Introduction
The development of light activated composite materials in 1970s heralded a period of rapid progress in the field of tooth colored restorations.3 Now a days, there is an increasing demand for aesthetic restorative dentistry, using primarily direct or indirect composites3. Successful use of these products depends directly on correct functioning of the visible light curing unit1. Light-cured resin composites rely on sufficient intensity of light to achieve adequate polymerization The impact of the sufficient intensity output of curing lights in ensuring the longevity of restorations and avoiding undesirable clinical outcomes is universally accepted.6 Most often, dentists blame material for the failure of restoration rather than the technique or method of placement of restoration. Light emitting diode (LED) lights have attracted interest and are becoming increasingly popular among dentists in comparison to laser and Plasma Arc Curing lights.6
Adequate polymerization is a crucial factor in obtaining optimal physical properties and clinical performance of resin composite restorative materials.8 Three essential components are required for adequate polymerization: sufficient radiant intensity, correct wavelength of visible light and ample curing time. Other factors influencingthe adequacy of polymerisation includes the type of composite resin, shade, translucency, thickness of the increment, distance of the light tip from the surface of the material.1
Although no acceptable single minimum value of intensity has been validated scientifically, light units with intensities of less than 300 mW/cm2are described in the literature as inadequate.4 As the curing light ages, the light output diminishes due to deterioration of the components. In addition, numerous factors are capable of interfering with efficient functioning of the curing unit. Diminished light output can affect the physical properties of the filling: incomplete resin polymerisation increases microleakage around resin composite thereby, decreases the integrity ofadhesion, leading to oral fuids and bacterial penetration. The resultant percolation will lead to a recurrence of caries.7 Recently, a number of light intensity meters (curing radiometers) have been marketed for dental use. Manufacturers of some dental radiometers imply a direct relationship between intensity readings and depth of cure.
Materials And Method
Materials
Radiometer (Confident Manufacturing Products) was used in this study. It had a detector at the centre and filter placed inside that helps in recording the intensity.
Method
One hundred light curing units in dental offices were examined for their output intensity. Collection of related information and measurement of the intensity was recorded by operators. Consent of the dentist was obtained in order to examine the light curing unit in the operatory.
The tip of the unit was cleaned before examination. When a quartz tungsten halogen (QTH) unit was examined for the output intensity, the unit was activated for three consecutive 60sec intervals interrupted by 1sec of off time to reduce the cool bulb variable. When a light emitting diode (LED) unit was examined, three readings were taken and the average values were obtained. The curing units were divided into two categories: QTH and LED. The parameters examined were:
1. Output intensity of the light curing unit
2. Monitoring of output intensity
3. Frequency of bulb replacement
The output intensity (mW/cm2) of all the examined lights were categorized into three groups:
1. < 300 mW/cm 2
2. In between 301-400 mW/cm 2
3. > 401mW/cm 2
Results
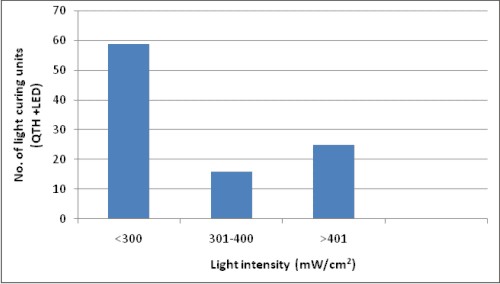
Among the 100 curing units examined, 31 were LED units and 69 were QTH units and most of the units examined by the operators had intensities ranging between 200 mW/cm 2 and 300 mW/cm 2. It was observed that the QTH units in which the bulb was changed once or twice, the recorded intensity was higher than to those in which the bulbs were not changed even once.59% (7% LED + 52% QTH )of the units were found to be faulty as shown in Table 1.
 |
 |
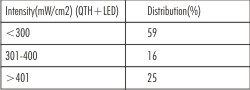 | Table 1. Distribution Of The Light Intensity Recording
 |
Discussion
Light-activated composite materials polymerize by free radical polymerization when exposed to light of adequate intensity and at wavelengths in the 400 to 500 nm range. Camphoroquinone (CQ) which is a commonly used photoinitiator absorbs energyand in combination with amine produces free radicals to begin the polymerization process. Macroscopically, the dental composite hardens, typically after light exposure times ranging from 20 s to 60 s.
Irradiance is an important factor to be pointed out because it represents the number of photons delivered to the sample per unit of time, regardless the area illuminated. Light intensities may vary significantly even among different units supplied from the same manufacturer. Duringpolymerization, light passes through anincrement of the material in which it isabsorbed and scattered; consequently, its intensity decreases. This maycause deeper layers of an increment notto polymerize sufficiently, resulting ina low monomer-polymer conversion rate which causes inferior physical properties, more water absorption, microleakage,postoperative sensitivity and discoloration of the resin composite. Thus, both the degree of cure on the surface closest to the light source and depth of cure have been shown to be affected by the intensity of the light curing units.3 Therefore, the performance of thelight cure unit remains one important factor in determiningadequate polymerization for optimal clinical results.
Nowadays, a number of sources for photo-initiating composite resins are available: halogen lamps, plasma arc lamps, laser and light-emitting diode (LED) lights. The most commonly used are halogen and LED lamps.
QTH light curing units are most widely used by the dentists worldwide. The main reason behind this is the low cost of QTH units as compared to plasma Arc curing unit or lasers. QTH lamps have a limited lifespan of 100 hours with consecutive degradation of bulb caused by considerable quantity of heat being produced during operating cycles. This implicates a reduction of curing efficiency overtime by aging of the components.9
As compared to QTH, LED consumes less energy and does not require external cooling. Moreover, LED lamps have a lifetime of several 1000s of hours without a significant intensity loss.9
A recommended minimum intensity of 300mW cm-2 has been suggested for curing a 2-3-mm increment of composite12. Hence, a minimum of 300 mW cm-2 was selected as an adequate intensity for this study.
This study found that 59% of the units had inadequate intensities.17% of the units in this study recorded levels of light output in the marginal range (250- 300 mW/cm2). Barghi et al recorded 30% of units with intensities of less than 200 mW cm-2, a level which they could not recommend for clinical use6.In another study conducted by Hegde et al, 51% of light curing units had intensities less than 200mW/cm2.6
Nearly one-half of the dental practitioners surveyed had never checked the intensity of their light curing units. Of the 19% who had checked their units in the previous 6 months, two practitioners checked their units weekly, the remainder less frequently.The present study showed a significant reduction in light intensity with older units. Friedman showed that the lamp degrades gradually with time.11 Caughman et al reported that majority of new units initially possessed an adequate intensity to polymerize composite resin to a thickness of 2mm.10
A relationship was found between replacement of the bulb and adequacy of light intensity. All but one of the 42 light curing units that recorded an inadequate intensity had never replaced their bulbs, and was reportedly replaced only when they failed completely. Many practitioners incorrectly assume that the halogen bulbs used in visible light curing units produce a consistent output until the bulb burns out or fails to produce blue light1.
Dentists are unable to determine the adequacyof light intensity by looking at the light emittedfrom a light polymerization unit.In addition, assessing the hardness of the surface of a polymerizedresin-based composite increment with anexplorer is also not a reliable method for testing theeffectiveness of the light sourceThis is due to the fact that a light unit withinferior light intensity was shown to be able toharden the surface of a resin-based compositeincrement just as well as a light unit with superiorlight intensity. However, the subsurfacelayer of a resin-based composite increment isaffected most by inferior light intensity.Light curing units should therefore be monitored regularly to ensure adequate light output. When this diminishes, the components, particularly the bulb andfilter, should be checked for deterioration and possible replacement.
Knoop hardness and infra-red spectroscopy tests, which determine the percentage of carbon double-bond conversion during polymerisation, have been found to be more accurate in measuring light intensity. But it has been suggested that radiometers are more accessible and less expensive to the general practitioner as compared to the above mentioned tests.2 Numerous authors have demonstratedthe usefulness of the radiometer as a tool for measuring light output from visible light curing units. It has been recommended that new or repaired units should be tested to ensure adequate light intensity. The units should be monitored periodically, with the initial reading providing a useful baseline for detecting changes in light intensity that occur with ageing.
Conclusions
A survey of the efficiency of light output from 100 visible light curing units in Punjab dental practices revealed that:
1. Approximately 59% had a light output of less than 300 mW cm-2, an intensity that has been reported as inadequate to cure a 2-mm thick increment of composite resin.
2. An additional 16% of the light curing units registered an output of between 301 and 400mW cm-2which is considered as an adequate intensity.
3. 25 % of the light curing units registered an output of more than 400 mW cm-2
4. There is general lack of awareness among dentists of the need of maintenance of these units.
Finally to conclude, further studies can still be performed on the influence of length and diameter of the curing tip, the effect of direct current supply or battery- supported systems on the intensity of curing light, and the use of different radiometer to measure intensity for same machine.
References
1. Martin FE. A survey of the efficiency of visible light curing units. Journal of Dentistry1998; 26(3):239-243.
2. Pilo R, Oelgiesser D, Cardash HS. A survey of output intensity and potential for depth of cure among light-curing units in clinical use. Journal of Dentistry1999; 27 :235-241.
3. Shortall AC, Harrington E and Wilson HJ. Light curing unit effectiveness assessed by dental radiometers. Journal of Dentistry1995:23( 4):221-232.
4. Fan PL, Schumacher RM,Azzolin K, Geary R,Eichmiller FC. Curing-light intensity and depth of cure of resin-based composites tested according to international standards.J Am Dent Assoc.2002; 133:429-434.
5. Barghi N, Berry T, Hatton C. Evaluating intensity output of curing lights in private dental offices. J Am Dent Assoc 1994; 125: 992-996.
6. Hedge V, Jadhav S, Aher GB. A clinical survey of the output intensity of 200 light curing units in dental offices across Maharashtra. J Conserv Dent 2009;12(3):105-108.
7. Tielemans M ,Compere P, Geerts SO, Lamy M, Limme M, Moor RJG, DelmeKIM, Bertrand MF, Rompen E, NammourS.Comparison of microleakages of photo-cured composites using three different light sources: halogen lamp, LED and argon laser: an in vitro study. Lasers Med Sci. 2009; 24:1-5.
8. Danesh G, Davids H, Reinhardt KJ, Ott K, Schafer E. Polymerisation characteristics of resin composites polymerised with different curing units. Journal of Dentistry 2004;3: 479-488.
9. Light curing of resin-based composites in the LED era.American Journal of Dentistry 2008; 21(3):135-142.
10. Caughman WF, Rueggeberg FA and Curtis JW. Clinical guidelines for photocuring restorative resins. J Am Dent Assoc 1995; 126:1280-1286.
11. Friedman J. Care and maintenance of dental curing lights. Dentistry today 1991;10:1-2.
12. Bayne SC: Dental Materials.Sturdvents, Art and Science of operative dentistry 4th Ed. USA. Mosby, 2002:133-233.
13. Miyazaki M, Hattori T, Ichiishi Y, Kondo M, Onose H, Moore BK. Evaluation of curing units used in private dental offices. Operative Dent 1998;23:50-4. |