Introduction
Planning and performing full mouth rehabilitation is probably one of the most demanding tasks faced by a prosthodontist. Full mouth rehabilitation entails the performance of all the procedures necessary to produce healthy, esthetic, well functioning, and self-maintaining masticatory mechanism.
Increasing the vertical dimension of occlusion (VDO) is often held to be a hazardous procedure in prosthetic treatment.1-3 But the modern practice of renewing and reorganizing the teeth by prostheses began with the idea of “raising the bite” to rectify closure resulting from excessive wear of the occlusal surfaces. A moderate increase in the vertical dimension of occlusion does not seem to be a hazardous procedure, provided that occlusal stability is established4 which by improving the relationship of the teeth improves the condition and health of the supporting structures. With our present understanding of traumatic occlusion and its deleterious effect upon the supporting structures, the procedure known as “bite raising” has shifted in emphasis and broadened in scope and is now designated by a term that describes it accurately.
It is not always practical, however to restore a worn occlusion without some increase in vertical dimension. If the vertical dimension (VD) needs to be increased, then it will be only to provide necessary room for the restorative materials & would rarely exceed 1.5 to 2 mm.5 Even then, the dentist should be aware of the potential problems that might result, mainly instability following the restorative increase in vertical dimension. The rationales for altering VD include aesthetic, correcting occlusal relationship & allowing space for restorations for prosthetic convenience.5
In the present case the bite was collapsed due to loss of numerous posterior teeth, & attrition of lower anterior teeth, together leading to loss of vertical dimension. The task of rehabilitating this patient includes the restoration of missing & attrited teeth, by increasing the VD. Here in this report, discussion of treatment plan has been elaborated, with procedural steps for full mouth rehabilitation of dentition with increased VDO according to Pankey Mann Schuyler Philosophy.
Case report
General & Dental History And Examination
A 42-year-old man was reported to department of Prosthodontics , KVG Dental College Sullia(D.K) with complaints of unpleasant smile, difficulty in chewing, and wants the replacement of his missing teeth. The medical history was non-contributory, except hypertension for which he was undergoing treatment.
The dental history revealed partially edentulous condition in upper & lower back teeth region since 8-10 years and had under-went some restorative treatment, but was not satisfied. The intraoral examination revealed missing maxillary right & left 2nd molars, and right 1st premolar. In mandible right & left 1st molar and left 2nd premolar were missing. There was severe attrition of lower anteriors with incisors attrited till gingival 1/3, resulting in severe anterior deep bite [Fig:1]. There was no history of bruxism. Retained posterior teeth were supra-erupted in the opposing edentulous spaces. And hence the entire occlusion was hampered with lot of occlusal interferences in centric & eccentric contact relationship, favouring attrition of teeth which had resulted in collapsed bite.6
 | Figure-1: Pre-treatment mutilated dentition with missing teeth & anterior deep bite.
 |
Anatomic differences due to worn anterior & posterior teeth must be managed differently by assessing the periodontal endodontic & coronal tooth tissue & the occlusal relationship which are necessary for a comprehensive treatment plan for worn posterior teeth.7 On examining individual tooth, upper left 2nd molar was RCT treated about 5 years back. There was heavy overhanging amalgam restoration, inflammed periodontium with gingival recession & bifurcation involvement of the root [Fig:2]. Lower right second premolar was post & core treated, with the core fractured & dislodged but the post was firm & intact. There were also the attrition & abrasion of upper anteriors [Fig:3].
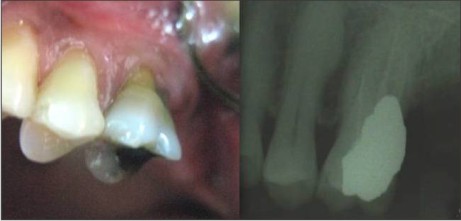 | Figure-2: RCT treated upper left 2nd molar with gingival recession & bifurcation involvement of the root, & heavy overhanging amalgam restoration.
 |
 | Figure-3: Post & core treated lower right second premolar with intact post but core fractured & dislodged.
 |
The Definitive Treatment Plan
Tentative jaw relation was recorded, by using face-bow (Teledyne Water Pik, Fort Collins, Colorado, USA) & centric records & then mounting was done on Hanau Wide Vue semi-adjustable Articulator (No 183, Teledyne Water Pik, Fort Collins, Colorado, USA). Based on amount of freeway space and for convenience of restoration, vertical dimension of occlusion was raised by 2mm on the articulator itself, & an anterior jig with this increased VD was fabricated. Occclusal plane was determined by Broadrick's flag analysis.8 Wax-up of diagnostic casts with increase VDO was done and an occlusal template was fabricated with self cure acrylic resin. Patient was allowed to wear this template for a period of two months according to standard protocol, and no relevant signs and symptoms reported during this period.
It was planned to restore upper distal extension edentulous space with cast partial denture, lower right and left missing posterior teeth with porcelain fused to metal restorations & attrited lower incisors with metal ceramic restorations with increased VDO. Mean while upper left first molar was endodontically & periodontically evaluated and was treated for overhanging restoration, followed by curretage & root planning. Later this tooth was restored with full metal crown extending to include the bifurcation, & with provision for occlusal rest seat for Cast partial denture(CPD). However in lower 2nd premolar, endodontic post was in good condition & the fractured core was built with composite and was included as abutment for 4 units Fixed partial denture(FPD) along with other abutment teeth.
With this treatment plan rehabilitation was done with PMS Philosophy, where in restoration of lower anterior dentition was done first, then upper anteriors followed by lower posterior and at last upper posteriors.3 Lower canines were minimally abraded, so they were restored with composites. As the clinical crown height of Lower incisors teeth were very less & VDO has been raised, preparation of these teeth was done with minimal occlusal reduction.9 Temporaries were fabricated according to diagnostic wax-up with proper anterior guidance during protrusion & unilateral group function during lateral excursions and were cemented, which was later replaced with bridge fabricated with porcelain fused to metal (PFM) restorations. The abraded and attrited upper anteriors were then restored with composites. Until posterior teeth rehabilitation was not completed, the anterior part of bite raising template was cut off and patient was asked to wear the same. Then lower posterior teeth rehabilitation was done. Teeth preparation was done, metal try-in completed and then final restorations were cemented[Fig:4]. Mouth preparation was done for cast partial denture preparation, impression made and routine clinical and lab-procedures were followed for the fabrication of it. Finally fit-in of removable cast partial prosthesis was done [Fig:5]. After two months of recall check up patient was completely satisfied with the prosthesis.
 | Figure-4: Rehabilitation of upper anteriors with composites & lower anterior posterior dentition with FPDs.
 |
 | Figure-5: Final fit-in of Removable Cast Partial Prosthesis on cast as well as intraoral.
 |
Discussion
The most common reason for full mouth rehabilitation is to maintain the health of periodontal tissues with many more reason including TMJ problems. The decision to carry-out any treatment in full mouth rehabilitation should be based upon achieving oral health, function, esthetics and comfort, hence should be planned around these rather than the technical possibilities.10
The present treatment for illustrated case was to; replace missing teeth, & to regain VD to treat wear and enhance esthetics with little cosmetic dentistry. The functional stable posterior occlusion exists when enough teeth are in simultaneous even contact.11 In our present case to reorganise the occlusion & achieve stable results in increased VDO, Occlusal Splint therapy was recommended which provides muscle relaxation & condyles in centric position. Discrepancy in centric contacts of occlusion was eliminated using provisional restorations and temporary partial dentures to restore the VDO. Hence the final restorations were in stable maxillo-mandibular relationship.
Conclusion
The basic principles in restoring attrited anterior & posterior with endodontic & periodontic complications have been discussed, highlighting the necessary steps for full mouth rehabilitation which was done with Pankey Mann Schuyler philosophy. However there are number of approaches to rehabilitate a mutilated dentition but achieving a stable occlusal relationship even after raising the VDO is paramount for which proper treatment plan including appropriate occlusal philosophies that apply necessary sequential steps for the rehabilitation is the must to achieve the expected treatment results.
References
1. Brecker C. Clinical Procedures in Occlusal Rehabilitation. St. Louis, 1966. The C.V Mosby Co., pp 203-205, 376.
2. Smith BH. Changes in occlusal face height with removable partial prostheses. J Prosthet Dent 1975;34:278-83.
3. Dawson PE. Evaluation Diagnosis and Treatment of Occlusal Problems. St. Louis. 1974, The C. V. Mosby Co., pp 275-285.Brill N. Adaptation of Hybrid-prosthesis; J Prosthet Dent. 1955 Nov;5(6):811-24.
4. Carlson GE, Ingervall B, Kocak G. Effect of increasing vertical dimension on the masticatory system in subjects with natural teeth. J Prosthet Dent 1979; 41:284-9.
5. Bloom DR, Padayachy JN. Increasing occlusal vertical dimension - Why, when & how.British Dental Journal 2006;200:251-6.] Eckert SE, Carr AB. Single maxillary complete denture. Dent Clin North Am. 2004;48:567-83.
6. Friedrick CSC, Hak KY, Philip RHN, Tak WC, Roger JS. Restorative Management of the Worn Dentition:1. Aetiology & Diagnosis. Dent Update 2002; 29:162-8.
7. Friedrick CSC, Michael GB, Philip RHN, Tak WC, Roger JS. Restorative Management of the Worn Dentition:3. Localized Posterior Toothwear. Dent Update 2002; 29:267-72.
8. Craddok HL, Lynch CD, Franklin P, Youngson CC, Manogue M. A study of the proximity of the Broadrick ideal occlusal curve to the existing occlusal curve in dentate patients. Journal of Oral Rehabilitation. 2005 Dec;32(12):895-900.
9. Wassel RW, Steele JG Welsh G. Considerations when planning occlusal rehabilitation: A review of the literature. International Dental Journal 1998; 48:571-81.
10. Friedrick CSC, Adam SCS, Philip RHN, Tak WC, Roger JS. Restorative Management of the Worn Dentition:2. Localized Anterior Toothwear. Dent Update 2002; 29:214-22.
11. McCullock AJ. Making Occlusion Work:2. Practical Considerations. Dent Update 2003; 30:211-19. |