Introduction
Tooth extraction renders an alveolar ridge that is deficient in bone volume because of the ongoing resorptive process. Sockets heal with the reduction in their dimensions over time. A reduction of 50% in both horizontal and vertical directions has been observed during 12 months , with two-thirds of the reduction occurring in the first 3 months. Reductions were slightly greater in molar than in premolar sites and in the mandible when compared to the maxilla.[1] The remodelling and the modelling of the alveolar process causes a severe resorption of the buccal plate than that of palatal/lingual wall and hence the center of the ridge will move in the palatal / lingual direction. In the extreme case, the entire alveolar process may be lost following tooth loss.[2] The first reported case of immediate implants in the fresh extraction socket had generated increased interest in this technique of implantology.[3] The advantages of immediate implants is multifold including reduction in the number of surgical interventions and the overall treatment time required. Other suggestive advantages include ideal orientation of the implant preservation of the bone at the extraction site and other optimal soft tissue esthetics.[4,5] The surgical criteria for placement of immediate implants involves : atraumatic extraction of teeth in order to preserve the socket walls, alveolar curettage to remove pathologic material , implant should exceed 3-5 mm apically in the host bone to achieve primary stability, greater diameter implant to be placed in the remnant alveolus, subcrestal implantation 1-3 mm dictates good esthetic emergence in anterior zone, excess pressure to be avoided in anterior maxilla, tapered implant should be preferred for an improved bone implant contact ( BIC ) ratio, biomaterials are placed in the circumferential defects > 3-4 mm. Immediate implants prevent undue resorption bound to happen post extraction [4] and allows for maintainence of gingival form & facilitates periimplant gingival tissue esthetics by maintaining the interdental papilla.
Case Description
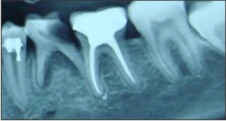
23-year-old female patient presented for routine checkup. Health history of the patient was relatively sound. Intraoral examination of the patient revealed bilateral retained mandibular deciduous molar. Left deciduous molar was carious exposed and right deciduous molar was mobile.(Fig1 a-c) Radiographic assessment revealed absence of 35, 45 and poor prognosis for carious exposed left deciduous molar. With the patients consent treatment planned for the patient included bilateral extraction of the deciduous molars and immediate implants.
 | Fig 1 A
 |
 | Fig 1 B
 |
 | Fig 1 C
 |
Treatment planning
Radiographs revealed a wide interradicular bone in relation of right and left deciduous molars. Treatment was planned to place the implants in the residual interradicular bone in order to for correct angulations. Diagnostic casts were made.
Surgical Stage
After adequate anaesthesia was administered, sulcular incisions are given around the two deciduous molars. Periotome is used to dissect the attached fibers. The tooth is luxated and all effort is made to extract it atraumatically. Following tooth extraction the extraction socket is thoroughly debrIded to remove any remnant tooth fragments. (Fig 2 a-b ).
 | Fig 2 A
 |
 | Fig 2 B
 |
An osteotomy site was prepared with the lindermann drill in the crestal part of the interradicular bone. (Fig 2 c)
 | Fig 2 C
 |
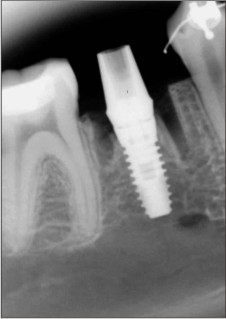
Caution was taken to avoid any slippage of the drill into the socket areas while drilling . The right socket presented an intact interradicular bone measuring 3mm mesiodistally (Fig 2 c), however the left mandibular socket had a very thin septum of interradicular bone which fractured on preparing the osteotomy site. Radiograph was taken with the guidepin to ascertain the depth and angulation of the prepared osteotomy. A threaded parallel walled 4/10.5 mm (Biohorizon, AL) implant was placed in right mandibular extraction socket and 5/10.5 mm (Biohorizon , AL) implant in the left mandibular . (Fig 2 d,f ) The HDD (horizontal defect dimension) around the implant in the left socket was > 3mm. Corticocancellos graft (Mineross, Biohoriozon ,AL) was placed around the implant in this socket. (Fig 2 f) Cover screw was screwed in. Collaplug (Zimmer) was placed over the bone graft and the residual voids around the implant and the surgical site was sutured. Postoperative radiographs were taken. (fig 2 e,g) Postoperative instruction and medication were given. Amoxicillin (Augmentin 675mg thrice a day) was prescribed for 5 days. Sutures were removed after 12 days.
 | Fig 2 D
 |
 | Fig 2 E
 |
 | Fig 2 F
 |
 | Fig 2 G
 |
Prosthetic stage
After the initial healing phase of 4 months, Stage 2 procedure of uncovering the implant was undertaken. Healing abutment (2.5mm, Biohorizon) were screwed in. 2 weeks later , healthy gingival collar was evident.(Fig 2 H, I) Impressions were made with the ball top screws.(Fig 2 J) Cement retained final PFM prosthesis was placed in the right while screw retained prosthesis on the left.(Fig 3 A) Patient was put on the maintainence schedule of 4 months interval and was followed upto 4 years with clinical and radiographic evaluation. (Fig 3 B,C)
 | Fig 2 H
 |
 | Fig 2 I
 |
 | Fig 2 J
 |
 | Fig 3 A
 |
 | Fig 3 B
 |
 | Fig 3 C
 |
Results
Radiographic interpretation reveals a stable periimplant crestal bone on both the sites.
Conclusions
The success of the implant lies in the primary stability as achieved when placed in the ideal restorative position at the time of extraction of the tooth. The reduced surgical visits and the overall treatment time makes immediate implants a treatment of choice over the conventional approach of tooth extraction and waiting upto 4-6 months. The use of grafting materials when used, do provide a conducive environment for soft tissue closure in the fresh extraction socket. However it has been seen that the buccolingual crestal bone changes after immediate & delayed implant placement on usage of bone grafts & guided tissue regenerative membranes, revealed that circumferential defects < 2-3 mm resolve themselves by connective tissue healing rather than GBR principles. [5]
References:
1) Schropp L, Wenzel A, Kostopoulos L, et al. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent 2003;23:313-323
2) Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol 2005;32:212-218.
3) Schwartz AD,Chashu G. The ways and wherefores of immediate placement of implants into fresh extraction sites. A literature review. J Periodontol 1997;68:915-923
4) Lazzara RM. Immediate implant placement into extraction sites. Surgical and restorative advantages. Int J Periodontics Restorative Den 1989;9:333-343.
5) Covani U, Cornelini R,Barone A. Buccolingual bone remodelling around implants placed in immediate extraction sockets. A case series. J Periodontol 2003;742:268-273.
|