandible. [8] This height requirement is reduced in the very dense bone of the symphysis of an atrophic mandible when the prosthesis is overdenture or increased in the very porous type of bone of the posterior maxilla. [9], [10].
Available Bone Width
Width of available bone is measured between the facial and lingual plates at the crest of potential implant site. The width of available bone represents the bucco-lingual dimension of available bone and determines the implant diameter.
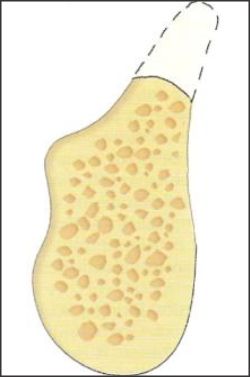
The crest of the edentulous ridge is composed of dense cortical bone which permits immediate fixation of the implant. It normally has a triangular cross-section and is supported by a wider base. Hence, an osteoplasty will provide greater width of bone, although of reduced height. However, the anterior maxilla does not follow this rule because most edentulous ridges exhibit a labial concavity in the incisor area with an hourglass configuration.
As a guideline, a minimum of 0.5-mm of bone should be available on each side of the implant at the crest to ensure sufficient bone thickness and blood supply around the implant. Hence, a 4-mm diameter implant usually requires more than 5-mm of crestal bone width (Fig 3).
Available Bone Length
This refers to the mesio-distal length of available bone in the edentulous area and is limited by adjacent teeth or implants. As a guideline, the ideal mesiodistal distance between an implant and a tooth is 1.5 mm or more and 3-mm between each implant. This is because if bone loss occurs at the crest module of an implant or from periodontal disease with the adjacent tooth, the vertical defect will not spread to a horizontal defect and cause bone loss on the adjacent structure (Figs 4 and 5). Thus, a 4-mm diameter implant usually requires a minimum 7 mm of available bone length.
Therefore in the narrower ridge with narrow diameter implant, placement of 2 or more implants often is indicated when possible to achieve sufficient implant bone surface area to compensate for the deficiency in width of implant.
Ideal implant diameter corresponds to the width of the natural teeth 2mm below the CEJ. So that implant crown emergence through the soft tissue is similar to a natural teeth.[11]
iv) Available Bone Angulation
Ideally, the bone is perpendicular to the plane of occlusion; is aligned with the forces of occlusion; and is parallel to the long axis of the tooth or restoration. The available bone angulation represents the root trajectory in relation to the occlusal plane and, therefore, signifies the direction of forces applied to the implant body. The maxillary central incisors are teeth in the arch which can be loaded at 12 degree angle only. [12]
The bone angulation does not remain constant after tooth loss. A common example is the anterior maxilla. Here, labial undercuts and resorption after tooth loss often mandate a greater angulation of the implant or correction of the site before insertion. A similar protocol may be considered in the submandibular fossa region of the posterior mandible which may show a deep lingual undercut [13], [14].
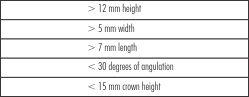 | Table 1: Division A Dimensions
 |
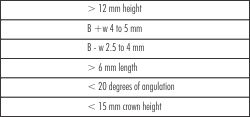 | Table 2: Division B Dimensions
 |
iv) Crown Height / Implant body ratio
The available bone height influences the available crown height space. The crown height influences the esthetic appearance of the final restoration. Importantly, crown height may be considered a vertical cantilever and influences the amount of moment force exerted on the implant and surrounding crestal bone.
As a guideline, the crown height/implant body ratio should be < 1 for improved implant prognosis. When this force multiplier is unfavorable (>1), the treatment plan may be modified to include a greater number of implants or wider implants to counteract the increase in stress.
Limiting factor of angulation of force between the body and the abutment of an implant is correlated with the width of bone. The angled load to implant body increases the crestal stresses.
Classification System for Available Bone
The dental implant approach to different bone volumes needs to be treatment plan oriented. In 1985, Misch and Judy proposed a classification system for the available bone with treatment options for each category. The basic four divisions have been expanded to following categories to extend this specific organized approach. Based on the Misch-Judy classification the bone volume divisions are:
Division A
Division B
i) Division B +
ii) Division B - w (width)
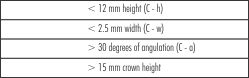
Division C
i) Division C - w (width)
ii) Division C - h (height)
iii) Division C - a (angulation)
Division D
Division A (Abundant Bone)
This category of bone volume is available soon after tooth loss and is abundant in all dimensions. Based on the available dimensions, use of Division A root-form implants with height > 12 mm and width > 4 mm is indicated in this category. Their advantages include:
Greatest surface area
Improved stress distribution
Greatest range of prosthetic options
Less fracture of implant and components
Less abutment screw loosening
Division A bone is mainly observed in the anterior regions
Less bone height is available in the posterior mandible and maxilla due to limiting structures. In such situations, wider implants (5 to 6 mm) may be considered in the molar regions as suitable alternatives.
Large diameter implants have less abutment screw loosening, and fracture of the implant body or components. [15], [16] Osteoplasty may be performed to obtain the necessary bone width.
Prosthetic Options Available in Div A bone
FP-1 restorations require Div A bone to allow ideal implant placement and natural appearance of the final prosthesis.
FP-2 or FP-3 prosthesis may be considered depending on amount of bone loss and lip positions.
RP-4 or RP-5 may need osteoplasty to gain sufficient interarch space to accommodate for the denture teeth, bulk of acrylic, superstructure and overdenture attachments.
Division B (Adequate Bone)
Slight to moderate atrophy is used to describe this clinical condition.[4] Division B bone is characterized by reduced bone width in comparison to Division A bone and is mostly observed in the posterior regions. Two subtypes (B + and B - w) exist depending on the extent of resorption. The available mesio-distal bone length and angulation criteria also differ as a consequence of the reduced width of bone. Criteria of available bone height and crown height remain the same.
 | Fig 6 : A Division B ridge may be converted to Division A by osteoplasty
 |
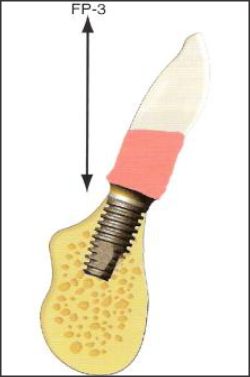 | Fig 7 : an FP- 3 prosthesis is usually indicated due to extended crown heights
 |
 | Fig 8 : Alternatively, augmentation may upgrade the Division B ridge to Division A
 |
 | Fig 9 A : preoperative radiograph showing division C-h bone in the maxillary premolar region with Division D in the molar region
 |
 | Fig 10 : The posterior maxilla has been modified to Division A bone by sinus grafting
 |
 | Table 3: Division C Dimensions
 |
Treatment Options for Div B bone
1) Osteoplasty
The most common approach followed is to modify the narrower Division B ridge into another bone division by osteoplasty.
If the bone height attained after osteoplasty is greater than 12 mm, the division has been altered to a Division A with width > 5 mm (Fig 6). A FP-2 or FP-3 restoration is indicated in this scenario to compensate for the increased clinical crown height (Fig 7). However, the crown height/implant body ratio remains < 1 after the osteoplasty due to sufficient available bone height. Osteoplasty to
 | Table 4: Division D Dimensions
 |
obtain a Division A ridge is mainly indicated in the anterior mandible because of the abundant available bone height and fewer esthetic concerns.
If bone height attained after osteoplasty is less than 12 mm, the division has been altered to a Division C - h with the crown height/implant body ratio > 1. The treatment options will then follow those available in the Division C - h bone.
2) Augmentation
The Division B ridge may be converted to a Division A by augmentation (Fig 8). The augmentation requires a 4 to 6 months healing period before placement of endosteal implants.
Augmentation is more predictable when the volume to augment is minimal and is for width rather than height due to the greater number of osseous walls in contact with the graft material. Augmentation is mainly indicated in the anterior maxilla for esthetics since it results in improved crown height/implant body ratios and more natural looking abutments.
3) Insert Division B implants
The third option is to treat the available bone volume as it is and place narrower diameter implants.
Division B implants have a smaller diameter of 2.7 to 3.5 mm. These root-form implants are indicated mainly for anterior single-tooth replacement for maxillary laterals or mandibular incisors. Their limitations are: [17], [18], [19]
The nearly 25% reduction in surface area results in almost twice the stress concentration at the crestal region.
Lateral loads result in almost thrice the stress to the implant as compared to Division A implants. Hence, a greater risk of fatigue fracture is present.
Due to the narrow diameter of the implant the emergence profile of the restoration is less esthetic (except for maxillary lateral or mandibular incisors)
Hence, when Division B implants are indicated, it is advisable to increase the surface area by placing additional implants (wherever possible) and by surface treatments. In addition, the angle of load must be reduced to less than 20 degrees to compensate for the smaller diameter.
Narrower diameter implants have been found to be successful in the anterior region of the maxilla and are preferable where space is limited
Division C (Compromised Bone)
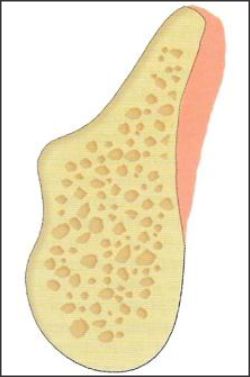
Moderate to advanced atrophy is used to describe this clinical condition. The bone may be deficient in one or more dimensions. (Fig 9)
With continued resorption, the Division C - w bone changes to a Division C - h bone which is commonly observed in the posterior regions because the maxillary sinus or mandibular canal limits the vertical height sooner. Division C - a bone is found most often in the anterior maxilla and mandible with facial undercut regions, or the mandibular second molar with a severe lingual undercut. Implant-supported prostheses are more complex for this category due to the reduced bone volume but the patient usually is in greater need for increased prosthodontic support.
Treatment Options for Division C Bone
A) Division C - w
1) Osteoplasty
This converts the Division C - w bone to a Div C - h category since the crown height/implant body ratio is > 1. The treatment protocol of Division C - h bone is then followed.
2) Augmentation
Augmentation of Division C - w bone is done when a fixed restoration is desired or when force factors necessitate so. The edentulism is then treated with the options available in the division of bone attained after augmentation. Augmentation is preferred in the posterior maxilla or mandible since osteoplasty may result in a Division D bone which represents the poorest prognosis. Bone grafting procedures are more difficult after height has been reduced. [20], [21], [22].
B) Division C - h
1) Augmentation
This is advocated in the posterior maxilla and mandible.
2) Root-form implants
Additional implants are required to increase the overall implant-bone surface area to counteract the unfavorable force multiplier of increases crown height. For the same reason, in edentulous patients, RP-5 prosthesis may be considered to reduce the cantilever.
Shorter textured implants may be suitable options in the posterior maxilla and mandible with compromised bone height as indicated by recent studies.
Alternative to endosteal implants in the posterior edentulous division c-h arch the other implant systems are placed which are as follow: [23], [24], [25].
3) Other implant systems
Subperiosteal
Disk design
Ramus frame
Transosteal
C) Division C - a
1) Augmentation to improve the angulation
2) Subperiosteal implants
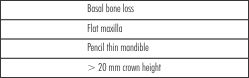
Division D (Deficient Bone)
Severe atrophy is used to describe the clinical condition.
The completely edentulous Division D patient is the most difficult to treat. The surgical skill required is greater and the prosthetic outcome has a guarded prognosis. Fixed restorations are almost always contraindicated due to significant crown height. Idiopathic fractures during surgery or from implant failure or removal are likely complications.
Treatment Options for Division D Bone
Augmentation
Autogenous bone grafts are indicated to upgrade the division. (Fig 10)
Endosteal or subperiosteal implants may be inserted depending on the division of bone attained.
Summary And Conclusion
The key determinant for clinical success of implants is available bone around that endosteal dental implant. The strength of bone is directly related to bone density. So available bone should be properly evaluated in terms of bone width, height, length, angulation during diagnosis to determine the prognosis of implant placement.
References
1. Adell R, Eriksson B, Lekholm U, Branemark PI, Jemt T (1990) Long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants 5:347-359.
2. Greeenfeld EJ (1913) Implantation of artificial crown and bridge abutments. Dent Cosmos 55:364-369.
3. Atwood DA (1963) Post extraction changes in the adult mandible are illustrated by microradiographs of midsagittal sections and serial cephalometrics roentgenogram. J Prosthet Dent 13:810-824.
4. Atwood DA (1971) Reduction of residual ridges: major oral disease entity. J Prosthet Dent 26:266-279.
5. Atwood DA, Coy WA (1971) Clinical, cephalometric, densitometric study of residual ridge. J Prosthet Dent 26:280-295.
6. Tallgreen A (1972) The continuing reduction of alveolar ridges in complete denture wearer: a mixed longitudinal study covering 25 years. J prosthet Dent 27:120-132.
7. Razavi R, Zena RB, Khan Z et al (1995) Anatomic site evaluation of edentulous maxilla for dental implant placement. J prosthet Dent 4:90-94.
8. Branemark PI (1983). Osseontegration and its experimental background. J Prothet Dent 50:399-410.
9. Misch CE (1999) short versus long implant concept: functional surface areas. Dent Today 18(8):60-65.
10. Misch CE (1990) Density of Bone: effect on treatment plan, surgical approach, healing and progressive bone loading. Int J Oral Implant 6:23-31.
11. Hebel KS, Gajjar R (1997) Achieving superior esthetics results: parameter for implants and abutment selection. Int J Dent Symposia 4(1):42-47.
12. Lam RW (1960) Contour changes in alveolar process following extraction. J prosthet Dent 10:25-32.
13. Pietrovski J, Sorin S, Hirshfield Z (1976) The residual ridge in partial edentulous patients. J prosthet Dent 36:150-157.
14. Pietrovski J,Massler M (1967) Alveolar ridge resorption following tooth extraction. J prosthet Dent17:21-27.
15. Rangert B, Krogh P, Langer P, et al (1995) Bending overload and implant fracture: a retrospective clinical analysis. Int J Oral Maxillofac Implants 10:326-334.
16. Misch CE, Bidez MW (1997) Occlusion and crestal bone resorption: etiology and treatment planning strategies for implants in Mc Niell C, editor: science and practice of occlusion, quitenssence.
17. Misch CE, Bidez MW (1995) Maxillary anterior single tooth Implant health esthetic comproise. Int J Dent Symp 3:4-9.
18. Lum LB (1991) A biomechanical rationale for the use of short implants. J Oral Implantol 17:126-131.
19. Misch CE, Bidez MW (1994) Implants protected occlusion, a biomechanical rationale. Compendium 15; 1330-1342.
20. Misch CM, Misch CE, Resnik RR, et al (1992) Reconstruction of maxillary defects with mandibular symphysis grafts for dental implants' preliminary procedural report. Int J Oral Maxillofac Implants 3:330-366.
21. Misch CM, Misch CE (1995) The repair of severe localized ridge defects for implant placement using mandibular bone grafts, implant dent 4:261-267.
22. Misch CM (1996) Ridge augmentation using mandibular ramus grafts for the placement of dental implants: presentation a technique. Pract Periodontics Aesthet Dent 8:127135.
23. Scortecci GM (1999) Immediate function of cortically anchored disk design implant without bone augmentation in moderately to severely resorbed completely edentulous maxillae. Oral implantol25:70-9.
24. Misch CE, Dietsh F (1992) The unilateral mandibular subperiosteal implant: indications and technique. Int J Oral Implantol 8(2, 3):21-29.
25. Misch CE (2005) Dental Implant Prosthetics.105-129.Elesvier Mosby . |