Introduction
The ectodermal dysplasias (EDs) are complex group of diseases, first described by Thurnam in 1848. In the last 10 years more than 170 different pathological clinical conditions have been recognized and defined as EDs, all sharing in common anomalies of the hair, teeth, nails, and sweat glands. Many are associated with anomalies in other organs and systems and, in some conditions, with mental retardation. The anomalies affecting the epidermis and epidermal appendages are extremely variable and clinical overlap is present among the majority of EDs.[1]
Ectodermal dysplasia is a relatively rare disorder, with a frequency varying between 1:10,000 and 1:100,000 live births, and is more frequent in males. The majority of cases follow the autosomal-recessive mode of inheritance, but it can also be autosomal-dominant or X-linked[2],[3]
These disorders are clinically divided into hidrotic and anhidrotic forms and each of these forms is subdivided into different syndromes based on the presence or absence of hair defects, tooth abnormalities, nail deformities, deafness, palmoplantar keratoderma and other features. [4], [5]
Freire-Maia and Pinheiro have proposed a classification based on the involved ectodermal derivative. In this classification, '1' indicates hair dysplasia, '2' dental dysplasia, '3' nail dysplasia and '4' sweat gland dysplasia. [6] Based on this, there are more than ten subgroups in Freire-Maia and Pinheiro classification [7]
Since our patient had abnormality in hair, teeth, nail and sweat gland function, his ectodermal dysplasia fits in 1-2-3-4 subgroup.
Case Report
A 5-year-old boy was seen with the complaint of oligodontia with few primary teeth missing, angular cheilitis and painful ulcers on oral mucosa In infancy, he had sparse, fine silky hair, thinly covering the scalp, thin eyebrows, narrow nose at the tip, folded lower eyelid, thick lower lip. Normal nails, and no genital, breast or ocular anomalies.
Family history revealed that his aunties had few primary teeth missing. Grandfather also present same features of Ed, partial anodontia.
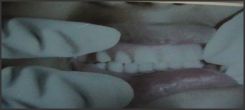
The intraoral examination revealed bone atrophy of the alveolar ridges, on both the maxilla and the mandible, and numerous dental gaps. Some of the existing teeth were short, conical and pointed (Fig 1) .
Orthopantomograph: displaying numerous agenesis in the primary dentition, having less than half the normal number (oligodontia), delayed eruption, and missing permanent teeth (Fig. 2). Therefore, this is a case of recessive, X-linked hypohidrotic ectodermal dysplasia.
An acceptable solution to this complex case was sought, considering the young age of the boy, and the emotional state of the mother, worried by the absence of numerous teeth.
Under these conditions, the earliest possible prosthetic treatment was evaluated, on the one hand to limit the resorption of the alveolar ridges, and on the other to minimize the emotional and psychological impact created by the lack of teeth on the child's relationships [3],[8].
Treatment started with morphological modifications using photopolymerizable composite material to some of the conical teeth in order to improve the esthetics and to aid retention of the prothesis.
It was considered appropriate to make a lower and upper acrylic partial prosthesis (Fig. 4) This design allows modifications to be made as and when necessary, as well as providing a reasonable esthetic result, an acceptable masticatory function on complementing the lack of dentition, at the same time as attempting to maintain the alveolar ridges free of atrophy, and allowing an almost normal social life, which is so important at this stage in a child's personal and psychological development.
The importance of oral hygiene as a fundamental aspect of dental prognosis for these patients was stressed to the parents, in the sense that they monitor brushing control the eating of sweets and snacks between meals as far as possible. Periodic check ups were prescribed, approximately once every six months, at which topical applications of fluoride gel
 | Fig 1 Short, conical primary teeth at 5 years of age
 |
 | Fig 2 Orthopantomogram showing oligodontia, missing permanent teeth
 |
 | Fig 3 clinical presentation of pt at 10 years of age
 |
 | Fig Upper and Lower acrylic denture in occlusion
 |
were to be applied as well as making small adjustments and modifications to the prosthesis.
At present , patient is of 10 year old. We are following the eruption of a still unerupted tooth, as well as insisting on good hygienic measures of daily brushing and mouth rinse, topical fluoride applications every six months, periodic check ups etc. (Fig. 3, 4).
Discussion
Ectodermal dysplasias are non-progressive, diffuse, congenital genodermatoses, characterized by a lack or scarcity of hair, teeth, nails and sweat glands, to which can be added defects in the external morphology (nose, outer ears, and lips), disorders of the CNS, alterations of the eyes; anomalies in the oronasal mucosa and in melanocytes.
The most frequently observed types of ectodermic dysplasia are the hypohidrotic-anhidrotic, and the hidrotic. The hypohidrotic-anhidrotic type, or Christ-Siemens- Touraine syndrome was first described in 1848 by Thurman, and is characterized by the triad of hypotrichosis (skin, hair and nail anomalies), either hypodontia or anodontia, and hypohidrosis (partial or total absence of eccrine sweat glands) and other features such as frontal bossing, saddle-shaped nose, everted lips etc[9]
The hidrotic type was first defined in 1929 by Clouston, and is distinguished by hypotrichosis, ungual dystrophy and hyperkeratosis of the palms and soles [10]
Recently, a new classification for ectodermal dysplasia has been proposed, based on the alterations in the proteic molecular functions that lie behind it [5]
Transmission of hypohidrotic ectodermal dysplasia is, in general, X-linked (females carry the responsible gene, and males suffer from the disease, although the carrying mothers usually bear some typical characteristic feature of the disease) and at times in autosomal recessive form.
A prosthodontic rehabilitation is fundamental in these situations, attempting to provide a functional and esthetic solution that will allow the child as normal a life-style as possible, without damaging self-esteem or psychological development and ensuring that behaviour is unaffected.
Treatment should be commenced as soon as possible in order to avoid possible resorption and atrophy of the alveolar ridges, and to control the vertical dimension, which can be severely affected by the total or partial lack of teeth.
Different authors have proposed different rehabilitation possibilities for these patients. In general, almost all agree in recommending the use of removable prostheses during the first stages of growth (3-5 years), allowing the adjustment of the vertical dimension or maxilla / mandible interrelationship.
From our point of view, the use of partial acrylic prostheses is an interesting and practical alternative that provides a relatively quick, easy, acceptable and economical solution to the functional and esthetic oral rehabilitation in patients
with pronounced edentulism. This solution improves the patient's quality of life and optimizes social integration; furthermore, it permits stimulation of the alveolar ridges for later treatment with an implant supported prosthesis as a more stable and esthetic solution for patients with multiple dental agenesis.
References
1. M. Tariq, M. S. Chishti, G. Ali, W. Ahmad: A Novel Locus for Ectodermal Dysplasia of Hairs, Nails and Teeth Type Maps to Chromosome 18q22. Annals of Human Genetics.2008;72 (1);19-25
2. Adolfo P. V. et al Treatment with removable prosthesis in hypohidrotic ectodermal dysplasia: A clinical case Med Oral Patol Oral Cir Bucal. 2008; 13(2):E119-23.
3. Della Valle D, Chevitarese AB, Maia LC, Farinhas JA: Alternative rehabilitation treatment for a patient with ectodermal dysplasia. J Clin Pediatr Dent. 2004;28(2):103-6.
4. Akhyani Maryam, Kiavash Katrin: Ectodermal dysplasia with alopecia, onychodysplasia, hypohidrosis, keratoderma, abnormal teeth and deafness. IJDVL: 2007;73(6): 409-411
5. Lamartine J. Towards a new classification of ectodermal dysplasias: Clin Exp Dermatol 2003;28:351-5.
6. Pinheiro M, Freire-Maia N. Ectodermal dysplasias: A clinical classification and a causal review. Am J Med Genet 1994;53:153-62.
7. Itin PH, Fistarol SK. Ectodermal dysplasias: Am J Med Genet C Semin Med Genet 2004;131C:45-51
8. Alvarez E, et al: Displasia ectodérmica hipohidrótica: características dentales en 11 casos. Arch Odontoestomatol 2004;20:455-62.
9. Campuzano S, Santos-Juanes J, Medina A, Sanchez J: Displasia ectodérmica hipohidrótica. An Pediatric 2005;62:393-4.
10. Sweeney IP, Ferguson JW, Heggie AA, Lucas JO: Treatment outcomes for adolescent ectodermal dysplasia patients treated with dental implants. Int J Paediatr Dent. 2005 Jul;15(4):241-8. |