Introduction
A proper occlusal scheme is a primary requisite for long-term survival, especially when parafunction or marginal foundations are present. A poor occlusal scheme both increases the magnitude of loads and intensifies mechanical stresses (and strain) at the crest of the bone. Implant Protective Occlusion (IPO) was previously known as medial positioned-lingualized occlusion. This occlusal concept refers to an occlusal plane that is often unique and specifically designed for the restoration of endosteal implant, providing an environment for improved clinical longevity of both implant and prosthesis.
Review Of Literature
J.B. Brunskin and J.A. Hipp in 1984 studied the in vivo forces on dental implants. Methods are presented for measuring vertical force components or bridged titanium dental implants in dog mandibles. These methods have included custom made strain gauge transducers, plus hard wiring and telemetric schemes for data collection. The essential components of the measurements system are described, and typical bite force data are illustrated.
Rangert et al in 1989 carried out a study on the forces and moments on Brenamark implants. The placement of fixture (implants) in relation to the geometry of a prosthetic restoration has a great influence on the mechanical loading of the implant. Based on Theoretic consideration and clinical experiences with the Brenamark system, this article gives simples guidelines for controlling these loads. The emphasis is on design rules that can be used in clinical practice. With the class I lever as a reference. Various clinical implant prosthesis situations are discussed and evaluated.
Parker et al in 1991 reviewed the occlusal considerations in restorative dentistry. The major topics include the assessment and treatment of occlusal wear, the controversies surrounding treatment position of the mandibular condyles, occlusal considerations in osseointegrated prosthesis, the two way relationship between occlusal factors and temporomandibular disorders, design criteria and longevity studies in resin bonded, fixed partial denture.
Hobo et al in 1991 presented a case report on occlusion for osseointegrated prosthesis and concluded that the concept of occlusion suitable for osseointegrated prosthesis is basically the same as the gnathological occlusion. However the natural tooth sinks about 30µm during function, while an osseointegrated bridge which is supporte only by the bone does not sink. Therefore it is necessary to adjust the centric contacts of the osseointegrated fixed bridge slightly more open than the natural teeth. During the eccentric movement, in order to minimize horizontal loading, the concept of disocclusion is generally used.
James et al in 1993 discussed the edentulous implants an emphasized that the occlusal contacts of the final fixed restoration are affected significantly by implant position. Lateral occlusal forces, may lead to abutment screw fracture. They may be due to either excessive lateral occlusal pressure or a malposed implant that requires non axial loading during normal function.
C.E. Misch et al in 1994 discussed an implant protected occlusal on a biomechanical rationale. The clinical success and longevity of endosteal dental implants are controlled, in a large part, by the mechanical milieu within which they function. The occlusion is a critical component of such a mechanical environment.
“Implant protected occlusion” refer to an occlusal scheme that is often uniquely specific to the restoration of endosteal implant prosthesis. Implant orientation and the influence of load direction, the surface area of implants, occlusal table width, and protecting the weakest area are blended together from a biomechanical rationale to provide support for a specific occlusal philosophy.
Tashkandi et al in 1996 did an analysis of strain at selected bone sites of cantilevered implant supported prosthesis. The results revealed that the maximum strain occurred at the strain gauge positioned on cortical bone over the apex of the most distal implant under 10 and 20 lb loading conditions.
Osamu et al in 2002 did a study on influence of supra structure materials on strain around an implant under two loading conditions. The results showed under static and non impact dynamic loading the three super structure materials tested (highly filled composite resin, acrylic resin and gold alloy), had the same influence on the strain transmitted to the bone simulant that surrounded a single implant.
Kent et al in 2004 did a photoelectric analysis of the effect of palatal support on various implant supported overdenture designs and concluded that at the removal of the palatal support produces a greater effect and more concentrated stress difference for maxillary overdenture than difference between the attachment designs.
Steven et al in 2004 did a study of stress transfer of four mandibular implant overdenture cantilevered designs. His results concluded that under load all prosthetic designs demonstrated a low stress transfer to the ipsilateral abutment and to the contralateral side of the arch. The plunger retained prosthesis retained by two implants demonstrated a more uniform stress trasnfer to the ipsilateral terminal abutment than the clip retained prosthesis retained by three implants and provided more retention.
Lucie et al in 2004 did a finite element analysis on the influence of implant length and diameter on stress distribution. Results showed an increase in the implant diameter decreased the maximum stress around the implant neck more than an increase in the implant length, as a result of a more favorable distribution of the simulated masticatory forces applied in this study.
Carlsson GE. in 2009 reviewed literature on various aspects of occlusion related to implant prosthodontics,
The widely spread opinion that implants are superior to natural teeth was refuted by two recent consensus conferences, which concluded that the long-term outcome of implant restorations is not better than that of natural teeth.
Dr. Benito Rilo, José Luis da Silva, María Jesús Mora, Urbano Santana in 2010 also reviewed occlusal contact designs and occlusion strategy guidelines for the main types of implant-borne prostheses.
Occlusal Considerations
Natural Tooth vs. Implant
Classification Of Osseointegrated Prosthesis
Hobo et al
1. Fully bone anchored bridge
2. Overdenture
3. Freestanding bridges
a. Kennedy class I
b. Kennedy class II
c. Kennedy class III
d. Kennedy class IV
4. Bridge connected to the natural teeth.
5. Single tooth replacement.
Misch C.E et al
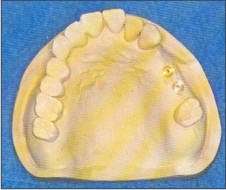
 |
 |
Occlusion For Freestanding Bridges
Kennedy Class I
Clearance of the anterior teeth should be smaller than the natural teeth.
Amount of disocclusion required is same as natural teeth since the anterior guidance is provided by the remaining anterior natural teeth.
Protrusive : 1.1mm
Non working side : 1.0 mm
Working Side: 0.5 mm
 | Fig. 1 - Kennedy Class I
 |
Kennedy Class II
In centric the posterior osseointegrated bridge should have 30 m open contacts, while anterior teeth also should have 30 m open contacts and begin to contact under strong bite pressure.
Amount of disocclusion required is same as natural teeth since the anterior guidance is provided by the remaining anterior natural teeth.
 | Fig. 2 - Kennedy Class II
 |
The disclusion required would be:
Protrusive: 1.1mm
Non working side: 1.0mm
Working side : 0.5 mm
Kennedy Class III
Vertical dimension is maintained by remaining natural teeth
The osseointegrated bridge should contact only under strong pressure.
Amount of disocclusion required is same as natural teeth since the anterior guidance is provided by the remaining anterior natural teeth.
 | Fig. 3 - Kennedy Class III
 |
The amount of disclusion required would be:
Protrusive: 1.1mm
Non working side: 1.0 mm
Working side: 0.5 mm
Kennedy Class IV
To minimize horizontal loads group function occlusion is recommended.
During lateral movement posterior teeth on working side can bear the horizontal load while non working side can be discluded.
Anterior guidance should be flatter than natural dentition to minimize load induced on the fixture during protrusive movement.
Amount of disclussion suggested is as follows:
 | Fig. 4 - Kennedy Class IV
 |
Protrusive: 0.8 mm
Non- working side: 0.4 mm
Working side: 0.0 mm
Overdenture
Recommended occlusion for overdenture is fully balanced occlusion with lingualized occlusion.
Incase maxillary overdenture is opposed by a mandibular fully bone anchored bridge, in centric a small clearance is recommended in the anterior teeth, while posterior contact simultaneously.
Disocclusion is not employed here.
 | Fig. 5 - Overdenture
 |
Crown Contour:
Division A Bone: The most common implant placement corresponds to a central position in the residual ridge. The implant osteotomy begins in the center of the crest and is gradually increased to the optimal width indicated win relation to the recipient bone. As a consequence, whether in the maxilla or the mandible, the implant is frequently placed under the central fossa region of the former natural tooth. (Fig 6).
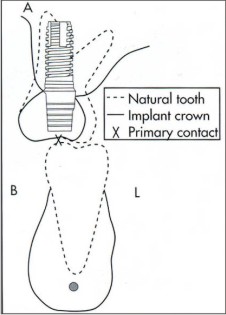 | Fig. 6 - Crown Contour (Div A Bone)
 |
Division B Bone: Division B bone has maxillary and mandibular implants positioned under the lingual cusp when compared with the original natural tooth position. As a result, mandibular crowns require even more reduced buccal contours to avoid offset occlusal contacts. The primary contact of occlusion on an opposing natural posterior maxillary tooth is the lingual cusp, which is reshaped to axially load the implant (Fig 7).
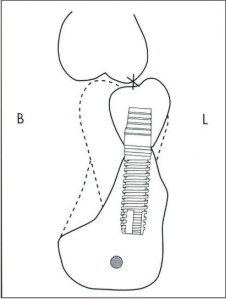 | Fig. 7 - Crown Contour (Div B Bone)
 |
When further resorption occurs and the ridge evolves into Division, C or D, the maxillary palatal cusp becomes the primary contact area, situated directly over the implant body.
Summary
Osseointegrated supported prosthesis (ISP) have shown high standard of success. This success rate depends not only on meticulous surgical protocol but also on understanding concept of occlusion.
Occlusion should be a key factor to overall success rate. The concept of occlusion suitable for implant supported prosthesis is basically the same as gnathological occlusion.
In Centric contact of the Osseo integrated crown or fixed prosthesis should be slightly more open than natural teeth.
In centric Osseo integrated crown or fixed prosthesis should not contact with opposing teeth under the soft bite pressure (to avoid the occlusal load on the I.S.P. which leads overload the bone structure)
Under the strong bite pressure Osseo integrated supported prosthesis should contact after the natural tooth intrudes approximately 30µm.
To avoid overloading of the occlusal surface, the I.S.P. should not have plane-to-plane contact.
Point contact especially cusp-to-fossa tripodal contact is preferred.
During eccentric movement, in order to minimize horizontal movement, the concept of disocclusion is generally recommended.
Anterior segments of the osseointegrated prosthesis should guide the mandible to produce posterior disocclusion.
Canine guided occlusion is not recommended for the Osseo integrated prosthesis to avoid excessive occlusal forces into the single implant fixture which is placed in the canine area. Group function is recommended to distribute the stress over the entire fixture.
The ideal place to bear the horizontal load is the trapezoid area, which is surrounded by the osseointegrated fixtures.
Load transmitted to the fixture is not so destructive when extended mesially in the anterior region, whereas more destructive when extended distally.
Conclusion
The local occlusal considerations in implant dentistry include the transosteal forces, bone biomechanics, basic biomechanics, differences in natural teeth and implants, muscles of mastication and occlusal force, and bone resorption. The incorporation of all these factors lead to an occlusal scheme (IPO) .Occlusal schemes consider the weakest component, full or partial edentulous arches, and posterior or anterior teeth and / or implants. An IPO is a consistent approach for implant occlusal schemes. The material from which the occlusal regions are fabricated may affect implant loading and also affect implant reaction forces to the opposing arch. These occlusal materials also affect wear and fracture, which affects the occlusal contacts, vertical occlusal dimension, and esthetics.
References
1. Misch CE : Progressive bone loading. In Misch CE, editor; Contemporary implant dentistry, pp 623-650, St. Louis, 1993, Mosby.
2. Misch CE : Occlusal considerations for implant supported prostheses. In Misch CE, editior: contemporary implant dentistry, pp 705-733, St. Louis 1993, Mosby.
3. Okeson: Management of Temporomandibular disorders and occlusion, pp 259-260, St. Louis, 1989, Mosby.
4. Ko CC DH, Hollister SJ: Micromechanics of implants /tissue interfaces, J oral implantol 18: 220, 1992.
5. Schupe RJ et al: effects of occlusal guidance on jaw muscles activity, J Prosthet Dent 51:811-818, 1984.
6. Bidez MW, Misch CE : Force transfer in implant dentistry; basic concepts and principles, Oral implant 18: 264-274, 1992.
7. Misch CE: Dentistry of bone and effect on treatment plans, surgical approach, healing and progressive loading. Int. J. Oral implantol 6:23-31, 1990.
8. Chee WWL, Cho GC: A rationale for not connecting implants to natural teeth, J. Prosthod.6 (1):7-10, 1997. |