Introduction:
Fractures of facial bones in children are relatively infrequent. Children are usually susceptible to craniofacial trauma because of their greater cranial mass to body ratio[1]. At birth, the ratio between cranial volume and facial volume is approximately 8:1. By the completion of growth, this ratio becomes 2.5:11. Children are more prone to cranial injuries than mid-face and mandibular fractures. The facial injuries can range from minor inconvenience to life time disfigurement. Timely and suitable management of these injuries is crucial for the successful clinical outcome for the patient. Treatment is usually performed without delay and can be limited to observation or closed reduction in non-displaced or minimally displaced fractures.
Case Report:
A 5 year old girl reported to the department of Pedodontics, PMVIDS, Hyderabad, with history of trauma in the mandibular anterior region 3 days back. The patient was conscious, well oriented to time, place and person. There was no history of convulsions or vomiting.
Extra oral examination revealed, diffuse facial oedema. Step defect was palpable in the left parasymphysis region with bruising of the overlying skin(Figure 1). Tenderness could be elicited along the lower border of the mandible over the same area.
Intra oral examination revealed restricted mouth opening with a deep wound in the left parasymphysis region in between lateral incisor and canine associated with bleeding and mobility of the fractured fragments. (Figure 2) Derangement of occlusion and subluxated primary right maxillary lateral incisor were present.
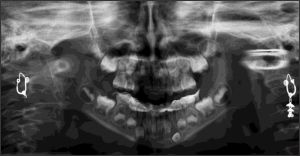
Panoramic radiograph revealed a fracture line running down the left parasymphysis region between 72 and 73 involving the alveolus and lying distal to the developing left permanent canine (Figure 3). There was no evidence of fracture clinically or radiographically in
 | Figure 1: Extra Oral Examination Revealed, Diffuse Facial Oedema.
 |
any other region.
On the basis of panoramic radiographic findings and clinical examination provisional diagnosis was made as unilateral left parasymphysis fracture of the mandible.
 | Figure 2: Deep Wound In The Left Parasymphysis Region In Between Lateral Incisor And Canine Associated With Bleeding And Mobility Of The Fractured Fragments.
 |
 | Figure 3: Panoramic Radiograph Revealing A Fracture Line Running Down The Left Parasymphysis Region Between 72 And 73.
 |
 | Figure 4: Cap Splint Placed On Mandibular Arch.
 |
 | Figure 6: Mild Inflammation Of Gingival After Removal Of The Splint.
 |
 | Figure 5: Panoramic Radiograph After 3 Weeks Showing Callous Formation.
 |
 | Figure 7: Post Panoramic Radiograph After 4 Weeks.
 |
Management:
Under local anaesthesia upper and lower alginate impressions were made and stone casts was poured. Casts were occluded to check for occlusal derangement. After occluding the upper and lower casts anterior open bite and posterior cross bite were noticed. When parents were questioned, they stated that the child has thumb sucking habit since 3 years. This made our treatment plan little more difficult to check for occlusion and any deviation in opening the jaw. A cap splint with clear acrylic was fabricated on the mandibular cast. The fracture was immobilized with the cap splint cemented on the mandibular arch (Figure 4). Subluxated primary maxillary right lateral incisor was extracted because of poor prognosis. Patient was advised to be on liquid and soft diet along with medication. Oral hygiene instructions were given. Patient was recalled for review.
A post operative panoramic radiograph was taken after 3 weeks which showed callus formation and absence of step defect along the lower border of mandible (Figure 4). The cap splint was removed after 4 weeks. Mild inflammation of gingiva was present (Figure 5). Patient advised to continue on soft diet and oral hygiene instructions given. A deviation of the mandible to the left side was noticed while closing the mouth (Figure 6, 7, 8). Instructions were given to occlude properly (Figure 9). Further treatment for crossbite correction is being considered.
Discussion:
Facial fractures are the most common type of injuries suffered by pediatric patients. The most common causes of fracture in children were falls (64%),
 | Figure 8: Photograph After 4 Weeks
 |
 | Figure 9
 |
followed by traffic (22%) and sports-related accidents (9%) [2]. The girl-to-boy ratio is 3:5, and the mean age was 7 +/- 4.4 years [3]. The most common facial fracture is fracture of mandible (32.7%) followed by nasal (30.2%), and maxillary/zygoma (28.6%) [4]. Patients with a fracture of the mandible were most likely to have a dental injury (39.3%) [5]. Another peak in incidence occurs during puberty and adolescence with increased unsupervised physical activity and sport. Symphysis and parasymphysis fractures account for 15-20% [6].
Management of mandibular fractures in children, though complex have to be treated very efficiently without damaging the underlying permanent tooth crypts or altering the mandibular growth which has a great significance on future facial development.
If the fracture line is within the tooth bearing area of the mandible and the tooth buds within the mandible do not allow internal fixation with titanium plates and screws, a mandibular cap splint can be used. If there is any doubt about the security of the splint then it can be reinforced by means of two circum-mandibular wires. Accordingly, the goal of treatment in primary dentition is to restore the underlying bony architecture to its pre-injury position in a stable fashion as non-invasively as possible with minimal residual esthetic and functional impairment [5],[7]. Children have greater osteogenic potential and faster healing rates than adults. Therefore, anatomic reduction in children must be accomplished earlier and immobilization times should be shorter (2 weeks versus 4-6 weeks in adult)[8]. Displaced mandibular fractures need to be reduced and immobilized and a long-term follow-up is necessary to monitor any potential growth abnormalities.
The acrylic splint consists of intermaxillary, lingual and labiolingual types that hold a dental arch and a cap type that covers the dental arch. The intermaxillary type is indicated for the loss of multiple teeth, the lingual type for the predicted intraversion of bone fragments and the labiolingual as well as cap types for the deciduous and mixed dentition.
The cap splint is suggested to be cemented only on non traumatised teeth, leaving the injured teeth free within the splint in order not to damage them when the splint is removed 8. Use of a cap splint in pediatric parasymphysis mandibular fracture is a definitive treatment modality with a conservative approach.
Pediatric dentists before going ahead with any kind of surgical intervention for the treatment of pediatric mandibular fractures, utmost priority should be given for a conservative treatment plan keeping in mind the anatomical complexity of the developing mandible.
References:
1. Frazer JE. The skull: general account. In: Breathnach AS, ed: Anatomy of the human skeleton. London: J &A. Churchill ltd 1965:161-181.
2. Nicole ME, Holzle A, Zachariou Z, Lizuka T. Pediatric craniofacial trauma. J Oral Maxillofac Surg. 2008 Jan; 66 (1): 58-64.
3. Gassner R, Tuli T, Hachi O, Moreira R, Ulmer H. Craniomaxillofacial trauma in children: a review of 3,385 cases with 6,060 injuries in 10 years. J Oral Maxillofac Surg. 2004 Apr; 62(4):399-407.
4. Imahara SD, Hopper RA, Wang J, Rivara FP, Klein M. Patterns and outcomes of pediatric facial fractures in the united states: a survey of the national trauma data bank. J Am Coll Surg. 2009 Feb; 208(2): 325.
5. John B, John RR, Stalin A, Elango I. Management of mandibular body fractures in pediatric patients: A case report with review of literature. Contemp Clin Dent. 2010; 1: 291-6.
6. Kale PT, Urolagin S, Motwani NB, Lingraj JB. Management of mandibular fracture in children with open cap splint. A treatment modality. IJCD. 2011 Jan; 2(1):69-72.
7. Aizenbud D, Molina HH, Emodi O, Rachmiel A. The management of mandibular body fractures in young children. Dental Traumatol. 2009; 25: 565-70.
8. Zimmermann CE, Troulis MJ, Kaban LB. Pediatric facial fractures: Recent advances in prevention, diagnosis and management. Int J Oral Maxillofac Surg. 2006; 35:2-13. |