Introduction:
Root resection is the procedure by which one or more of the roots of a tooth are removed at the level of the furcations while leaving the crown and remaining roots in function.1 Farrar2 introduced this root resection procedure, which has been used to treat class II and III furcation involved molars. Proper tooth selection is important for the success of the procedure. The ideal tooth is one with well developed long roots that have adequate divergence and a narrow root trunk. The furcations area should have a good deal of remaining bone, and the remaining roots should have adequate support and a favorable crown to root ratio.
The endodontic-periodontic lesion presents challenge to the clinicians as far as diagnosis and prognosis of involved teeth are concerned. Proper diagnosis of the lesion is essential for appropriate treatment. When endodontic infection drains through the periodontal ligament, a typical narrow and deep probing site can be detected.
Classification of Endodontic-Periodontic Lesions.3
1. Primary Endodontic
2. Primary Periodontic
3. Primary Endo Secondary Periodontic
4. Primary Periodontic Secondary Endodontic
5. True Combined
Root resection is one of the treatment modality in cases of periodontic-endodontic lesion especially when molars are involved. Root resection may be carried out as vital or nonvital procedures. If vital sectioning is employed provision for final endodontic therapy should be made, and in cases of non-vital root resection endodontic therapy should be done prior to surgery.
The prognosis of root resection has been well-documented. Some investigators4,5 reported that root-resected molars had >90% survival rate, whereas other investigators6,7 reported that 30% of resected molars failed over a 10-year period.
Indications for root resection are:
1) Grade III lesions. Inability to maintain furcations.
2) Severe gingival recession on a single root.
3) Close root proximity with minimal interseptal bone (commonly seen between the maxillary first and second molars).
4) Root resorption.
5) Root perforation.
6) Severe vertical bone loss about one or more roots.
7) Inability to achieve predictable regeneration.
Case Report:
A 32 year old male patient reported to the Department of Periodontology, M.G.V Dental College and Hospital, Nashik with the chief compliant of food lodgment and pain in the upper and lower right posterior region. Clinical examination revealed deep periodontal pocket in between 16 and 17 (7mm) and between 46 and 47 (9mm). Recession of 3mm present with 16 and 17 (Figure. 1). Grade III furcation involvement was observed with 16,17 and 46. Grade I mobility was present with 17 while no mobility was detected with 16 and 46. Radiographic examination revealed severe bone loss with respect to the distobuccal root of 16, mesiobuccal root of 17 (Figure. 2) and distal root of 46 (Figure.3). Radiolucency in the furcation area suggested furcation involvement. Vitality test showed positive response with 16 and 17 and negative response with 46.
 | (Figure. 1) Pre operative photograph showing gingival recession with 16, 17 and periodontal abscess with 46.
 |
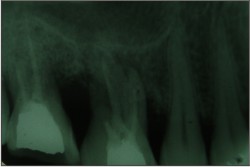 | (Figure. 2) Pre operative radiograph showing severe bone loss distal to 16 and mesial to 17.
 |
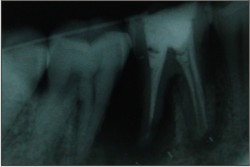 | (Figure. 3) Pre operative radiograph showing severe bone loss distal to 46.
 |
After initial periodontal therapy non-vital root resection was planned with the respective teeth. Roots to be resected were ditobuccal root of 16, mesiobuccal root of 27 and distal root of 46. Root canal treatment was done with the respected teeth. Two weeks after root canal treatment periodontal flap surgery was performed to gain access for the root resection. High speed diamond burs were used to resect the root at the level of furcation (Figure 4 and 5). After resection, overhangs of the crowns were removed and gradual smoothening was done. Patient was evaluated for one month after surgery and it showed uneventful healing of the respected area (Figure 6, 7 and 8). Special instruction was given to the patient for the oral hygiene maintenance by the use of interproximal brush.
 | (Figure. 4) Flap reflection and root resection done. (distobuccal of 16 and mesiobuccal of 17)
 |
 | (Figure. 5) Flap reflection and root resection done. (distobuccal of 46)
 |
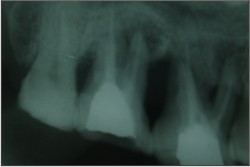 | (Figure. 6) Radiograph of 16,17, one month after root resection.
 |
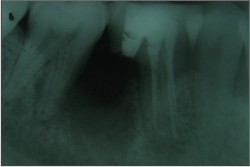 | (Figure. 7) Radiograph of 46, one month after root resection.
 |
 | (Figure. 8) One month post operative photograph with uneventful healing.
 |
Discussion:
The reported case was of endo-perio lesion associated with 16,17 and 47. Establishing the original cause of an endo-perio lesion is not usually straightforward. Serial radiographs and the state of the pulp on first entering the root canal system can provide useful clues. For example, the presence of a vital (bleeding) pulp in a tooth associated with serial radiographs, which showed progressive periodontal disease, would suggest a periodontal origin to the endo-perio lesion. In this case serial radiographs were not available but bleeding from the pulp at the time of root canal therapy indicated vital pulp which suggests secondary endodontic involvement. Root resection was planned with the involved teeth.
Root-resection therapy is a treatment option for molars with periodontal, endodontic, restorative, or prosthetic problems. Because root resection is very technique sensitive and complex, proper case selection is essential.8 The prognosis of root resection has been well-documented in previous studies.4,9,10 According to the standardized reports on root resection of Buhler11, 89% of root-resected teeth survived over a 7-year period. However, Carnevale et al.5 reported a 6.9% failure rate over a 10-year period, which was lower than this study. In a limited meta-analysis using common denominators of time of observation and criteria of failure as defined by Langer et al, Buhler12 reported that the failure rate for teeth treated by root-resection, over a seven-year observation period, was 11%.
The survival rate of resected molars might be influenced by a variety of factors. Lang and Tonetti13 suggested that an evaluation of the risk factors for periodontal disease progression was required at the patient, tooth, and site level. Molars that underwent root resection because of periodontal problems had a higher survival rate than those resected because of non-periodontal problems. Root-resection therapy for molars with periodontal problems was based on the periodontal pathology and could obtain a good prognosis.
Conclusion:
Root-resection therapy is still a valid treatment option for molars with furcation involvement and severe bone loss. Root resection should be considered as another weapon in the arsenal of the dental surgeon, determined to retain and not to remove the natural teeth. Root resection to treat periodontal problems showed a better prognosis than root resection performed for non periodontal purposes. In addition, a careful prosthetic plan should be designed to avoid a fracture of resected molars related to biomechanic impairment.
References:
1. American Academy of Periodontology. Glossary of Periodontal Terms. Chicago: American Academy of Periodontology; 2001:45.
2. Farrar JM. Radical and heroic treatment of alveolar abscess by amputation of roots of teeth. Dental Cosmos 1884;26:79.
3. Simon J.H.S., Glick, D.H., and Frank, A.L. The relationship of edodontic- periodontic leaions. J Periodontol. 1972;43:202-208.
4. Carnevale G, Di Febo G, Tonelli MP, Mann C, Fuzzi M. A retrospective analysis of the periodontal-prosthetic treatment of molars with interradicular lesions. Int J Periodontics Restorative Dent 1991;11:189-205.
5. Camevale G, Pontoriero R, di Febo G. Long-term effects of root-resective therapy in furcation-involved molars. A 10-year longitudinal study. J Clin Periodontol 1998;25:209-214.
6. Langer B, Stein SD, Wagenberg B. An evaluation of root resections. A ten-year study. J Periodontol 1981; 52:719-722.
7. Blomlof L, Jansson L, Appeigren R, Ehnevid H, Lindskog S. Prognosis and mortality of root-resected molars. Int J Periodontics Restorative Dent 1997;17:190-201.
8. DeSanctis M, Murphy KG. The role of resective periodontal surgery in the treatment of furcation defects. Periodontol 2000. 2000;22: 154-168.
9. Minsk L, Poison AM. The role of root resection in the age of dental implants. Compend Contin Educ Dent 2006;27: 384-388.
10. Hamp SE, Myman S, Lindhe J. Periodontal treatment of multirooted teeth. Results after 5 years. J Clin Penodontol 1975:2:126-135.
11. Buhler H. Survival rates of hemisected teeth: An attempt to compare them with survival rates of alloplastic implants. Int J Periodontics Restorative Dent 1994;14:536-543.
12. Buhler H (1988) Evaluation of root-resected teeth. Results after 10 years. J Periodontol 1988;14:537-543.
13. Lang NP, Tonetti MS Peslodontal diagnosis in treated periodontitis. Why, when and how to use dmical par ameters. J CIin Periodontol 1996;23:240-250. |