Introduction
Desquamative gingivitis is characterized by a diffuse erythema of the marginal and attached gingivae associated with areas of vesiculation, erosion, and desquamation. Desquamative gingivitis is not a disease sui generis but represents a reaction pattern of the gingivae to various stimuli.1 A number of disorders can cause desquamation of the gingiva, many of which are immunologically mediated.(2) Desquamative gingivitis is often associated with mucous membrane pemphigoid, followed by oral lichen planus, and pemphigus vulgaris.2
In such disorders, the gums are especially affected, though lesions may also develop on the inside of the cheeks, the hard and soft palate, tongue, lips and floor of the mouth. Gingival lesions very often precede signs in other parts of the body, and in such situations are referred to as heraldic manifestations.3 Alternatively, they may appear simultaneously with alterations in other locations such as the skin or other mucous membranes such as the conjunctiva, pharynx, larynx, esophagus, vagina and rectum. 4
Such disorders manifest as blisters of variable size ranging from minute vesicles seen as pink to intense red erythematous areas, to actual vesicles (blisters under 5 mm in diameter)
and bullae (blisters over 5 mm in size).5 The blister phase is difficult to detect in the mouth, since trauma and oral mechanical movements quickly rupture the blisters or shed their epithelial covering, leaving bleeding and painful ulcerated areas. The clinical diagnosis may be difficult to establish. In some cases important gingival manifestations are observed as alterations not associated to bacterial dental plaque, while in other situations the presentation may be more insidious - with mild focal erythema refractory to conventional bacterial irritant elimination and control. Paradoxically, periodontal manipulations and prescriptions such as mouthrinses can increase the symptomatology as a result of physical and chemical irritation. As a further source of diagnostic uncertainty, the lesions found in the above mentioned mucocutaneous diseases are initially very similar, and become unrecognizable and impossible to differentiate upon ulcerating. In such situations histological, haematological and immunohistological studies are needed to establish the diagnosis and define an adequate treatment strategy.3
Case Report
A 79 year old female complaining of burning sensation in her mouth since 2 years was referred to the Department of Periodontics, D.A Pandu Memorial R.V. Dental College, Bangalore. On general examination, she was found to have pallor of nail beds and the lower palpebral conjunctiva. Hematological investigation revealed the Hemoglobin percentage (Hb%) to be 10 gm%.
Intraoral examination revealed diffuse edema and spontaneous bleeding of the gingiva. The colour of gingiva was found to be pale pink, except for areas of reddish pink patches in the upper and lower right posterior regions of her mouth. The surface of gingiva was smooth and shiny. Oral hygiene was poor. The gingival contour was altered with rounded margins and a positive Nikolsky's sign was seen. Vesicle formation of the size of about 1 mm in diameter, was seen palatally between 11 and 21. The provisional diagnosis was Pemphigus Vulgaris.
 | Image 1 : Patchy Erythema of the Gingiva
 |
 | Image 2 : Vesicle formation between 11 and 21
 |
 | Image 3 : Positive Nikolsky's Sign
 |
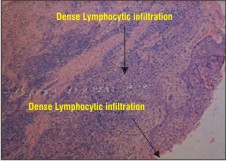 | Image 4 : Microscopic Picture
 |
 | Image 5 : Recall at 6 months
 |
 | Image 6 : Recall at 6 months
 |
The differential diagnosis included:
1) Bullous pemphigoid
2) Mucous membrane pemphigoid
3) Linear IgA disease
4) Lichenoid reaction
5) Plasma Cell Gingivitis
6) Senile atrophic gingivitis
Investigations
A biopsy was taken to include the lesional as well as perilesional tissue from areas of desquamation.
Histopathological Testing revealed a stratified squamous epithelium with ulceration; the underlying stroma showed a dense lymphocytic infiltrate, suggestive of a non -specific inflammatory pathology.
Direct Immnofluorescence testing showed the results to be negative for IgG, IgA, IgM as well as the complement components C1q and C3c.
Due to the lack of specific findings after histopathological and immun of luorescence testing, the diagnosis of non specific vesiculo-bullous lesion was made.
The patient was managed using conventional treatment. Scaling and root planing was performed.
Topical steroids were prescribed. The patient was instructed to apply 0.1 % Triamcinolone oral paste (Kenacort), a synthetic topical corticosteroid, on the affected areas p.c. and h.s. The clinical signs and symptoms were found to be diminished at 1 week recall. The patients is being followed up at regular recall intervals for periodontal maintenance and showed no recurrence of the lesions at 2 weeks, 3 months and 6 months recall.
Discussion
Epithelial cell-cell and cell-matrix adhesions are maintained by anchoring junctions which function by connecting the cytoskeletal elements of a cell either to those of another cell or to the extracellular matrix. The anchoring junctions are, in principle, built up by intracellular attachment proteins which connect specific elements of the cytoskeleton to transmembrane glycoproteins whose extracellular domains interact either with adjacent plasma membrane proteins or with proteins in the extracellular matrix.6 Immune mediated processes modify the biology of epithelial and sub-epithelial areas . The action of circulating auto-antibodies causes damage to the basement membrane, dysfunction of epithelial cell-cell and cell-basement membrane adhesion systems, and formation of vesicles and bullae.2 Bullous lesions of the skin and oral mucosa were traditionally classified according to their clinical and histological patterns 7. In the '60s and '70s, it was demonstrated that several of these conditions were autoimmune diseases, and the autoantigen localization was described by immunohistology.7,8 Patients' autoantibodies were classified according to immunoglobulin class and complement binding capacity and were proven to be critical to the disease process. Traditionally, vesiculo-erosive disorders causing desquamative gingivitis have been divided into 2 types according to the location of splitting under light microscopy, which also corresponds to the location of immune-mediated attack:
i) intraepithelial eg. Pemphigus vulgaris
ii) subepithelial eg.mucous membrane pemphigoid, bullous oral lichen planus,linear IgA disease, erythema multiforme.2
In the present case, the provisional diagnosis of Pemphigus vulgaris had been given due to presence of the classical Nikolsky's sign along with vesicle formation. However, histopathology and immunofluorescence could not detect any specific antibodies / immune complexes or the specific area of immune attack. Therefore, the final diagnosis of non-specific vesiculo-bullous lesion was given.
The condition was expressed in the oral cavity as desquamative gingivitis. There is no evidence that desquamative gingivitis per se can cause loss of attachment and alveolar bone destruction.2 There is only little systematic information about the impact and the potential influence of desquamative gingivitis on the onset and / or progression of plaque-related periodontitis.
It has been suggested that desquamative gingivitis lesions may indirectly increase the long-term risk for plaque-induced periodontal disease via plaque accumulation when symptoms associated with such lesions impede proper oral hygiene.2,9 Hence, in the present case, emphasis was laid upon establishment of proper plaque control in addition to prescription of topical steroids. Moreover, it has also been suggested by JC Leao 10 that although desquamative gingivitis is usually unrelated to local plaque accumulation, it could aggravate the disease condition. It is likely that the resolution of chronic inflammation including periodontal lesions further contributes to the improvement of desquamative gingivitis. Hence plaque control was stressed upon in this patient.
In addition, 0.1% Triamcinolone oral paste (Kenacort) was prescribed to be applied on the affected areas after food and before bedtime. At 1 week recall, the vesicles had disappeared and the gingival condition showed significant improvement. The patient was followed up at regular visits scheduled for maintenance therapy. No recurrence was observed at 2 weeks, 3 months and 6 months recall.
Conclusion
A case of vesiculo-bullous lesion is presented, in which the specific diagnosis could not be confirmed by histopathological examination or immunofluorescence. Patient was managed symptomatically. The clinical signs and symptoms are under control.
References
1) Journal of American Academy of Dermatology 1982 Dec;7(6):729-35. Desquamative gingivitis: clinical, histopathologic, immunopathologic, and therapeutic observations. Rogers RS 3rd, Sheridan PJ, Nightingale SH.
2) JOP 2008 Jan;79(1):4-24. Diagnostic pathways and clinical significance of desquamative gingivitis. Lo Russo L, Fedele S, Guiglia R, Ciavarella D, Lo Muzio L, Gallo P, Di Liberto C, Campisi G.
3) Medicina Oral 2002; 7: 271-83. Gingival disorders of immune origin. José Luis Castellanos Suárez.
4) Castellanos JL, Diaz GL, Gay ZO, eds. Medicina en odontología.Second edition. México: El Manual Moderno; 2002, Chapter 11 (in press).
5) Sapp JP, Eversole LR, Wysoky GP, eds. Patología oral y maxillofacial contemporánea. Madrid: Harcourt Editores, 1998. p. 244-76.
6) Alberts B, Bray D, Lewis J, Raff M, Roberts K, Watson JD (1994). Molecular biology of the cell. New York, NY: Garland Publishing Inc.
7) Lever WF (1979). Pemphigus and pemphigoid. Am Acad Dermatol 1:2-31.
8) Bean SF, Rogers RS, Jordon RE, Furey NL, Michel B (1979). Cicatricial pemphigoid. In: Immunopathology of the skin. Beutner EH, Chorzelski TP, Bean SF, editors. New York: John Wiley & Sons, pp. 257-263.
9) Oral Diseases (2010) 16, 102-107.Effect of desquamative gingivitis on periodontal status:a pilot study. L Lo Russo1, R Guiglia, G Pizzo, G Fierro, D Ciavarella, L Lo Muzio, G Campisi.
10) Oral Diseases (2008) Vol 14, Issue 6, 556-560 Desquamative gingivitis: retrospective analysis of disease associations of a large cohort .JC Leao , M Ingafou, A Khan, C Scully, S Porter. |