Introduction:
Unicysticameloblastomais considered tobe a less aggressive variant ofameloblastoma and simple enucleation was suggested as treatment. However, theterm unicysticameloblastoma was adopted in the second edition of theinternational histologic classification of odontogenictumors and encompasses lesions previously referred to as cystic ameloblastoma, ameloblastoma associated with dentigerous cyst, cysto genicame loblastoma, extensive dentigerous cyst with intracysticame loblastic papilloma, dentigerous cyst withameloblastomatous proliferation, ameloblastoma developing in a radicular (orglobulomaxillary) cyst, luminal ameloblastomas, mural ameloblastomas andameloblastomas arising in dentigerous cysts. It refers to those cystic lesionsthat show clinical, radiographic or gross features of jaw cyst, but on histologicexamination shows typical ameloblastomatous epithelium, lining part of thecystic cavity with or without luminal and / or mural tumor growth[1],[2].
Case Report:
A 35 years old male patient reported to department with a chief complaint of swelling on right lower third of face since 6 months, which was small in size and slowly progressed to present size, not associated with pain, no difficulty in chewing and speaking (jaw movements), no history of trauma or fever.No history of discharge and paraesthesia.
Extraorally on inspection, a single well defined swelling was present on right lower third of face extending anterio posteriorly from 1 cm behind the angle of mouth to anterior border of ramus and superioinferiorly from line drawn to angle of mouth from tragus of ear to inferior border of mandible, measuring about 3X2 cm. Overlying skin was smooth, stretched and of normal colour.All inspectory findings were confirmed. On palpation, swelling was non-tender, hard in consistency and not fixed to overlying skin. Submandibular lymphnodes were palpable, two in number, non tender and mobile.
Intraorally on inspection, a solitary diffuse swelling was present extending from 45 to ramus area.Swelling caused buccal cortical plate expansion, lingual side was not involved. Overlying mucosa was stretched, smooth and of normal colour without any dilated superficial veins.There was obliteration of buccal vestibule extending up to occlusal surface of 47 and 46 was missing. On palpation, all inspectory findingswere confirmed. The swelling was non tender on palpation, hard in consistency except in distal to 45 and distal to 47 region (firm to soft in consistency). There was no tooth mobility in relation to 47 (Fig.-1).
 | Fig - 1
 |
 | Fig - 2
 |
Based on history and clinical examination, provisional diagnosis of ameloblastoma of right side of mandible was made. Dentigerous cyst and odontogenic keratocyst were considered as differential diagnosis. Aspiration was done from soft to firm area (decorticated area) and straw colored fluid was obtained (Fig-2).
OPG revealed impacted 48 which were displaced to inferior border of mandible. A multilocular radiolucency (soap bubble) was seen extending from 46 (edentulous region) to coronoid process.There was complete loss of bony margin of the anterior border of ramus without any root resorption (Fig-3).
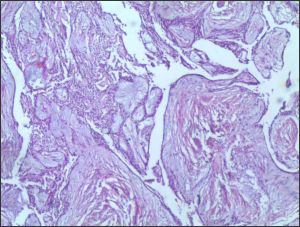
Enucleation was done and specimen was sent for histopathological examination which revealed unicysticameloblastoma.
Discussion:
Ameloblastoma accounts for 1% of all the tumours. They are slow growing, expansile tumour producing deformity, locally aggressive and has a moderate recurrence rate.
Ameloblastoma is classified into four distinct categories based on the behaviour, these are:
(1) Solid or multicystic
(2) unicystic
(3) peripheraland
(4) desmoplastic variety.
UA is a less encountered variant of the ameloblastoma. It is almost exclusively encountered asymptomatically in the posterior mandible. Unicysticamelo
 | Fig - 3
 |
 | Fig - 4
 |
blastomas are most often seen in young patients with about 50% of such tumors diagnosed during the second decade of life. More than 90% of UA are found in the mandible, usually in the posterior region followed by parasymphysis region, anterior maxilla and posterior maxilla. The lesion is often asymptomatic, although a large lesion may cause painless swelling of the jaw and accounts for 10-15% of all intraosseousameloblastomas in various studies[3].
Unicystictumors include those that have been variously referred to as mural ameloblastoma, luminal ameloblastoma, and ameloblastoma arising in dentigerous cyst.
Leider et al proposed three pathologic mechanisms for evolution of unicystic ameloblastoma:[1],[2]
a. The reduced enamel epithelium associated with a developing tooth undergoes ameloblastic transformation with subsequent cystic development.
b. Ameloblastomas arise in dentigerous or other types of odontogenic cysts in which the neoplastic ameloblastic epithelium is preceded temporarily by a non-neoplastic stratified squamous epithelial lining.
c. A solid ameloblastoma undergoes cystic degeneration of ameloblastic islands with subsequent fusion of multiple micro cysts and develops intoa unicystic lesion.
Completely cystic may be related to epithelial dysadhesion (eg. Defective desmosomes) or more likely intrinsic production of proteinases (eg. Metalloproteinases, serine protineases ).
The radiographical features of UA are typicallyunilocular and there is a round area of radiolucency. Therefore, this lesion is oftenmisdiagnosed as an odontogenic keratocyst or a dentigerous cyst. As compared to this, in our case we found multilocular radiolucency with impacted 48 which makes the use of the term "cystic ameloblastoma" more appropriate. One of the efficient diagnostictools which can be used to detect UA is contrastenhanced (CE)-MRI. It is done to diagnose the cases of unilocular, round radiolucent lesionswhich can be visualized by panoramicradiography and/or CT. In the cases of UA, lowsignal intensity (SI) is observed on the T1-weighted images (WIs), a markedly high SI isobserved on the T2WIs; and a relatively thickrim-enhancement with/without smallintraluminal nodules is observed on the CET1WIs.CE-MRI is considered to be useful in the diagnosis of UA[4].
Apart from CE -MRI, another importantdiagnostic tool for detecting UA isimmunohistochemistry. By this, one candifferentiate UA from other types ofameloblastomas. The expression ofproliferating cell nuclear antigen (PCNA) is markedly observed in the tumors cells of othertypes of ameloblastomas, whereas there is noexpression of PCNA in the cells of any variantsof UA. Moreover, β-catenin was characterizedby a more positive marked expression in the UAthan in other types of ameloblastoma and thecells that expressed this substance were not PCNA positive cells. This distinguishes UAfrom other ameloblastomas[4],[5].
Histologically minimumcriterion for diagnosis of unicysticameloblastoma is demonstration of cysticsac lined by ameloblastomatous epithelium. Ackermann et al. classified
unicysticameloblastoma into 3 histological groups[1],[6].
Group I: Luminal Unicysticame loblastoma (tumor confined to luminalsurface of the cyst).
Group II: Intraluminal / Plexiformuni cysticame loblastoma (nodularpro liferation into the lumen without infiltration of tumor cells into theconnective tissue wall).
Group II: Mural unicysti cameloblastoma (invasive islands ofameloblastomatous epithelium in the connective tissue wall notinvolving the entire epithelium).
The above classification was modified further by Philipsen and Reichart as[1],[6]
Subgroup 1 - luminal unicysti camelo blastoma.
Subgroup 1.2 - luminal and intraluminal
Subgroup 1.2.3 - luminal, intraluminal and intramural
Subgroup 1.3 - luminal and intramural.
The UAs diagnosed as subgroups 1 and 1.2 can betreated conservatively (carefulenucleation), whereassubgroups 1.2.3 and 1.3 showing intramural growthsrequire treated radical resection, as for a solid or multicysti came loblastoma.Following enucleation, vigorouscurettage of the bone should be avoided as it mayimplant foci of ameloblastoma more deeply into bone.Chemical cauterization with Carnoy's solution is alsoadvocated for subgroups 1 and 1.2. Subgroups 1.2.3 and 1.3 have a high risk for recurrence, requiring moreaggressive surgical procedures. This is because the cysticwall in these cases has islands of ameloblastomatumorcells and there may be penetration into the surrounding cancellous bone[2],[6].
Conclusion:
The diagnosis of UA was based on clinical andhistopathologic features. UA is a tumour with strong propensity for recurrence, especially when the ameloblastic focus penetrates the adjacent tissue from the wall of the cyst. The challenge is in the diagnosis of UA in early stage soas to prevent large multilating bony and soft tissue defects and recurrence.
References:
1. Philipsen HP, Reichart PA. Unicysticameloblastoma. In: Odontogenictumors and allied lesions. P.77-86: Quintessence Pub.Co.Ltd, 2004.
2. Kokila G, LaxmideviBl, JyothiMahadesh. Unicystic and solid type of ameloblastoma occurring in same person- A rare case. Image 2010;10(5):10-19.
3. VJ Paikkatt, S Sreedharan, VP Kannan. Unicysticameloblastoma of the maxilla: A case report. J Indian SocPedodPrev Dent 2007;25:106-10.
4. Meetkamal, ParwinderKaur. An unusual case of UnicysticAmeloblastoma involving the anterior of maxilla. Journal of clinic and diagnostic Research 2010;4:3659-63.
5. JyothiMahadesh, Dilip Kumar Rayapati, Prathima M Maligi, PrashanthRamachandraUnicysticameloblastoma with diverse mural proliferation - a hybrid lesion. Imaging Science in Dentistry 2011;41:29-33.
6. Rakesh S Ramesh, SurajManjunath, Tanveer H Ustad, SairaPais, K ShivakumarUnicysticameloblastoma of the mandible - anunusual case report and review of literature. Head and Neck Oncology 2010;2:1. |