Introduction
Special needs individuals are children or adults who are prevented by a physical or mental condition from full participation in the normal range of activities of their age groups[1],[2]. The designation is useful for getting needed services, setting appropriate goals and gaining understanding for a child and stressed family[3]. They usually exhibit high orthodontic treatment needs because of an increased prevalence and severity of malocclusions[4],[5],[6]. Although their parents are highly motivated to improve the children's quality of life, by improving the appearance and the oral function, they are also the least likely to receive orthodontic treatment[2]. Careful attention to malocclusion in children with special needs leads to a considerable improvement in the quality of life[7].
The Dental Aesthetic Index (DAI), developed in the United States of America[8]predicts the clinical judgments of orthodontists in separating handicapping from non-handicapping malocclusion[9]. DAI is integrated into the International Collaboration Study of Oral Health Outcomes by the World Health Organization as an international index, links clinical and aesthetic components mathematically to produce a single score[10]. As dental auxiliaries can use the DAI to determine which patients to refer to a specialist, this can reduce the number of initial consultations by dentists or orthodontists, an important advantage in public health programmes[11],[12]. DAI scores have also been found to be significantly associated with the perception of treatment need by students and parents (Cons et al. , 1987; Spencer et al. , 1992), and these are good predictors of the acceptance of future fixed orthodontic therapy (Jenny and Cons, 1996b)[12].
The DAI has proven to be reliable and valid index[13],[14]. It is generally agreed that DAI is quick, relatively simple to use and universally acceptable[15]. Besides, the DAI has been adopted by the World Health Organization (WHO) as a cross-cultural index and has been applied among diverse ethnic groups without modification. All these reasons made it a suitable epidemiological index for using in developing countries, which lack a specifically developed orthodontic treatment need index[16]. The DAI satisfies this need and can be used in epidemiological surveys to assess unmet treatment need[15],[17].
The purpose of this study was to evaluate the various malocclusions and understand the orthodontic treatment need among 12-15 years children with special needs from special schools using Dental Aesthetic Index, so that better treatment services can be planned in future in the field of dentistry to treat the malocclusions.
Materials and Methods
A cross-sectional prospective study was performed among 78 children with special needs (52 boys and 26 girls) from special schools in Chandigarh and its surrounding areas aged between 12 to 15 years. These children were suffering from various developmental, physical and mental disabilities [Table 1]. This age group was chosen as this is the age when the malocclusion is expressed fully and the need for orthodontic treatment can be estimated so that the early intervention is possible.
Students were excluded from the study if they wore an orthodontic appliance or reported a history of previous orthodontic treatment, who were not cooperative for oral examination, children below the age of 12 years and children above the age of 15 years. The study was approved by the Ethical Committee and prior consent to conduct the study was obtained from the respective school authorities and from the parents or guardians of the children.
The dental examinations and diagnostic criteria followed the World Health Organization recommendations for oral health surveys[18]. Clinical examinations for evaluating DAI were made by two calibrated examiners. Thorough methodology training for DAI measurements was done prior to the data collection at the Department of Orthodontics and Dentofacial Orthopedics, M. M. College of Dental Sciences and Research, Mullana, Haryana. Twenty five of the children were re-examined 1 month after their initial examination to check the reliability of two examiners. The reliability of two examiners was calculated by Cronbach's Alpha.
The students were examined in natural daylight in one of the brightest rooms of their school using the Community Periodontal Index (CPI) probe, metal millimeter ruler and mouth mirror. Clinical examinations for evaluating DAI were made and the data was collected in WHO Oral Health Assessment Form (1997). Scores for each component were then multiplied by its corresponding regression coefficient using the rounded weights. The products were added, and summed up with the regression constant to give the DAI score [Table 2].
The result was then grouped according to various malocclusion severity levels:
1. < 26: little or no treatment need
2. 26 to 30: treatment elective
3. 31to 35: treatment highly desirable
4. > 35: treatment mandatory
The statistical analysis was carried out using Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, version 15.0 for Windows). Qualitative or categorical variables were described as frequencies and proportions. Proportions were compared using Chi square or Fisher's exact test whichever was applicable. All statistical tests were two-sided and performed at a significance level of α=0.05.
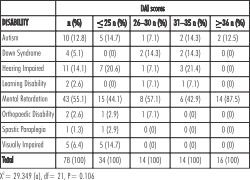 | Table 1. Disability wise distribution of DAI scores.
 |
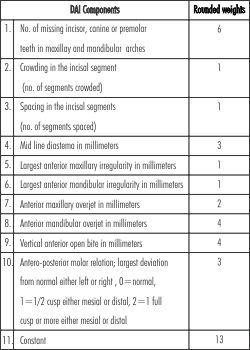 | Table 2. Standard Dental Aesthetic Index (DAI) scoring
 |
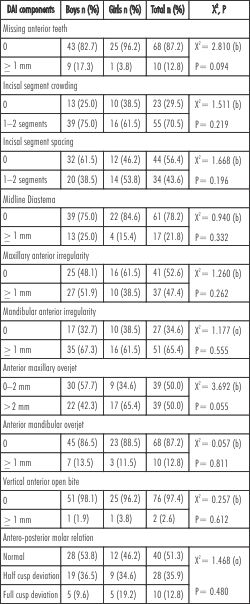
 | Table 4. Distribution of DAI components.
 |
 | Table 3. Age wise distribution of DAI scores and orthodontic treatment needs.
 |
 | Table 5. Prevalence of malocclusion and orthodontic treatment needs of study population.
 |
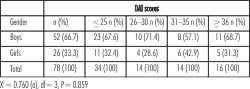 | Table 6. Gender wise distribution of DAI scores.
 |
Results
The reliability between two examiners was 0.903 which is more than 0.7 it indicated that values of two observers were reliable and the correlation coefficient between examiner 1 and examiner 2 was 0.824 which is excellent correlation.
Among the total 78 children with special needs, 52 (66.7%) were boys and 26 (33.3%) were girls. From these 10 (12.8%) of the children were suffering from autism, 4 (5.1%) were suffering from Down Syndrome, 11 (14.1%) were hearing impaired, 2 (2.6%) were suffering from learning disability, 43 (55.1%) were suffering from mental retardation, 2 (2.6%) were suffering from orthopaedic disability, 1 (1.3%) were suffering from spastic paraplegia and 5 (6.4%) were visually impaired. The DAI scores calculated for all the disabled children are shown in Table 1. No statistically significant differences were observed with in the study group for different disabilities (X2=29.349, p=0.106). Among the 78 children, 21 (26.9%) belonged to 12 years of age group, 17 (21.8%) belonged to 13 years of age group, 19 (24.4%) belonged to 14 years of age group and 21 (26.9%) belonged to 15 years of age group. No statistically significant differences were observed with in the study group for different age groups (X2=7.495, p=0.586). [Table 3]
Out of the 78 examined school children, 68 (87.2%) had no missing anterior teeth while 10 (12.8%) had 1 or more missing anterior teeth. Among the 52 examined boys, 43 (82.7%) had no missing anterior teeth, and 9 (17.3%) had 1 or more missing anterior teeth. Among the 26 examined girls, 25 (96.2%) had no missing anterior teeth, and 1 (3.8%) had 1 or more missing anterior teeth. A total of 23 (29.5%) school children had no incisal segment crowding and 55 (70.5%) had 1- or 2-segments crowding. A total of 44 (56.4%) school children had no incisal segment spacing and 34 (43.6%) had 1- or 2-segments spacing. Of 78 school children examined, 61 (78.2%) had no midline diastema and 17 (21.8%) had diastema of 1-4 mm. [Table 4]
41 (52.6%) of the children had no maxillary anterior teeth irregularity and 37 (47.4%) had more than 1 mm maxillary anterior irregularity. A total of 27 (34.6%) of the children had no mandibular anterior teeth irregularity and 51 (65.4%) had more than 1 mm mandibular anterior irregularity. [Table 4]
In the present study, 39 (50.0%) school children had an anterior maxillary overjet of 0 to 2 mm, and 39 (50.0%) had an overjet of >2 mm. Of the boys, 30 (57.7%) had an anterior maxillary overjet of 0 to 2 mm, and 22 (42.3%) had an overjet of >2mm. 9 (34.6%) of the girls had an anterior maxillary overjet of 0 to 2 mm and 17 (65.4%) had an overjet of >2mm. Of the 78 examined school children, 68 (87.2%) had no mandibular overjet and 10 (12.8%) had a mandibular overjet of 1-5 mm. Of the 78 examined school children, 76 (97.4%) had no anterior open bite and 2 (2.6%) had an anterior open bite of 1-2 mm. Of the 78 examined school children, 40 (51.3%) had normal molar relationship, 28 (35.9%) had half-cusp deviation, and 10 (12.8%) had full-cusp deviation. However, for all 10 components of DAI, there were no statistically significant differences observed between boys and girls. [Table 4]
In the present study, the distribution of DAI scores and orthodontic treatment needs showed, 34 (43.6%) had DAI scores <_ 25 with no abnormality or little malocclusion requiring no or slight treatment, 14 (17.9%) had DAI scores of 26-30 with definite malocclusion requiring elective orthodontic treatment, 14 (17.9%) had DAI scores of 31-35 with severe type of malocclusion requiring highly desirable orthodontic treatment, 16 (20.5%) had DAI scores >_36 with very severe or handicapping malocclusion requiring mandatory type of orthodontic treatment. [Table 5]
Among the students who were having DAI scores <_ 25, 23 (67.6%) were boys and 11 (32.4%) were girls. Students having DAI scores of 26-30, comprised 10 (71.4%) boys and 4 (28.6%) girls. Students having DAI scores of 31-35, comprised 8 (57.1%) boys and 6 (42.9%) girls. Students having DAI scores >_ 36 comprised 11 (68.7%) boys and 5 (31.3%) girls. No statistically significant differences were found with in the study group between the boys and girls. (X2=0.760, p=0.859). [Table 6]
Discussion
The results of this study indicated that 43.6% of the disabled children had a dental appearance that required no orthodontic treatment. This is comparable to the study of Onyeaso CO for mentally handicapped children in Ibadan, Nigeria which reported about 42% not requiring treatment[19].This result is, however, lower than that reported by Shivakumar and Chandu in a study of same age group of normal Indian children[20]. In this latter study, over 79.9% of the normal children had DAI scores of 25 or less with slight or no treatment need. Furthermore, the results of our study indicated that the children with special needs had a higher DAI score of >_36 than the normal Indian children. It came out to be 20.5% in our study, which is very high in comparison to 0.5% as reported by Shivakumar and Chandu[20]. It shows that children with special needs had a high frequency of very severe or handicapping malocclusion indicating mandatory treatment need as compared to normal children.
A large proportion of the children had severe to very severe malocclusion with treatment considered mandatory based on the decision points on the DAI scale. Unfortunately, the orthodontic treatment need of these children may not be met due to environmental factors and individual characteristics. Those with disabilities often lack the ability to recognize health problems and when they do recognize the need for services, many environmental and individual barriers prevent them from receiving necessary care. Constraints in a developing country like India are such that access to dental services including orthodontic care is impeded by several factors. These include the relatively low dental awareness, low number of orthodontic specialists, high cost of treatment, socio economic status of the patients and the lean budgetary allocation to oral health care.
Concerning the different malocclusion traits, hypodontia was found to occur in 12.8% of the study population which is comparable to that (7%) previously reported by Onyeaso CO among the handicapped children[21]. Spacing occurred quite frequently among the disabled children. The higher prevalence of spacing in the disabled was a reflection of the higher frequency of missing teeth noted in such subjects, which our present study confirms.
About one-half of the study population noted with increased overjet is very high when compared to 6.7% observed in the normal population by Shivakumar and Chandu[20]. This is of orthodontic concern, as in a previous report by Franklin and Luther children with cerebral palsy have a significantly increased overjet when compared with normal children[22]. Children with mental retardation formed a large proportion of the study population. This may, therefore, explain the higher percentage of malocclusion in this study population when compared with the normal population. Anterior open bite was observed in 2.6% of the study population which was very less than that 25.5% noted by Utomi and Onyeaso in the mentally handicapped children[15]. It is, however, comparable to that 2.4% reported by Shivakumar and Chandu in normal subjects[20]. Oral dysfunctions and parafunctions of the masticatory system has been suggested as being responsible for the increased prevalence of malocclusion in mentally handicapped children by Oreland and Heijbel[23].
48.7% of the population had molar relationship discrepancies which is higher than that reported in the normal population 9.9% by Shivakumar and Chandu[20].
Utomi and Onyeaso found 36.2% of mentally handicapped children having severe and very severe malocclusion indicating treatment highly desirable and mandatory using DAI[15]. In our study, 46.51% of children with mental retardation fall in this category which is slightly higher than their study. This means mentally handicapped children are really suffered from malocclusions requiring very much need for orthodontic treatment. Luppanapornlarp and Leelataweewud found 37.5% of autistic children having severe and very severe malocclusion indicating treatment highly desirable and mandatory using DAI[14]. In our study, 40% of children with autism came out for this category which is nearly similar to their study.
Although, DAI is a relatively simple, reproducible, valid and appears to be the easiest tool to use, but it does not take into account buccal crossbite, posterior open bite, central line discrepancies, or a deep overbite, factors which may have considerable impact on treatment complexity and, therefore, weaken the index.
Conclusion
1. A large proportion of the children with specials needs had very severe malocclusion where treatment is considered mandatory.
2. The children with special needs had higher frequencies of all the malocclusion traits than normal children. Hence children with special needs have more orthodontic treatment needs than the treatment needs for normal children.
3. The mentally disabled children had higher frequencies of all the malocclusion traits than sensory impaired children. Hence mentally disabled children have more orthodontic treatment needs than the treatment needs for sensory impaired children.
4. Malocclusion is not a single entity but rather a collection of situations, each in itself constituting a problem, and any of these situations can be complicated by a multitude of genetic and environmental causes, so further studies in future can help in exploring more.
5. Establish a good doctor-patient relationship, to gain the child's and parents' trust and to improve their confidence.
References
1. Becker A, Shapira J,Chaushu S: Orthodontic treatment for disabled children-A survey of patient and appliance management.Jour of Orthodontics/vol.28/2001/39-44.
2. Becker A, Chaushu S, Shapira J: Orthodontic treatment for the special needs child. Seminars in orthodontics Dec 2004; vol. 10(4): 281-292.
3. Soni S, Aggarwal P, Dua V: The Use of Index of Orthodontic Treatment Need (IOTN) in Children with Special Needs. Int J Cont Dentistry.June 2011;2(3):72-79.
4. Shah N, Mathur V, Logani A: Guidelines for Oral Health Promotion & Intervention for Disabled Population. Developed under GOI - WHO Collaborative Program (Biennium 08-09).
5. Koidin MB: Orthodontic care for the person with special needs: an overview. Exceptional Parent. May 2002: 1-2.
6. Winter K, Baccaglini L, Tomar S: A review of malocclusion among individuals with mental and physical disabilities. Special Care in Dent. 2008; 28(1):19-26
7. Oliveira A, Paiva S: Prevalence and determinant factors of malocclusion in children with special needs.Ejo. oxfordjournals.org/ content/ early/ 2010/ 10/18/ejo.cjq094.abstract.
8. Huwaizi A, Rasheed T: Assessment of orthodontic treatment needs of Iraqi Kurdish teenagers using the Dental Aesthetic Index. Eastern Mediterranean Health Journal. 2009; vol 15(6): 1535-41.
9. Jenny J, Cons NC:Predicting handicapping malocclusion using the Dental Aesthetic Index (DAI). Int Dent J. 1993 Apr;43(2):128-32.
10. Danaei S, Amirrad F: Orthodontic treatment needs of 12-15-year-old students in Shiraz, Islamic Republic of Iran. Le Rev de S de la Medi or.2007; vol 13 (2): 326-334.
11. Cons NC, Jenny J: Comparing ethnic group-specific DAI equations with the standard DAI.Int Dent J. 1994 Apr;44(2):153-8.
12. Hamamci N, Basaran G: Dental Aesthetic Index scores and perception of personal dental appearance among Turkish University students. Eur J Ortho. 31(2009): 168-173.
13. Joanna J, Naham C: Comparing and contrasting two orthodontic indices, the Index of Orthodontic Treatment Need and the Dental Aesthetic Index. Am J Orthod Dentofac Orthop.1996;110:410-6.
14. Luppanapornlarp S, Leelataweewud P: Periodontal Status and Orthodontic Treatment Need of Autistic children. World Journal of Orthodontics. 2010; vol.11, no.3: 256-261.
15. Utomi IL, Onyeaso CO: Malocclusion and orthodontic treatment need of mentally handicapped children in Lagos, Nigeria: Pesq Bras Odontoped Clin Integr, João Pessoa. 2009; 9(1):7-11.
16. Naham C, Joanna J: Utility of the Dental Aesthetic Index in Industrialized and Developing Countries. Journal of Public Health Dentistry.June 1989; Volume 49, Issue 3, pages 163-166.
17. Jenny J, Cons NC: Establishing malocclusion severity levels on the Dental Aesthetic Index (DAI) scale. Aust Dent J. 1996 Feb;41(1):43-6.
18. World Health Organization: Oral Health Surveys-Basic Methods 4th edition. Geneva 1997; ISBN: 9241544937.
19. ONYEASO CO: Orthodontic treatment need of mentally handicapped children in Ibadan, Nigeria, according to the dental aesthetic index. Journal of dentistry for children. 2003; vol. 70(2), pp. 159-163.
20. Shivakumar KM, Chandu GN: Severity of malocclusion and orthodontic treatment needs among 12-to-15-year-old school children of Davangere District, Karnataka, India. Eur J Dent. 2010; vol 4: 298-307.
21. Onyeaso CO: Malocclusion pattern among the handicapped children in Ibadan, Nigeria. Nig J Clin Pract. 2002; 5(1): 52-60.
22. Franklin DL, Luther F: The prevalence of malocclusion in children with Cerebral palsy. Eur J Ortho. 1996; vol 18: 637-643.
23. Oreland A, Heijbel J: Oral function in the physically handicapped with or without severe mental retardation. ASDC J Dent Child. 1989 Jan-Feb; 56(1): 17-25.