Introduction
Supernumerary tooth develops from an extra tooth bud arising from the hyperactivity of the dental lamina near the permanent tooth bud, or possibly from dichotomy or splitting of the permanent tooth bud itself.[1] Several pathologies may arise because of them like impaction, malposed teeth, midline diastemma, ectopic eruption, and formation of primordial or follicular cyst.[2] However, fusion of a normal permanent tooth and a supernumerary tooth is unusual.[3]
Fusion is the union of two developing dental germs resulting in a single large dental structure.[4] It is defined, according to the classification of Wedl and as supplemented by Busch, as the organic dentinal union of two or more individual teeth. De Jonge (1955) proposed the term 'Synodontia' to describe teeth, which originate by the inability of adjacent tooth germs to retain their individuality.[5] Fusion between supernumerary and permanent teeth occurs less frequently than fusion between other types of teeth.[6] The overall prevalence is estimated in the literature to be 0.5% in the deciduous and 0.1% in the permanent dentition.[7],[8],[9].
The aetiology of fusion is still unknown, although many theories have been proposed, including genetic factors, racial differences, local metabolic interference during tooth bud differentiation , traumatic or inflammatory causes.[6], [8], [9], [10]
The purpose of this paper was to report the case of a 12-year-old boy who presented with trauma-induced fusion of a supernumerary tooth and permanent maxillary right central incisor and describe its management.
Case Report
A 12-year old male patient reported to our institution with the chief complaint of extra tooth in the upper front region leading to an unaesthetic appearance. There was no associated history of pain or discomfort. Detailed anamnesis revealed a history of trauma in the upper front tooth region when the child was around 18 months of age, which led the milk tooth in the same region to get intruded. At that time, the patient visited a dental clinic and was recommended a 'wait and watch' approach, and one year
 | Figure1- Intra-oral photograph: mesiodens fused to labial surface of tooth 11
 |
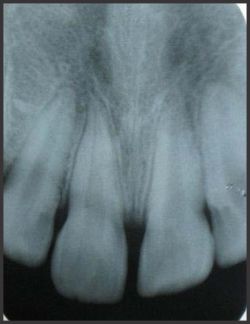
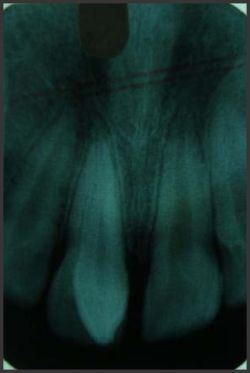 | Figure2- Pre-treatment radiograph: fused teeth with different roots and pulp cavities
 |
 | Figure3- Per-operative: reflected muco-periosteal flap revealing fusion extending to the root
 |
 | Figure4- Sectioning: of supernumerary tooth followed by odontoplasty
 |
 | Figure5- Post-operative photograph: depression on labial enamel of tooth 11
 |
 | Figure6- Esthetic rehabilitation: with composite resin
 |
 | Figure7- Post-operative radiograph: after 1 year, exhibiting normal periodontal and periapical tissues
 |
later the intruded tooth was extracted. There was no relevant past medical history or any hereditary conditions and his physical examination was unremarkable.
On intra-oral examination (Fig 1), an erupted conical-shaped extra tooth was seen labial to the permanent maxillary right central incisor [tooth no. 11] causing slight lingual tipping of the permanent tooth. A dental floss was passed through the crowns of the two closely placed teeth, but this failed indicating a fusion between the two with deep grooves on the complex. There was presence of midline diastema arousing a suspicion of another unerupted supernumerary in the same area.
Radiographic examination (Fig 2) revealed the presence of only one supernumerary tooth that was seen erupted. However, the fusion between the roots of the supernumerary and the permanent tooth was not evident radiographically. The root canal morphology was assessed using Clark's tube-shift technique that revealed two separate pulp chambers and canals.
Thus, a diagnosis of trauma-induced fusion between erupted conical mesiodens and permanent maxillary right central incisor was made that presented with two separate pulp cavities.
Treatment. Surgical sectioning and extraction of the supernumerary tooth were planned, and written consent was obtained after explaining the treatment plan to the patient and the parents.
Following local anesthesia, a full thickness muco-periosteal flap was raised (Fig 3). This revealed the extension of fusion beyond the cervix of the crown extending to the root. So, the buccal cortical plate was removed with a surgical handpiece under water coolant, followed by sectioning of the supernumerary tooth with a high-speed dental handpiece and diamond bur (104R, Shofu Inc., Kyoto, Japan) under a water coolant to separate the permanent central incisor and the supernumerary tooth (Fig 4). The teeth were separated such that the anatomy of the permanent tooth was not much disturbed. Also, the dentin of crown was not involved, leaving behind a layer of enamel, thus excluding the chances of sensitivity. Odontoplasty was performed on the root of permanent central incisor to establish a normal anatomy. There was no communication found between the pulps of the two involved teeth, confirming the radiographic diagnosis, thus, no endodontic treatment was required for the conserved central Incisor. It was expected that the involved permanent tooth would achieve reattachment of the cementum to bone as careful sectioning was done to avoid exposure of dentin, [which otherwise would have required restoration of the root to avoid dentin hyperesthesia]. Bonegraft (Ostofom, Zimmer Inc. Warsaw, IN, US) was placed and the mucosal flap was carefully repositioned and sutured using 4-0 interrupted silk suture. One week following the surgical removal, patient returned back to report no discomfort, mobility or sensitivity, and the tooth was vital (Fig 5). Sutures were removed and esthetic rehabilitation of permanent right central incisor was done with composite resin (Beautiful II, Shofu, Inc) (Fig 6). After one year of successful treatment, the permanent central incisor remains vital, no pathological feature has been observed, and the patient has experienced no discomfort. Postoperative radiograph exhibits normal periodontal and periapical tissues (Fig 7).
Discussion
Many theories have been proposed describing the aetiology of fusion, trauma to the predecessors being one of the causes; however, such cases are not well documented in the literature. Shafer, Hine, and Levy opined that the two normally separated tooth germs fuse when some physical force or pressure causes contact between them.[1] Lowell and Soloman believe that fused teeth result from some physical action that causes the young tooth germs to come into contact, producing necrosis of the intervening tissue, thus allowing the enamel organ and dental papilla to fuse together.[11] Spouge proposed that crowding of adjacent tooth germs may result in fusion.[12]
Thus, in the present case, the intrusive trauma to the predecessor incisor might have caused space lack in the area which was already crowded by the presence of a supernumerary tooth, thus, bringing a close contact between the two tooth buds, and hence, fusion ensued.
Fusion may be classified as partial or total, i.e., fusio-totalis, partialis-coronaries or partialis-radicularis.[8],[13] This process involves epithelial and mesenchymal germ layers resulting in irregular tooth morphology.[10] The pulp chambers and canals may occur either separately or together according to the formation stage at the moment of the union. If this union occurs precociously, the crowns will be together with separate roots resulting in a big dental structure. If the union happens after the crown formation, the roots will probably be together.[14] The two teeth may join at dentinal and/or enamel level - merging at enamel level alone being infrequent.[15]
However, unusually in the present case, both, the crowns as well as the roots were fused; but there was no communication between the pulp chambers and canals. Also, the union was limited to the level of enamel and cementum only with no involvement of dentin.
Most cases of fused teeth are asymptomatic, and do not require treatment; nevertheless, fusion might cause clinical problems related to function; loss of space in the dental arch; carious lesions in the grooves, particularly in the fusion zone; periodontal problems associated with the grooves that extend subgingivally; asymmetries when fusion occurs in the anterior segment; malocclusions, especially when supernumeraries are involved; causes deviations; sometimes delays the eruption of other teeth; and endodontic complications. In the anterior region, this anomaly also causes an unpleasant aesthetic tooth shape due to the irregular morphology. [6],[8],[9],[10]
Various treatment modalities have been described in the literature with respect to the different presentations, locations and morphological variations of fused teeth. These include endodontics, restorations, selective grinding, surgical separation or extraction followed by prosthesis, periodontal and/or orthodontic treatment.[9],[10] Most of these cases require surgical removal because of their abnormal morphology excessive mesiodistal width, causing crowding, tooth malalignment and occlusal dysfunction; however, many authors have reported salvaging the fused teeth by acquiring a multi-disciplinary approach.[8],[10],[16]
Ferreira-Junior et al [17], Cetinbas et al[18] and, Tsujino and Shintani[3] reported sectioning of the fused teeth and extraction of the supernumerary tooth. Ghoddusi et al[19], Nunes et al[10] and Song et al[20] assumed a non-surgical endodontic approach for treatment of fused teeth, while surgical endodontic approach has also been successfully adopted and documented.[15],[21] Tuna recommended extra-oral hemi-section and immediate replantation as an alternative treatment.[9] Good and Berson[22], and Rani et al[6] reported the management of fused teeth with combined multidisciplinary approach.
In the present case, treatment was recommended in order to improve the esthetic status of the patient, and to prevent periodontal disease and development of dental caries. The treatment required surgical separation and extraction of the supernumerary tooth followed by esthetic rehabilitation of the permanent tooth to achieve the desired result. Also, utmost care was taken to conserve the tooth structure and prevent exposure of dentin.
Conclusion
This case shows that presentation of fused teeth can be complex, thus requires diverse treatment protocols and necessitates proper diagnosis and multidisciplinary approach to achieve functional and esthetic success. Efforts must be directed to understand the tooth morphology and root canal anatomy in order to avoid treatment complications.
References
1. Shafer WG, Hine MK, Levy BM. A textbook of oral pathology. 4th ed., Philadelphia: W B Saunders Co., 2005:2-85.
2. Rajab LD, Hamdan MA. Supernumerary teeth: review of the literature and a survey of 152 cases. Int J Paediatr Dent 2002;12:244-254.
3. Tsujino K and Shintani S. Management of a supernumerary tooth fused to a permanent maxillary central incisor. Pediatr Dent 2010;32(3):785-8.
4. Regezi JA, Sciubba JJ, Jordan RCK. Oral pathology: clinical pathologic correlations. 4th ed., Philadelphia: W B Saunders Co., 2003:367-384.
5. Schulze C. Developmental anomalies of the teeth and the jaws. In Gorlin RJ, Goldman HM (eds). Thoma's Oral Pathology, 6th ed., St. Louis: CV Mosby Co., 1970:96-183.
6. Rani KA, Metgud S, Yakub SS, Pai U, Toshniwal NG, Bawaskar N. Endodontic and esthetic management of maxillary lateral incisor fused to a supernumerary tooth associated with a talon cusp by using spiral computed tomography as a diagnostic aid: a case report. J Endod 2010;36:345-349.
7. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and Maxillofacial Pathology. 2nd ed., New Delhi: Elsevier, 2005:49-106.
8. Hulsmann M, Bahr R, Grohmann U. Hemisection and vital treatment of a fused tooth: literature review and case report. Endod Dent Traumatol 1997;13:253-8.
9. Tuna EB, Yildirim M, Seymen F, Gencay K, Ozgen M. Fused teeth: a review of the treatment options. J Dent Child 2009;76(2):109-16.
10. Nunes E, de Moraes IG, Novaes PMO, de Sousa SMG. Bilateral fusion of mandibular second molars with supernumerary teeth: case report. Braz Dent J 2002;13(2):137-141.
11. Lowell RJ, Soloman AL. Fused teeth. J Am Dent Assoc 1964, 68(5): 762-763.
12. Spouge JD. Oral Pathology. St. Louis: CV Mosby Co., 1973:135-6.
13. Peyrano A, Zmener O. Endodontic management of mandibular lateral incisor fused with supernumerary tooth. Endod Dent Traumatol 1995,11(4):196-198.
14. Morris DO. Fusion of mandibular third and supernumerary fourth molars. Dent Update 1992;19(4):177-178.
15. Oliván-Rosas G, López-Jiménez J, Giménez-Prats MJ, Piqueras-Hernández M. Considerations and differences in the treatment of a fused tooth. Med Oral Patol Oral Cir Bucal 2004;9(3):224-8.
16. Delany GM, Goldblatt LI. Fused teeth: a multi- disciplinary approach to treatment. J Am Dent Assoc 1981;103(5):732-734.
17. Osny Ferreira-Junior, Luciana Dorigatti de Ávila, Marcelo Bonifácio da Silva Sampieri, Eduardo Dias-Ribeiro, Wei- liang Chen, Song Fan. Impacted lower third molar fused with a supernumerary tooth-diagnosis and treatment planning using cone-beam computed tomography. Int J Oral Sci 2009;1(4):224-228.
18. Cetinbas H, Halil S, Akcam MO, Sari S, Cetiner S. Hemisection of a fused tooth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod Oct 2007;104(4):120-4.
19. Ghoddusi J, Zarei M, Jafarzadeh H. Endododntic treatment of a supernumerary tooth fused to mandibular second molar: a case report. J Oral Sci 2006;48(1):39-41.
20. Song CK, Chang HS, Min KS. Endodontic management of supernumerary tooth fused with maxillary first molar by using cone-beam computed tomography. J Endod Nov 2010;36(11):1901-04.
21. Ozant O, Umit C, Fatih A. Comprehensive therapy of a fusion between a mandibular lateral incisor and supernumerary tooth: a case report. Int Dent J 2005;55(4):213-216.
22. Good DL, Berson RB. A supernumerary tooth fused to a maxillary permanent central incisor. Pediatr Dent 1980;2(4):294-6. |