Introduction
Since 1964, when Simring and Goldberg[1] first described the relationship between periodontal and endodontic disease, the term 'endo-perio' has become an integral part of the dental vocabulary. The relationship between pulpal and periodontal disease can be traced to embryological development since the pulp and the periodontium are derived from a common mesodermal source of the developing tooth bud. Ectomesenchymal cells proliferate to form the dental papilla and follicle, which are the precursors of the periodontium and the pulp respectively. This embryonic development gives rise to anatomical connections, some of which remain patent throughout life.
Pathways of Communication
There is a very close relation between pulpal and periodontal tissues and the disease transmission between these two is strongly supported by many studies, which showed significant microbiological similarities between infected root canals and advanced periodontitis.[2],[3] Other than these microbial findings, similarities in the composition of cellular infiltrates also suggest the existence of communication between the pulp and the periodontal tissues.[4] The possible pathways for ingress of bacteria and their products into these tissues can broadly be divided into: anatomical and nonphysiological pathways.[5]
Anatomical pathways
These include vascular pathways such as the apical foramen and the lateral canals and tubular pathways.
Apical Foramen: The apical foramen is the principal and most direct route of communication between the periodontium and the pulp. Although periodontal disease has been shown to have a cumulative damaging effect on the pulp tissue, total disintegration of the pulp is only a certainty if bacterial plaque involves the main apical foramen, compromising the vascular supply. Irritants from a diseased pulp may permeate readily through the apical foramen resulting in periapical pathosis. This results in destruction of periodontal tissue fibers and resorption of the adjacent alveolar bone and root.
Lateral canals: In addition to the apical foramen, which is the main route of communication, there are a multitude of branches connecting the main root canal system with the periodontal ligament. These ramifications are now currently termed as 'accessory canals'. The term accessory canal is now used to describe any ramification that connects the root canal system to the periodontal ligament. As the root develops, ectomesenchymal channels get incorporated, either due to dentine formation around existing blood vessels or breaks in the continuity of the Hertwigs root sheath, to become lateral or accessory canals. The majority of the accessory canals are found in the apical part of the root and the molar furcation areas. DeDeus evaluated 1140 teeth for accessory canals; frequency of ramifications found on the root surface were as follows: apical third 17%, coronal third 1.6% and body of the root 8.8%.[6] Bender et al. stated that periodontal endodontic problems were much more frequent in the molars than in the anterior teeth because of the greater number of accessory canals present in the molars. The percentage of lateral canals in the furcation is 46% in first molars[7] and 50 to 60% in any multirooted teeth.[8] Gutmann(1978) found 25.5% accessory canals in the furcation areas. Patent accessory canals are a potential pathway for the spread of microorganisms and their toxic byproducts, as well as other irritants, from the pulp to the periodontal ligament and vice versa, resulting in an inflammatory process in the involved tissues.
Tubular Pathways
Passage of microorganisms between the pulp and periodontal tissues is possible through the patent dentinal tubules, when the cementum layer is denuded. This is usually attributed to various developmental defects such as incomplete union of cementum and enamel at cement-enamel junction (CEJ), disease processes or surgical procedures involving root surfaces like root scaling and planning etc. Exposed dentinal tubules, in areas of denuded cementum may serve as communication pathways between the pulp and the periodontal ligament.
Nonphysiological Pathways
These include iatrogenic root canal perforations, vertical root fractures caused by trauma, pathway created due to resorption etc. The incidence of root fractures is more in the roots that are filled with lateral condensation technique and the teeth restored with intracanal posts.
Etiopathogenesis of Perio-Endo Lesions
Effect of periodontal lesions on the pulp
Microbial agents are the main cause in the evolution of perio-endo lesions along with the other etiologic factors involved. The formation of bacterial plaque on denuded root surfaces, following periodontal disease, has the potential to induce pathologic changes in the pulp through lateral or accessory canals. The effect of periodontal lesions on the pulp can result in atrophic and other degenerative changes like reduction in the number of pulp cells, dystrophic mineralization, fibrosis, reparative dentin formation, inflammation and resorption.
Atrophic changes: The pulp tissue of a periodontally involved tooth has cells which are small and have more collagen depositions than normal. Due to impaired nutrition, the pulp cells slowly degenerate. The death of the cell is so gradual that morphologic evidence sometimes appears to be lacking. The cause of these atrophic changes is the disruption of blood flow through the lateral canals, which leads to localized areas of coagulation necrosis in the pulp. These areas are eventually walled off from the rest of the healthy pulp tissue by collagen and dystrophic mineralization. With slowly advancing periodontal disease, cementum deposition may act to obliterate lateral canals before pulpal irritation occurs. This may explain why, not all periodontally involved teeth demonstrate pulpal atrophy and canal narrowing. Pressure atrophy may also occur because of mobility of these periodontally involved teeth.
Inflammatory changes: The causative agents of periodontal disease are found in the sulcus and are continually challenged by host defenses. An immunologic or inflammatory response is elicited in response to this microbiologic challenge. This results in the formation of granulomatous tissue in the periodontium. When periodontal disease extends from the gingival sulcus towards the apex, the inflammatory products attack the elements of the periodontal ligament and the surrounding alveolar bone.
A clear cut relationship between progressive periodontal disease and pulpal involvement, however, does not invariably exist. The most common periodontal lesion produced by the pulp disease is the localized apical granuloma. It is produced by the diffusion of bacterial products through the root apex, with the formation of vascular granulation tissue. Subsequently, resorption of the alveolar bone and occasionally of the root itself may occur.
Resorption: Resorption of the sides of the roots is frequently found adjacent to the granulation tissue overlying the roots. When the periodontal lesions are deep, resorption may also be found within the root canals, often opposite lateral canals, and at the apical foramen. Since this resorptive process extends into the dentin peripherally towards the pulp, and the activating factors are produced from the periodontal lesion, a name which reflects the etiology of this phenomenon, peripheral inflammatory root resorption (PIRR) was proposed. [9]
Effects of periodontal treatment procedures on the dental pulp
Scaling and root planing: This procedure removes the bacterial plaque and calculus. However, improper root planing procedures can also remove cementum and the superficial parts of dentin, thereby exposing the dentinal tubules to the oral environment. Subsequent microbial colonization of the root dentin may result in bacterial invasion of the dentinal tubules. As a consequence, inflammatory lesions may develop in the pulp. The initial symptom is sharp pain of rapid onset that disappears once the stimulus is removed.
Acid etching: During periodontal regenerative therapy, root conditioning using citric acid helps to remove bacterial endotoxin and anaerobic bacteria and to expose collagen bundles to serve as a matrix for new connective tissue attachment to cementum. Though beneficial in the treatment of periodontal disease, citric acid removes the smear layer, an important pulp protector. Application of citric acid may have a detrimental effect on the dental pulp.
Effects of endodontic infection on the periodontium
It has been demonstrated that intrapulpal infection tends to promote epithelial downgrowth along a denuded dentin surface. Also, experimentally induced periodontal defects around infected teeth were associated with 20% more epithelium than noninfected teeth. Noninfected teeth showed 10% more connective tissue coverage than infected teeth. Therefore, it is essential that pulpal infections be treated first, before undertaking periodontal regenerative procedures.
Classification of Endo-Perio Lesions
A. Classification according to Weine, based on etiology of the disease
Class 1- tooth in which symptoms clinically and radiographically simulate periodontal disease but are infact due to pulpal inflammation and/or necrosis.
Class 2- tooth that has both pulpal or periapical disease and periodontal disease concomitantly.
Class 3- tooth that has no pulpal problem but requires endodontic therapy plus root amputation to gain periodontal healing.
Class 4- tooth that clinically and radiographically simulates pulpal periapical disease but infact has periodontal disease.
B. The most accepted classification was given by Simon, Glick and Frank in 1972 .[10] According to this classification, perio-endo lesions can be classified into:
1. Primary endodontic lesion
2. Primary periodontal lesion
3. Primary endodontic lesion with secondary periodontal involvement
4. Primary periodontal lesion with secondary endodontic involvement
5. True combined lesion
Primary Endodontic Lesion
An acute exacerbation of a chronic apical lesion on a tooth with a necrotic pulp may drain coronally through the periodontal ligament into the gingival sulcus. This condition may clinically mimic the presence of a periodontal abscess. In reality, however, it would be a sinus tract originating from the pulp that opens into the periodontal ligament. Primary endodontic lesions usually heal following root canal therapy. The sinus tract extending into the gingival sulcus or furcation area disappears at an early stage, if the necrotic pulp has been removed and the root canals are well sealed.
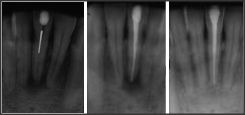 | (Radiograph showing primary endo lesion treated by root canal treatment only)
 |
Primary Periodontal Lesion
These lesions are caused primarily by periodontal pathogens. In this process, chronic periodontitis progresses apically along the root surface. In most cases, pulpal tests indicate a clinically normal pulpal reaction. There is frequently an accumulation of plaque and calculus and the presence of deep pockets may be detected.
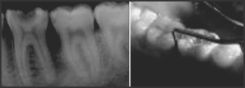 | (Radiograph showing generalized bone loss indicating a primary perio lesion, treated by perio intervention only)
 |
Combined Diseases
Primary endodontic lesion with secondary periodontal involvement
If a primary endodontic lesion remains untreated, it may become secondarily involved with periodontal breakdown. Plaque accumulation at the gingival margin of the sinus tract leads to plaque induced periodontitis in this area. When plaque and calculus are detected, the treatment and prognosis of the teeth are different from those of the teeth involved with only endodontic disease. The tooth now requires both endodontic and periodontal treatment.
 | After 3 wks of RCT & Debridement
 |
Primary endodontic lesion with secondary periodontal involvement may also occur as a result of root perforation during root canal treatment, or where pins and posts may have been misplaced during restoration of the crown. Symptoms may be acute, with periodontal abscess formation associated with pain, swelling, pus or exudates, pocket formation, and tooth mobility. A more chronic response may occur without pain, and involves the sudden appearance of a pocket with bleeding on probing or exudation of pus.
Root fractures may also present as primary endodontic lesions with secondary periodontal involvement. These typically occur in root canal treated teeth, often with posts and crowns. The signs may range from a local deepening of periodontal pocket to a more acute periodontal abscess formation.
Primary periodontal disease with secondary endodontic involvement
The apical progression of a periodontal pocket may continue until the apical tissues are involved. In this case, the pulp may become necrotic as a result of infection entering through lateral canals or the apical foramen. In single-rooted teeth, the prognosis is usually poor. In molar teeth, the prognosis may be better. Since not all the roots may suffer the same loss of supporting tissue, root resection can be considered as a treatment alternative.
If the blood supply circulating through the apex is intact, the pulp has good prospects for survival. It has been reported that pulpal changes resulting from periodontal disease are more likely to occur when the apical foramen is involved. In these cases, bacteria originating from the periodontal pocket are the most likely source of root canal infection.
The treatment of periodontal disease can also lead to secondary endodontic involvement. Lateral canals and dentinal tubules may be opened to the oral environment by scaling and root planing or surgical flap procedures. It is possible for a blood vessel within a lateral canal to be severed by a curette and for the microorganisms to be pushed into the area during treatment, resulting in pulp inflammation and necrosis.
 | Treatment and Prognosis of Endodontic-Periodontic Lesions
 |
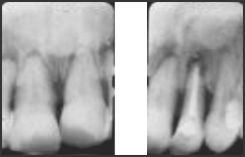
True Combined Lesion
True combined endodontic periodontal disease occurs less frequently than other endodontic-periodontal problems. It is formed when an endodontic lesion progressing coronally joins an infected periodontal pocket progressing apically.[10] The degree of attachment loss in this type of lesion is invariably large and the prognosis guarded. This is particularly true in single-rooted teeth. In molar teeth, root resection can be an alternative treatment. The radiographic appearance of combined endodontic periodontal disease may be similar to that of a vertically fractured tooth. If a sinus tract is present, it may be necessary to raise a flap to determine the etiology of the lesion.
Diagnosis
It is important to determine whether the primary lesion may be pulpal or periodontal, otherwise the wrong treatment may be chosen or there may be unnecessary overtreatment. Following diagnostic measures are undertaken to establish the correct diagnosis.
1) Vitality tests The first step would be to examine for vitality by pulp testing and with heat and cold. A nonvital tooth may indicate primary pulpal involvement, although at times, it can indicate secondary pulpal disease. Endodontic treatment (RCT) is required in this situation. A vital tooth indicates primary periodontal involvement, and does not require endodontic therapy. Clinician should be cautious about the possibility of false positive results also.
2) Radiographic evaluation Radiograph may exhibit loss of bone at the alveolar crest, an apical radiolucency, or a continuous bone loss involving both sites. Apical radiolucency indicates primary pulpal disease. Bone loss confined to coronal one third of the tooth is associated with primary periodontal disease. Finding the cause is more difficult when bone loss is present at both sites. If the tooth has a radiographic furcation involvement that cannot be detected clinically, there is likelihood of pulpal involvement. Gutta-percha points used as probes in sinus tracts can be a valuable aid in tracing the origin of a draining lesion.
3) Pain and abscess formation Clinical signs and symptoms will help to differentiate endodontic and periodontal lesions.
a) Periodontal abscess may produce a dull, more even pain accompanied by a feeling of fullness in the area or may present as a high tooth. Pulpal pain is usually sharp.
b) Pulpal lesion may be difficult to localize when the symptoms start. The periodontal lesion is usually easy to localize.
c) Pulpal lesion usually drain by a fistula through the alveolar mucosa or gingiva, it rarely fistulates through the sulcus. The periodontal abscess usually drains through the lumen of the pocket.
4) Pocket depth The presence of a deep solitary pocket in the absence of periodontal disease may indicate the presence of a lesion of endodontic origin or a vertical root fracture. Periodontal probing helps in differentiating between endodontic and periodontal disease. It can also be used to track a sinus resulting from an inflammatory periapical lesion that extends cervically through the periodontal ligament space. In periodontal lesions, numerous defects are present throughout the mouth and
[Image 6]
subgingival calculus can be detected. A pocket that does not extend to the apical one third of the root in a periodontally involved mouth also indicates primary periodontal disease.
Discussion and Conclusion
Treatment and prognosis of primarily endodontic and primarily periodontal disease is very straightforward. However, prognosis of combined forms of the lesions is more difficult to predict. Endodontic therapy is more predictable and completion of this therapy before periodontal procedures has a positive effect on periodontal healing. In conclusion, it is essential to understand that in endo-perio lesions, the endodontic treatment is the more predictable of the two. However the success of endodontic therapy is dependent on the completion of periodontal therapy. The complete treatment of both aspects of endo-perio lesions is essential for successful long-term results.
References
1. Simring M, Goldberg M. The pulpal pocket approach: Retrograde periodontitis. J Periodontol 1964;35:22-48.
2. Kipioti A, Nakou M, Legakis N, Mitis F. Microbiological findings of infected root canals and adjacent periodontal pockets in teeth with advanced periodontitis. Oral Surg Oral Med Oral Pathol 1984;58:213-20.
3. Kobayashi T, Hayashi A, Yoshikawa R, Okuda K, Hara K. The microbial flora from root canals and periodontal pockets of non vital teeth associated with advanced periodontitis. Int Endod J 1990;23:100-6.
4. Bergenholtz, Lindhe J. Effect of experimentally induced marginal periodontitis and periodontal scaling on the dental pulp. J Clin Periodontol 1978;5:59-73.
5. Zehnder M, Gold SI, Hasselgren G. Pathologic interaction in pulpal and periodontal tissues. J Clin Periodontol 2002;29:663-71.
6. DeDeus QD. Frequency location and direction of the lateral, secondary and accessory canals. J Endod 1975;1:361-6.
7. Vertucci FJ, Williams RJ. Furcation canals in the human mandibular first molars. Oral Surg 1990;69:743.
8. Rahmat A, Barkhordar, Stewart GG. The potential of periodontal pocket formation associated with untreated accessory root canals. Oral Surg Oral Med Oral Pathol 1990;70:769-72.
9. Gold S, Hasselgren G. Peripheral inflammatory root resorption: A review of literature with case reports. J Clin Periodontol 1992;19:523-34.
10. Simon JH, Glick DH, Frank AL. The relationship of endodontic-periodontic lesions. J Clin Periodontol 1972;43:202.
11. Newman, Takei, Klokkevold, Carranza. Clinical Periodontology 10 th ed. Saunders; 2006. p. 88-90
12. Schilder H. Endodontic-periodontal therapy. In: Grossman LI, editor. Endodontic Practice, 6 th ed. Philadelphia: Lea and Febiger; 1965. |