Introduction
Root fracture which is classified as Ellis' class VI fracture, is a combined injury of pulp, dentine, cementum and periodontal ligament and is a relatively rare form of dental injuries, occurring in 0.5 to 7% of cases. They occur most commonly in 11-20-year age group and may be associated with fracture of the alveolar process. They most often occur in the maxillary central incisors of male patients and are frequently seen in the middle third of root followed by apical and coronal third fractures.[1] The classification of horizontal root fractures is based on the location of the fracture line and on the degree of dislocation of the coronal fragment.[2]
The prognosis of the tooth concerned is influenced by many factors, such as the patient's age, stage of root growth, mobility of the coronal fragment, and diastasis of the fragments. Communication between the palatal sulcus and the fracture line can additionally negatively influence the prognosis. [2] In 1958, Lindahl observed that root fractures could heal even after endodontic treatment of the tooth.
Basically, four types of conservative endodontic treatment have been described for the treatment of root fractures: cleansing and obturation of the coronal root fragment only; cleaning and obturation of the root canal in both the fragments; cleaning and obturation of the root canal of the coronal fragment and surgical removal of the apical fragment; and treatment of the root canal with calcium hydroxide followed by obturation. [3] The sequelae to root fractures may be divided into four categories:
Healing with cementogenic or calcified tissue,
Healing with interproximal dense connective tissue,
Healing with interproximal bone and connective tissue,
Interproximal inflammatory tissue without healing [4].
It has been shown that 20% to 40% of teeth with fractured roots eventually undergo pulpal necrosis, usually limited to the coronal fragment. [5] This case report illustrates the optimal treatment of root fracture where coronal fragment was necrotic.
Case Report
A 40 year old male reported to the Department of Conservative Dentistry and Endodontics at Bhojia Dental College and Hospital, for the treatment of discolored upper anterior teeth. He gave the history of road accident two years back, in which he suffered a blow on his permanent maxillary central incisors. At the time of injury, the patient complained of pain in his maxillary central incisors and slight tenderness to apical palpation but it subsided in few days. The clinical examination revealed crown discoloration of maxillary left central incisor. The radiographic examination showed horizontal root fracture in the middle third of the maxillary left central incisor (Fig 1). Periodontal pathosis at the fracture lines was also evident. The radiolucency extended upto the lateral surface of left lateral incisor. Lamina dura of both the incisors was not intact. Thermal tests and electric pulp tests gave negative response.
The surgical removal of apical fractured segment of maxillary central incisor was planned, but the patient was not willing for the surgical treatment. So the decision was made to start endodontic therapy on these teeth. At the same visit the access preparation was done for both the teeth. The pulp of the coronal fragment of central incisor was necrotic and was removed to the fracture line with number ISO 40 K-type file and the root canals were irrigated with 2.5 vol.% sodium hypochlorite solution. Working length was established by subtracting 0.5mm from the fracture line of tooth in central incisor. Grove discussed the importance of always filling the root canal to the dentinocemental junction (DCJ), which is "a definable point in all cases [6]. According to Kuttler, the root canal should be filled as far as 0.5 mm from the foramen because the average distance from the minor diameter to the foramen is roughly 0.6 mm6. But as there is no apical constriction at the coronal end of fractured central incisor, so after determining the diameter of apical opening by apical gauzing which came out to be 0.4mm, a mechanical barrier was created by biomechanical preparation upto master apical file ISO 80K file. Regular biomechanical preparation was done upto ISO size 60 in lateral incisor.
Following biomechanical preparation, the canals were irrigated with 3 ml of 17% EDTA solution and final irrigation was done with 2% chlorhexidine. Canals were dried with absorbent paper points and mixture of calcium hydroxide and iodoform (metapex) was placed in left maxillary central incisor while the coronal access was temporarily restored with cavit. The lateral incisor was obturated with gutta percha and Zinc
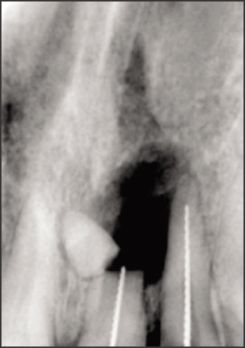 | Fig 1. Fractured Segment Of Central Incisor
 |
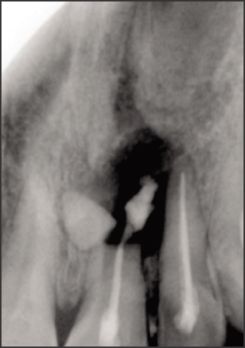 | Fig 2. Metapex Pushed Out Of Root Canal Of Central Incisor
 |
 | Follow Up Radiograph After 1 Month
 |
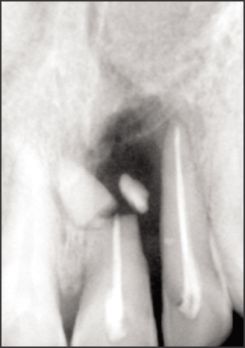
 | Fig 3. Post Obturation Iopar Of Both Incisors
 |
 | Follow Up Radiograph After 1 Year
 |
oxide based sealer using lateral compaction technique. At the subsequent visit two weeks later, the tooth was asymptomatic.
The coronal fragment of maxillary central incisor was obturated after 1 month with gutta-percha and zinc oxide eugenol based sealer, using the lateral compaction technique. The coronal access of the canal was closed with Cavit. Patient was recalled for follow up visits, in which the radiographs showed that the root fracture of the central incisor had healed with calcified tissue. After a 1-year follow-up, the radiograph showed that, there was definite evidence of repair at the fracture site with reduced radiolucency.
Discussion
The root fracture involves the cementum, dentin and pulp. The fracture line or lines may be well within the bony support, in which case it is considered a deep root fracture or the fracture line is at or close to the crestal bone of the alveolus and then it is called a shallow root fracture. Mid-root fractures occur most frequently in the upper anterior teeth due to their position in the arch. Cavalleri & Zerman and Caliskan & Pehlivan verified that maxillary incisors were the teeth most often affected by crown and root fractures (95%), respectively. The most common type of root fracture was in the middle third of the root (57%) followed by apical part (34%) and coronal part (9%)[5].The prognosis of these root fracture vary, as many factors play an important role in influencing the outcome and pattern of repair [1], [5].
This case report presents a deep horizontal root fracture in the middle third with periodontal ligament injury. This condition had persisted for almost two years without treatment. This kind of fracture may heal spontaneously or may result in pulp necrosis of the coronal segment.
The rate of pulp necrosis in teeth with root fractures varies from 20% to 44 % [5]. Al-Nazhan et al.[7] verified pulp necrosis in 100% of cases of crown-root fractures and in 43.7% of horizontal root fractures. In 1967, Andreasen and Hjorting-Hansen found that necrosis of the pulp usually occurs only in the coronal fragment, while the pulp of the apical fragment remains vital [8].
It has been shown in monkeys that resorption of bone occurs only when the necrotic pulp becomes infected[9]. Unlike coronal fractures involving the pulp, in root-fractured teeth there is no contamination of the pulp at the time of injury. The source of subsequent infection has not been established, but infection would not appear to be blood borne[10]. It could occur via the periodontal ligament, with bacteria reaching the pulp via the fracture line or through cervical dentinal tubules. Root-fractured teeth often possess a vital apical fragment, even when the coronal fragment is necrotic.
Bacteria have long been recognized as the primary etiologic factors in the development of pulp and periapical lesions. Irrigants augment mechanical debridement by flushing out debris, dissolving tissue, and disinfecting the root canal system [11]. Irrigating solutions used in this case were sodium hypochloride with EDTA and chlorhexidine as final solution. NaOCl is a potent antimicrobial agent, killing most bacteria instantly on direct contact. Though hypochlorite is the only root-canal irrigant of those in general use that dissolves necrotic and vital organic tissue[12] but it does not remove the smear layer. It affects the organic part of the smear layer, thus making its complete removal possible by subsequent irrigation with EDTA. EDTA and Citric Acid effectively dissolve inorganic material, including hydroxyapatite [12]. Chlorhexidine appears to be the most promising agent to be used as a final irrigant. In a randomized clinical trial, a 2% chlorhexidine solution, used as a final irrigant, significantly decreased bacterial loads in root canals that had been irrigated with sodium hypochlorite during canal preparation.
In this case there is no natural apical constriction or stop against which a suitable root filling material can be placed to prevent re-infection of this space. Therefore one of the aims of the treatment was to produce a barrier, against which a root canal filling material could be placed thereby preventing the extrusion of material into the surrounding tissues as well as providing a restoration that reinforces or strengthens the weak immature dentinal root walls in an attempt to improve aesthetics and function.
When the coronal segment pulp becomes necrotic and there is no radiographic or clinical evidence that the apical segment is irreversibly inflamed or necrotic, the treatment of the coronal segment only is indicated after the root fracture [5]. This procedure was popularized by Frank who emphasized the importance of reducing contamination within the root canal by instrumentation and medication with calcium hydroxide[13]. The beneficial result of root canal treatment with calcium hydroxide was probably because of its antibacterial effect and its ability to promote the formation of a hard-tissue barrier at the canal's apical opening.
The use of calcium hydroxide in teeth with horizontal root fractures was first recommended by Cvek [5]. He proposed that the canal at the level of the fracture line is comparable to the apical foramen of an immature tooth. Thus, he assumed that the repair would be similar to the apexification procedure employed for the tooth with an open apex [5]. The time and the re-filling of the canal with calcium hydroxide that are required to obtain these results may be seen as a drawback.
In the present case calcium hydroxide was used as an intracanal medicament. Several benefits have been proposed when it is used as an intracanal medication during root canal treatment. The one presumed advantage of Ca(OH)2 over other types of medications is its antimicrobial properties attributed to its alkalinity. Several well-controlled studies, both in vivo and in vitro, have shown intracanal reduction of microbial populations, or at least inhibition of bacterial proliferation, both short-term and long-term. It was shown to be superior to camphorated paramono chlorophenol and camphorated phenol in antibacterial activity in a clinical study of 65 single-rooted teeth with periapical lesions (Bystrom et al 1985). When compared with 2% iodine-potassium iodide solution, calcium hydroxide-dressed root canals yielded fewer culture reversals (Safavi et 1985). Ca(OH)2 also alters bacterial cell walls and denatures a potent endotoxin , lipopolysaccharide, thereby rendering it less antigenic [13]. The exact mechanisms are unknown, but the following mechanisms of actions have been proposed [14]:
1. Calcium hydroxide is antibacterial depending on the availability of free hydroxyl ions. It has a very high pH (hydroxyl group) that encourages repair and active calcification. There is an initial degenerative response in the immediate vicinity followed rapidly by a mineralization and ossification response.
2. The alkaline pH of calcium hydroxide neutralizes lactic acid from osteoclasts and prevents dissolution of mineralized components of teeth. This pH also activates alkaline phosphatase that plays an important role in hard tissue formation.
3. Calcium hydroxide denatures proteins found in the root canal and makes them less toxic.
4. Calcium hydroxide activates the calcium-dependent adenosine triphosphatase reaction associated with hard tissue formation.
5. Calcium hydroxide diffuses through dentinal tubules and may communicate with the periodontal ligament space to arrest external root resorption and accelerate healing.
Different treatment modalities in this case were surgical removal of the apical fractured end and orthograde root end filling of the coronal fragment of the fractured root or apexification of the coronal fragment of the fractured end or nonsurgical treatment of the apical end.
The histological reactions at the fracture line are categorized into four types [4]:
(I) Interposition of calcified tissue (callus formation);
(II) Interposition of connective tissue, which is characterized by peripheral rounding of the fracture's ends;
(III) Interposition of bone and connective tissue, radiologically characterized by the clear separation of the two fragments; and
(IV) Interposition of granulation tissue, caused by an infected or necrotic pulp (Andreasen et al. 2007).
Type I is found most commonly in those root-fractured teeth in which the coronal fragment is not or only slightly dislocated. Type II often results after lateral dislocation or extrusion of the coronal fragment. If the trauma occurs before growth of the alveolar process is complete, the coronal fragment continues to erupt, but the apical fragment remains in its pre-trauma position. As a result, bone and connective tissue grow between the two fragments (Type III). In type IV, infected or necrotic pulpal tissue causes an inflammatory reaction in the fracture line (Schroeder 1997, Andreasen et al. 2007). In this case type III healing pattern is seen with the formation of bone and connective tissue in between the fractured ends.
In this case complete obliteration of root canal of apical end was seen on follow up radiographs. In clinical studies of root fractured permanent incisors [15],[16],[17], pulp canal obliteration was found in 69 - 73% of teeth. Pulp canal can be either partial or complete. Both obliteration types progress at the same rate and are normally well advanced after 9-12 months and approach full density 1-2 years later [16]. Obliteration of the apical root canal alone is commonly seen in cases of healing with hard tissue, while obliteration of the apical and coronal aspects of the root canal is often seen in cases with interposition of connective tissue, as well as in teeth with interposition of connective tissue and bone [16]. Therefore, in cases of pulp necrosis while the coronal root canal is usually the only part of the root canal affected, the apical root canal can be completely obliterated[4].
In the present case, the endodontic treatment was considered successful as the following criteria were met: there were absence of clinical symptoms, calcific or scar tissue was present at the fracture line, periradicular radiographic pathosis was reduced in size, no abnormal mobility and sinus tracts was seen.
Conclusion
Mid-root fractures have long been considered to have hopeless prognosis because of poor understanding of the biologic concept of such fracture. After traumatic injury clinical and radiographic follow-up examinations are needed to disclose possible pulpal pathosis. This emphasized that the coronal fragment of the tooth may behave as an independent unit after this type of injury. The treatment of only coronal part can also save the tooth and show good prognosis.
References:
1. J. A. Yates. Root fractures in permanent teeth: a clinical review. IEJ (1992) 25,150-157.
2. Andrea B.Wolner- Hanssen Thomas Von Arx. Permanent teeth with horizontal root fractures after dental trauma. Schweiz Monatsschr Zahmed, vol. 120;3,2010.
3. Cvek M, Mejare I, Andreasen JO. Conservative endodontic treatment of teeth fractured in the middle or apical part of the root. Dent Traumatol 2004; 20: 261-269.
4. Andreasen J O. Traumatic injuries of teeth. Root fracture. 363- 367.
5. Gomes APM et al, Treatment of traumatized permanent incisors with crown and root fractures: a case report. Dent Traumatol 2001; 17: 236-239.
6. Endodontic Therapy - Wein
7. Al-Nazhan S, Andreasen JO, Al-Bawardi S, Al-Rouq S. Evaluation of the effect of delayed management of traumatized permanent teeth. J Endod 1995; 21: 391-3.
8. Andreasen JO, Hjo¨rting-Hansen E. Intraalveolar root fractures. Radiographic and histology study of 50 cases. J Oral Surg 1967; 25: 414-26.
9. Moller A.J.R et al. Influence on periapical tissues of indigenous oral bacteria and necrotic pulp tissue in monkeys. Scandinavian Journal of Dental Research. 1981; 89. 475-84.
10. Deuvanis P.D. & Fan V.S.C. The localisation of blood-borne bacteria in instrumented unfilled and overinstrumented canals. Journal of Endodontics,1984; 10, 52!-524
11. Deivanayagam Kandaswamy, Nagendrababu Venkateshbabu. Root canal irrigants.A review. Journal of Conservative Dentistry, Oct-Dec 2010; Vol 13, Issue 4.
12. Matthias Zehnder. Root Canal Irrigants. JOE, 2006; May: Volume 32, Number 5.
13. B. S. Chong & T. R. Pitt Ford. The role of intracanal medication in root canal treatment. lntermtional Endodontic journal ,1992; 2 5,97-106
14. Shalin Desai and Nicholas Chandler. Calcium Hydroxide-Based Root Canal Sealers: A Review. JOE, April 2009, Vol. 35, Issue 4 , 475-480.
15. Zachrisson BU et al. Long term prognosis of 66 permanent anterior teeth with root fracture. Scand J Dent Rest. 1975, 83;345-54
16. Zachrisson BU et al. repair characteristic of root fracture in permanent anterior teeth. Scand J Dent Rest. 1975, 83;355- 4
17. Anderasen F M et al. Prognosis of root fracture the permanent incisor - prediction of healing modalities. Endod dent trauma. 1989, 5;11-22. |