Introduction
Throughout the last century, the number of cancer cases increased worldwide, now representing one of the most important public health problems in the world. The incidence of oral cancer has also increased.[1] Oral squamous cell carcinoma (OSCC) represents between 90- 95% of all malignant neoplasms of the oral cavity. Lesions are located mainly on the tongue, especially on the lateral posterior border.[2]
Historically, scientific literature has demonstrated a preferential incidence of oral cancers in men aged 50 to 70 years.[2],[3] However, recent epidemiological studies have shown an increase in the development of OSCC in patients under 45 years old.[4] In those cases, tumor behaviour is different and patients have a poor prognosis in comparison to cancer in older adults.[5]
The modification of social and cultural habits, specifically those concerning male and female behaviours, could be related to the increase in the occurrence in women.[1],[6],[7] However, the absence of traditional risk factors such as alcoholism and excessive tobacco use [2] in young patients has suggested that in these cases cancer may be a different disease from that occurring in older patients, and may have a different etiology and clinical progress.[8],[9]
In this article, we report the case of alveolar carcinoma in a sixteen year young female with no history of tobacco or alcohol use, and discuss the clinicopathological findings, etiology and treatment.
Case Summary
A sixteen years young female presented with 2 months history of odynophagia and ulcerated lesion in the oral cavity. There was no history of bleeding from the oral cavity, change in voice and weight loss. She was non-smoker and there was no history of alcoholism or any other harmful habit. Menstrual history of the patient was normal with menarche at 14 years. General physical and systemic examination was normal. Clinically, facial asymmetry with tumefaction at the right side was observed. Local examination revealed two ulcerated lesions in the oral cavity, with irregular borders, and necrotic bed, one was an ulcero-proliferative growth of 5x1 cm size involving lower alveolus, gingiva, gingivo-buccal sulcus posteriorly and another lesion of 3x1 cm size involving the lower alveolus, gingiva, anteriorly on the right side of the oral cavity (Figure: 1). Whitish areas could be observed in the periphery of the ulceration. There was no other lesion seen in the oral cavity. Complete hemogram and routine blood biochemistry of the patient were within normal limits. Mantoux test of the patient was negative. No significant cervical lymphadenopathy was observed. The radiographic examination/ Orthopantogram did not reveal any signs of bone destruction (Figure: 2), and the proposed clinical diagnosis was a traumatic ulcer. Patient underwent incisional biopsy from both the lesions. Areas of great inflammatory infiltrate were identified as well as hornish pearls, intact stratified pavemented epithelium, islets of neoplastic epithelium, polymorphism, and hyperchromatism, thus establishing the diagnosis as well differentiated squamous cell carcinoma with infiltration of the underlying connective tissue and the margins were infiltrated by the tumor (Figure 3A & 3B). The tumor-node-metastasis (TNM) staging system revealed was stage III disease (T3N0M0) based on the mouth cancer TNM classification criteria of the American Joint Committee for Cancer Staging (UICC/AJC). Patient was given external beam radical radiotherapy by conventional fractionation (64Gy / 32fractions / 6.2weeks) by parallel opposed lateral fields to face and neck and patient was disease free for six months and later has lost the follow-up.
 | Figure 1: The intraoral clinical view showing ulcero-proliferative lesion with irregular margins and necrotic bed growth involving the lower alveolus, gingiva, gingivo-buccal sulcus anteriorly and posteriorly with white pseudomembrane in the posterior man
 |
 | Figure 2: The panoramic x-ray examination did not reveal any signs of bone destruction. Additionally, there was a broad area of well and poorly circumscribed radioluency, with no evidence of alveolar crest involvement.
 |
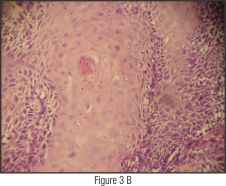 | Figure 3 A & B: Photomicrograph (H&E stain; original magnification ×40) showing unremarkable overlying mucosa and underlying connective tissue with infiltration by tumor.
 |
Discussion
OSCC occurs less frequently in young individuals (<20 years). Those cases represent 3-6% of all OSCCs.[3] In up to 72% of these younger patients; one or more behavioural risk factors are present. Also, men are affected twice as often as women.[10] Of the many different factors associated with an increased risk for OSCC, tobacco and alcohol seem to be the most studied. Individuals who smoke more than 20 cigarettes a day and consume more than 100 g of alcohol a day are at increased risk of oral epithelial dysplasia. Few reports have shown distinct molecular differences between younger and older patients with OSCC, as well as between non-smoking and smoking patients, supporting the hypothesis that different subgroups of OSCC exist, especially with respect to exposure to tobacco carcinogens. [2],[3],[11] It is hypothesised that a subgroup of individuals, characterised by the development of the disease at early ages and by shorter exposure time to behavioural risk factors, develops a histologically similar, but genetically different OSCC, as compared to their older counterparts. This may be due to an increased susceptibility to the development of oral cancer as a result of a lower expression of single nucleotide polymorphisms of the GSTP1 gene. This encodes an enzyme that functions in xenobiotic metabolism of polycyclic aromatic hydrocarbons, which is involved in the metabolism of carcinogens and/or DNA repair, as seen in other tumor types.[3]
Clinical manifestations of OSCC in younger patients have no features to distinguish them from that of older patients; nevertheless, many clinicians tend not to include OSCC as a differential diagnosis in young patients, simply because such disease does not often present in that age range.[2]
The reported case presents different characteristics from the OSCC usually reported in epidemiological studies; the patient was young and without a history of alcoholism or excessive tobacco use. This is consistent with the observation of other workers who report OSCC without a history of alcoholism or excessive tobacco use.[11] Alcoholism or excessive tobacco use have been reported in only a small number of young patients, and even in cases where a correlation is found, the exposure to carcinogens was not sufficient for the development of a malignant lesion.[7] A viral association, particularly the human papilloma virus (HPV), has been implicated in the pathogenesis. The prevalence of HPV, mainly HPV 16, is high in oropharyngeal SCC, but concerning the prevalence of HPV in the oral cavity- mostly tongue SCC as a main location for oral cavity cancer-the data from the literature are not concordant, ranging from 2.6 to 98%. Moreover many people are exposed to such risk factors and only a small percentage develops the disease, which determines the necessity of searching for other risk factors such as immunological or nutritional deficiencies, genetic factors, and microbiological agents in etiogenesis. Among these factors, human papillomavirus and Epstein-Barr virus have already been suggested as etiological factors.[1],[7]
In summary, the factors that should be investigated in order to explain the etiology of OSCC in young female patients, include genetic predisposition, previous viral infections, nutritional patterns, immunodeficiency, occupational exposure to carcinogens, socioeconomic conditions, and oral hygiene.[2] There is some agreement regarding the poor prognosis and short survival rates in younger patients who develop OSCC in the absence of the usual risk factors,[11] although some studies were based on small numbers of patients.[9]
Conclusion
We described the case of a 16-year-young female who was diagnosed to have OSCC of the lower alveolus. There were no known risk factors. OSCC in this age and alveolar site is rare, but should always be considered in the differential diagnosis of non-healing ulcers. The association a young female patient without exposure to the most common risk factors, and more aggressive tumoral behavior in an unusual area, suggest that OSCC, when occurring in non-smokers, represents a different clinical and molecular disease. Further studies would be necessary to identify other risk factors involved in tumoral development in order to improve prevention programmes and early detection.
References
1. Liu L, Kumar SK, Sedghizadeh PP, Jayakar AN, Shuler CF. Oral squamous cell carcinoma incidence by subsite among diverse racial and ethnic populations in California. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 105:470?80.
2. Hirota SK, Migliari DA, Sugaya NN. Oral squamous cell carcinoma in a young patient - case report and literature review. Ann Bras Dermatol 2006; 81:251?4.
3. Tremblay S, dos Reis PP, Bradley G, Galloni NN, Perez-Ordonez B, Freeman J et al. Young patients with oral squamous cell carcinoma. Arch Otolaryngol Head Neck Surg 2006; 132:958?66.
4. Binahmed A, Charles M, Campisi P, Forte V, Carmichael RP, Sándor GK. Primary squamous cell carcinoma of the maxillary alveolus in a 10-year-old girl. J Can Dent Assoc 2007; 73:715?8.
5. Martin-Granizo R, Rodriguez-Campo F, Naval L, Diaz Gonzalez FJ. Squamous cell carcinoma of the oral cavity in patients younger than 40 years. Otolaryngol Head Neck Surg. 1997;117:268?75.
6. Hashibe M, Brennan P, Benhamou S, Castellsague X, Chen C, Curado MP, et al. Alcohol drinking in never users of tobacco, cigarette smoking in never drinkers, and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. J Natl Cancer Inst 2007; 99:777?89.
7. Curado MP, Hashibe M. Recent changes in the epidemiology of head and neck cancer. Curr Opin Oncol 2009; 21:194?200.
8. Hirota SK, Braga FPF, Penha SS, Sugaya NN, Migliari DA. Risk factors for oral squamous cell carcinoma in young and older Brazilian patients: a comparative analysis. Med Oral Patol Oral Cir Bucal 2008; 13:227?31.
9. Popovtzer A, Shpitzer T, Bahar G, Marshak G, Ulanovski D, Feinmesser R. Squamous cell carcinoma of the oral tongue in young patients. Laryngoscope 2004; 114:915?7.
10. Jaber MA. Oral epithelial dysplasia in non-users of tobacco and alcohol: an analysis of clinicopathologic characteristics and treatment outcome. J Oral Sci 2010; 52:13?21.
11. Alsharif MJ, Jiang WA, He S, Zhao Y, Shan Z, Chen X. Gingival squamous cell carcinoma in young patients: report of a case and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107:696?700.
|