Introduction
Wounds in the oral cavity feature extremely good healing capacities, however, some situations requires the isolation of wounds from the oral milieu, ranging from extractions to flap surgeries. Periodontal surgical procedures are routinely carried out for the management of diseased periodontal tissues. Several factors contribute to uneventful and healthy post-operative healing.[1],[2]
Wound healing following periodontal flap surgery is influenced by the factors like bacterial contamination, innate wound-healing potential, local site characteristics, surgical procedure / technique and systemic and environmental factors (e.g diabetes & smoking).
The inhibitory effect of bacterial contamination and infection on post-surgical wound healing has been well documented (Burke et al; Herrera et al). Following surgery, the healing process develops by an inflammatory response and in turn the inflammation promotes the rapid formation of biofilm. Periodontal wounds appear to heal faster in sites with fewer plaque score (Mengel et al). In fact the First European Workshop stated that post operative plaque control is the determining factor for the successful outcome of flap surgery.
As early as 1920, Ward advocated the use of periodontal dressing for routine periodontal surgical procedures in order to reduce pain, infection, root sensitivity & minimise caseous deposits within the wound site. But studies using split mouth design (Stahl et al, Greensmith & Wade, Jones et al) have demonstrated surgical sites with dressing resulted in more amount of plaque accumulation compared to sites without a dressing and concluded that dressing aids little to the healing process. Also, Addy et al found advantage in using 0.2%CHX rinse when compared to periodontal dressing.[3],[4],[5],[6],[7]
Three categories of some common periodontal dressings in the dental market are classified as solid and non-soluble, soft and non-soluble, and soft and soluble materials. The most common and widely used non-soluble dressing is the non-eugenol dressing in the Coe-pakTM (Coe laboratories, GC international Inc, UK) which is supplied as two pastes or as an auto-mixing system contained in a syringe.
GCF flow is an important determinant in the ecology of periodontal pocket or sulcus. It creates a flushing action and an isolation effect. In addition, it probably determines the growth level of subgingival microorganisms and is a potential marker for periodontal disease activity. GCF flow (or flow rate) is the process of fluid moving into and out of the gingival crevice or pocket. It is a small stream, usually only a few microliters per hour. It is approximately 10.2 μl/hr in health and in advanced periodontitis, it is as high as 137 μl/hr. 5-24 ml of GCF is secreted daily. The gingival flow however, is expected to increase dramatically as inflammation becomes more severe and vascular permeability increases. It has also been stated that increase in GCF flow is one of the first change occurring as inflammation progresses before any other visible signs of inflammation and that its value is more correlated to the status of the underlying gingival tissues than any other signs or indices of gingival inflammation.
Various studies have shown that GCF flow consistently increases following surgery till 2-3 weeks, decreasing to baseline or lower values following then in 6 weeks or so and that the percentage increase is directly proportional to the inflammatory component of the underlying healing tissues (Arnold et al 1966, Suppipat et al in 1978).
Griffiths and Sterne et al (1992) found thatwhile the initial volume of GCF showed no association with any clinical measurement, there was an association between flow rate of GCF and gingival colour. The volume of GCF collected in the final, 5th sample was associated with the Gingival Index. The sample site strongly influenced all measures of GCF volume. It is proposed that the flow rate of GCF may be a better indicator of gingival inflammation than the more imprecise clinical assessments of inflammation, since GCF flow rates more precisely reflect changes in tissue permeability.[8],[9],[10]
Greensmith Al et al in 1947 studied the differences between dressing (Coe-pak) and non- dressing wound after reverse bevel flap procedures. The results showed that both the groups had comparable clinical parameters and gingival fluid level. However, it was found that 45% of patients preferred no closure of the wound by periodontal dressing, while 37.5% had no preferences and 16.6% preferred a dressing.
Jones TM et al in 1979, compared clinical and histological results after access flap surgery with and without non-eugenol dressing and evaluated fluid Index, inflammatory index, pocket depth and patient comfort upto 16 weeks postoperatively. Results showed no difference in these parameters between quadrants where periodontal dressings were or were not used following surgery. The patients reported severe pain and discomfort postoperatively when the dressing was used. The results of this study suggest that a surgical dressing serves no useful purpose following a periodontal flap surgery.[6]
Its an accepted fact that there will be more amount of plaque and debris accumulation underneath a periodontal dressing as compared to sutures alone; however, whether it leads to delayed wound healing response is something which needs to be sorted out. (PHOTOS 1,2,3 AND 4).
Thus the aim of this study was:
1. To assess the early wound healing outcomes of patients with a periodontal dressing and to compare with a non-dressed site.
2. To assess patient comfort as evaluated by the patient assessment questionnaire.
Materials and methods:
This was a randomized case controlled clinical trial with split mouth design study which was conducted on patients reporting to the Department of Periodontics, The Oxford Dental College and Hospital, Bangalore. Patients who were systemically healthy, non-smokers, not under any medication, diagnosed with periodontitis, indicated for periodontal flap surgery were included in the study. It was made clear that participation is entirely voluntary. Patients were explained about the nature of the study, the need for surgery and the outcome of it, followed by which a verbal & written consent was obtained. A total number of 15 patients having at least 2 sextants indicated for surgery were randomly allotted to either Dressing group (Coe-PakTM) or Non-dressing group and a split mouth design was followed. Access flap surgery was done and patients were given dressing or left without it following the surgery.
Comprehensive medical and dental history was recorded and routine blood investigations were carried out. The patients were then given an explanation of the study and an informed consent was obtained and was also asked to fill a self reported questionnaire.
On the day of surgery (baseline) PeriotronTM score was recorded at the deepest site of the selected area for surgery. All periodontal surgical procedures were performed on an outpatient basis under aseptic conditions using the conventional techniques of Kirkland's access flap surgery.
All subjects answered a questionnaire [Pain (0-10);Swelling of mucosa (0-3);Swelling of face (0-3);Bleeding post operatively (yes or no);Mean no of analgesics taken] at each day following surgery till one week, which was provided to them as a VAS chart, to evaluate post-operative symptoms.
 | Photo: 1 - Coe- Pak Placement At Baseline
 |
 | Photo: 2 - Deposits Underneath The Coe- Pak After One Week
 |
 | Photo: 3 - Non-Dressing Site At Baseline
 |
 | Photo: 4 - Plaque Deposits On The Suture Threads After One Week
 |
All the patients were subjected to evaluation of swelling of soft tissues and colour of gingiva at one week after surgery.
Volumetric measurement of GCF was done at baseline (at the day of surgery) and two weeks following surgery by using filter paper strips which was subjected to quantitative analysis on the Periotron 8000TM.
Statistical analysis was done by unpaired and paired Student t test. Significance is assessed at 5 % level of significance. The Statistical software namely SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1, Systat 12.0 and R environment ver.2.11.1 were used for the analysis of the data.
Results:
Graph 1, Graph 2, Graph 3, Graph 4, Graph 5, Graph 6
Discussion
Periodontal dressings are routinely used following periodontal surgical procedures. This study compared clinically the use of dressing following periodontal flap surgery versus non-dressing, in a randomized clinical trial;considering the hypothesis that it results in more plaque accumulation and hence pronounced inflammation immediate post-surgically; which delay the healing of the tissues. Also the bulky periodontal dressing can result in considerable patient discomfort. The results of the present clinical experiment has demonstrated thatthe useof dressings resulted in increased inflammation immediate post-surgically based on the clinical parameters and increased patient discomfort based on the self reported questionnaire by the patient.
Smeekens JP et al 1992, studied the histological evaluation of tissue response 7 days after surgery using dressing materials like Barricaid, Ward's wonder pak and carboxyl methyl cellulose and control. No significant differences between the 2 different dressings. The control areas showed an overall lesser degree of inflammation. After 14 days, no difference
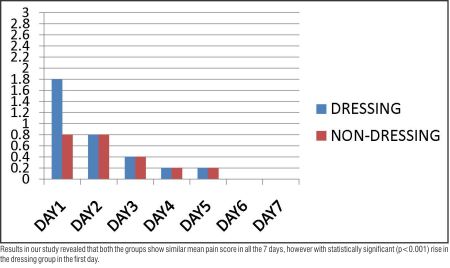 | GRAPH 1: PAIN- Post operative pain experience (0= no pain, 1= mild pain, 2= moderate pain, 3= severe pain) noticed at each day following surgery till one week.
 |
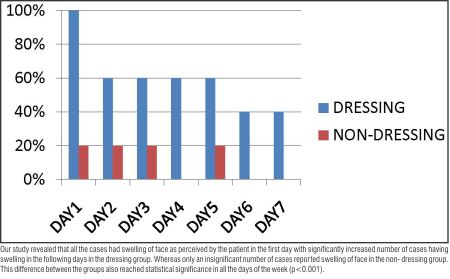 | GRAPH 2: SWELLING OF FACE- Post- operative swelling of face (YES/ NO) noticed at each day following surgery till one week.
 |
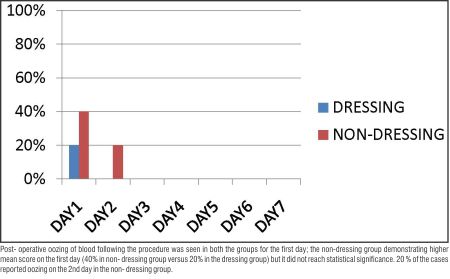 | GRAPH 3: BLEEDING POST-OPERATIVELY- Post- operative oozing of blood (YES/ NO) noticed at each day following surgery till one week.
 |
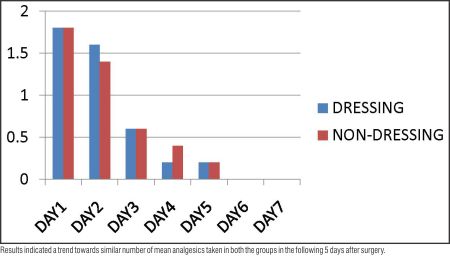 | GRAPH 4: MEAN NUMBER OF ANALGESICS TAKEN- Number of analgesics taken every day following surgery till one week is noted in the two groups.
 |
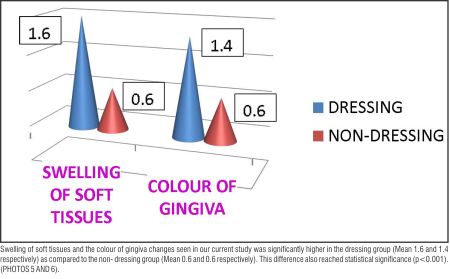 | GRAPH 5: CLINICAL EVALUATION AT ONE WEEK- Swelling of soft tissues and colour of gingiva was evaluated after one week as absent (0), moderate(1) or pronounced(2) in the two groups.
 |
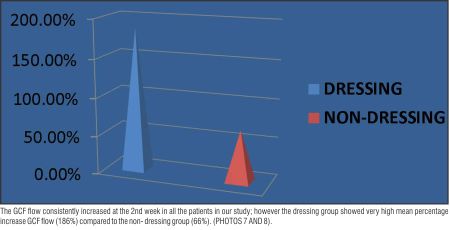 | GRAPH 6: GCF FLOW- Measured at baseline (at the day of surgery) and 2 weeks and the percentage rise in GCF flow is noted in the two groups.
 |
between test and control were noted.
Allen DR et al in 1983, Studied the clinical effects of a periodontal dressing after Modified Widman flap surgery. The patients were studied for 2 months after surgery (at 2 weeks, 1 month, and 2 months) with respect to gingival crevicular fluid, gingival inflammation, attachment level and pocket depth. The patients were also given a questionnaire. Result showed no significant differences between the dressed and undressed sites.[5],[11],[12]
Jones TM, Cassingham RM in 1979 compared healing following periodontal surgery with and without dressing in humans.Clinical and histological results after periodontal flap surgery with and without dressing were evaluated and subjectively postoperative comfort was evaluated. Out of the 20 quadrants
 | Photo: 5 - Clinical Picture Of Gingiva After One Week Under Coe- Pak
 |
 | Photo: 6 - Clinical Picture Of Gingiva After One Week Without Dressing
 |
 | Photo: 7 - Paper Strip Placement For Gcf Evaluation
 |
 | Photo: 8 - Periotron Score
 |
operated half received a noneugenol dressing and the other half had no dressing. GCF, gingival index, pocket depths and patient comfort were studied up to 16 weeks. Results indicated that there was no difference in clinical parameters. Patients reported more pain and discomfort when dressing was used.
Checchi L, Trombelli L in 1993 evaluated postoperative pain and discomfort with and without periodontal dressing in conjunction with 0.2% chlorhexidine mouthwash after apically positioned flap procedure. 24 patients requiring bilateral comparable procedures was taken up in a split mouth design. Results indicated a similar trend for mean pain scores as assessed by patients for both sides during the 7-day postoperative period. No significant differences were found between the 2 treatments with respect to frequency distribution of patients who did or did not take analgesics. Although patients with dressing frequently experienced eating difficulty, most stated a psychological feeling of protection and well-being with its use.
However, in our study results indicated a higher trend for mean pain scores and swelling of face as assessed by patients in the dressing group compared to the non- dressing group during the 7-day postoperative period. This can be attributed to the hardness on setting, non-adhesiveness and non-solubility of the Coe- PakTM dressing and comparative bulkiness of the dressing as compared to when it is left undressed, although it mainly depends on the nature and duration of surgical procedure.
Mild post-procedural oozing of blood was found to be more in patients without a dressing as compared to the Coe-Pak group. This mainly implies that a periodontal dressing is more helpful in controlling post-operative oozing of blood following flap surgery, if any; and should be advocated in cases where hemostasis could not be achieved properly.
Clinical evaluation after one week revealed more pronounced swelling and colour changes of the gingiva in patients with a Coe- Pak dressing. These differences could be attributed due to the higher amount of plaque accumulation and hence higher inflammation seen underneath Coe- Pak as compared to the non-dressing sites.
Also, the mean percentage increase of GCF flow from baseline to 2 weeks was found to be higher with the same. GCF is a reflection of the inflammatory status at the base of the gingival sulcus, thus this difference reflects that Coe- pak resulted in pronounced inflammation at the base of the sulcus whereas it was minimal when no dressing was placed.
Patients with dressing frequently experienced eating difficulty and most of them preferred the usage of no dressings (60%), although most (20%) stated a psychological feeling of protection and well-being with its use and the rest had no preference (20%).
Conclusion
At this time, there is a great deal of debate over the value and usefulness of periodontal dressings. Experimental evidence has not fully resolved this issue.
Based on the results of our study, we can conclude that periodontal dressing with Coe- PakTM results in more inflammation immediate post-surgically which may in turn delay the wound healing response as compared to patients without a dressing following periodontal flap surgery, permitting the cellular oxidation and exchange of tissue fluids which are essential for the events in wound healing process.
Thus a periodontal dressing should only be advocated in certain cases where it is definitely indicated e.g., apically displaced flap to prevent its displacement coronally (Tyrell et al), or to provide support to stabilize a free gingival graft (Farnoush et al). It is indicated in other cases where good adaptation of the flap is not achievable (Allen et al). In most other cases, it should be left on the preference of the operator and the patients.
So, instead of regular use of a dressing following flap surgeries, we can limit our use only to certain indications and in patients who prefer the feeling of being well protected psychologically.
Acknowledgements:
1. I would like to thank Dr. A. V. Ramesh, The Head of The Department of Periodontics,The Oxford Dental College, Hospital and Research Center;
2. I would also like to extend my support to Mr. K.P. Suresh, for helping me in carrying out the statistical analysis; and
3. And last but not the least, I would like to thank the Management, The Oxford Dental College, Hospital and Research Center,for providing me with the materials for carrying out the study.
References
1. Burke, J. F. (1971) Effects of inflammation on wound repair. J Dent Res 50, 296-301.
2. Flores de Jacoby, L. & Mengel, R. (1995) Conventional surgical procedures. Periodontol 2000 9, 38-54.
3. Sandalli. P. & Wade, A. B. (1969) Alterations in crevicular fluid flow during healing following gingivcctomy and flap procedures. J Periodontol Res 4, 314-318.
4. Stahl. S. S.. Witkin. G. Heller A. & Brown. R. (1969) Gingival Healing III. The effects of periodontal dressings on gingivectomy repair .J Periodontol 40, 34- 37.
5. Allen, D. R. and Caffesse, R. G. (1983): Comparison of results following modified Widman flap surgery with and without surgical dressing. J. Periodontol. 54, 470-475.
6. Jones, T. M. and Cassingham, R. J. (1979): Comparison of healing following periodontal surgery with and without dressing in humans. J. Periodontol. 50, 387-393.
7. Checchi L, Trombelli L. Postoperative pain and discomfort with and without periodontal dressing in conjunction with 0.2% chlorhexidine mouthwash after apically positioned flap procedure. J Periodontol. 1993;64(12):1238-42.
8. Arnold R, Lunstad G, Bissada N. Alteration in crevicular fluid flowduring healing following gingival surgery. J Periodont Res1966; 1: 303-308.
9. Griffiths GS, Sterne JAC. Association between volume and flow rate of GCF and clinical measurements of gingival inflammation in a population of British male adolescents. J Clin Periodontol 1992; 19: 464- 470.
10. Cheshire, P. D., Griffiths, G. S., Griffiths, B. M. and Newman, H. N. (1996): Evaluation of the healing response following placement of Coe-pak and an experimental pack after periodontal flap surgery. J. Clin. Periodontol. 23, 188-193.
11. Eber, R. M., Shuler, C. F., Buchanan, W., Beck, F. M. and Horton, J. E. (1989): Effects of periodontal dressings on human gingival fibroblasts in vitro. J. Periodontol. 60, 429-434.
12. Smeekens JP, Maltha JC, Renggli HH. Histological evaluation of surgically treated oral tissues after application of a photocuring periodontal dressing material. An animal study. J Clin Periodontol. 1992;19 (9 Pt 1):641-5. |