Introduction:
Until the recently required use of barrier techniques during treatment of patients , sterile surgical gloves were generally not used routinely when exodontic procedures were performed. Surgical gloves are generally accepted as a good barrier against cross-infection between operators and patients. Sterile gloves are normally worn for surgical procedures to maintain sterility during the operation, in order to minimize postsurgical infection. This randomized, prospective study was designed to compare the postoperative infection rate following dental extraction by wearing clean gloves to sterile gloves, to identify any complicating factors on socket healing, and whether there is now a need to use expansive sterile gloves during such procedures or whether non sterile ; but clean, gloves can be used.
Methods & Material:
This prospective study is conducted in a postgraduate institute from June- 2009 to September-2009. Subjects selected were those referred for extraction. Patients who were taking antibiotics for current infection or required antibiotic prophylaxis prior to extraction, E.g: For valvular heart disease or prosthetic joint replacement were excluded. The relevant pre-operative information recorded in the protocol included the participant's medical history as diabetes mellitus ; informed consent and excludes the medical condition such as history of radiotherapy, smoking and drinking habit. The reasons for extraction and any intraoperative complications, such as crown or root fracture, prolonged bleeding etc. were also noted.
Patients were assigned to either dental surgeons or dental students and were allocated to the sterile and clean gloves group using a randomization table. After informed consent was obtained from the subjects, extraction was performed in the usual manner and no postoperative antibiotics were prescribed. The same postoperative instruction were provided to all patients and they were given an appointment to return in 3 days and 6 days respectively for assessment of complication in socket healing. The operated / surgical site was considered to be infected if one or more of the following clinical signs were present and diagnosis was made as follows:
1. Inflamed socket-painful socket with exuberant inflamed tissue, but without pus or systemic fever.
2. Infected socket-pain, redness, swelling, pus discharge and systemic fever.
3. Dry socket-persistent throbbing pain and exposure of bare alveolar bone.
A total of 200 patients attended the out patient clinic for dental extractions under local anesthsia. In Sterile glove group (n=100), 10 patients didn`t report on 3rd day ( n= 90) & 6 patients didn`t came on 6th days ( n= 84) for postoperative assessment. There for the drop-out rate for the study on 3rd day is 10% (10/100) and on 6th day is 6.6% (6/90). Also in Clean glove group (n=100), 8 patients didn`t report on 3rd day (n=92) and 5 patients didn`t came on 6th day ( n= 87) for postoperative assessment. There for drop -out rate for clean gloves group on 3rd day & 6th day are 8% (8/100) & 5.4% (5/92). The over all response rate was determined as 88%.
 |
 |
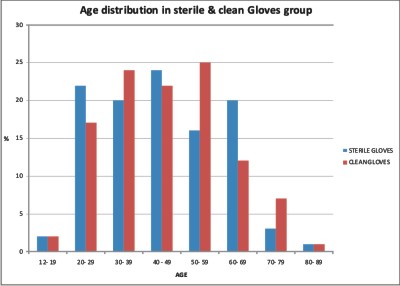
A total of 307 Extractions in 200 patients were obtained at the end of the study. The age range of patients was between 12-89 years old with the mean age of 53.3 years. The major group included those aged from 40-49 years old, which account for 23%. The percentage of other age group varied from 1% - 19%.
The common reason for extractions were retained roots, periodontal disease, retained deciduous and non -restorable carious teeth.
Eighteen patients (9%) presented with a history of Diabetes mellitus, in which two patients were uncontrolled diabetic.
 |
 |
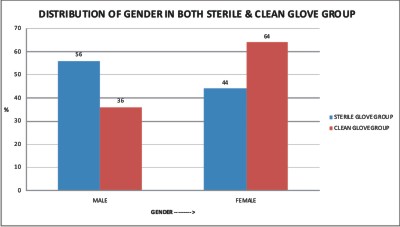
The study group of 200 patients was divided into the sterile glove group ( n=100) and clean glove group ( n=100) , having a sterile to clean gloves of 1:1. The male to female ratio in clean glove group was approximately 1:2 and in Sterile glove group was approximately 1.3: 1.
Dental surgeons performed extractions in 60% of the patients in each group , while extraction carried out by dental students account for 40%. The sterile and clean glove groups were analyzed separately and compared by chi-square test.
Results:
Postoperative Healing In Sterile And Clean Glove Groups:
Sterile Glove Group:
(I). ON 3RD DAY POSTOPERATIVE ASSESSMENT:
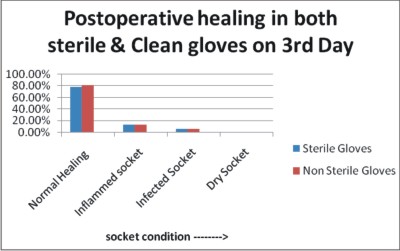
A total of 90 patient (n=90 = 100%) reported on 3rd day postoperative assessment, out of which 70 patient (77.77%) presented with uneventful wound healing, 12 patients (13.33%) were found to have inflammed sockets and 6 patients (6.6%) in this group was diagnosed as having an infected socket.
(ii). ON 6TH DAY POSTOPERATIVE ASSESSMENT:
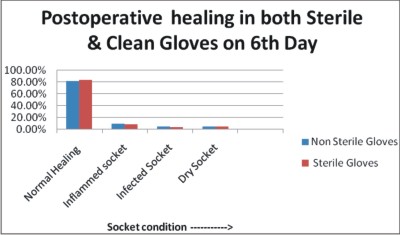
A total of 84 patient (n=84 = 100%) reported on 6th day postoperative assessment, out of that 70 patients (83.33%) presented with uneventful wound healing, 7 patients (8.33%) were found to have inflammed sockets and 3 patients (3.57%) in this group was diagnosed as having an infected socket. A dry socket was found in 4 patients (4.76%%).
Clean Glove Group:
(I). ON 3RD DAY POSTOPERATIVE ASSESSMENT:
A total of 92 patient (n=92 = 100%) reported on 3rd day postoperative assessment, out of which 74 patients (80.43%) presented with normal healing. An inflammed socket was found in 12 patients (13.04%). 6 patients (6.52%) in this group was diagnosed as having an infected socket.
(ii). ON 6TH DAY POSTOPERATIVE ASSESSMENT:
A total of 87 patient (n=87 = 100%) reported on 6th day postoperative assessment, out of that 71 patients (81.60%) presented with normal healing; 8 patients (9.19%) were found to have inflmmed sockets and 4 patients (4.59%) in this group was diagnosed as having an infected socket. A dry socket or Localised osteitis was found in 4 patients (4.59%).
 |
 |
 |
 |
There were no significant differences in the incidence of having an inflamed socket; infected socket and Dry socket between the two groups. The pattern of results observed between the two groups was very similar.
Contributing Factors To Postoperative Healing:
 |
 |
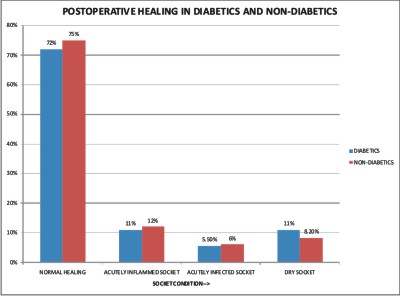
There was no significant difference found in the rate of postoperative infection between diabetic and Non-diabetic. Only one patient in the Diabetic group developed postoperative acutely infected socket (5.5%) , however, Eleven patients (6%) in the non-diabetic group presented with an infected socket on 6th postoperative assessment day. A dry socket was found in two patients (11%) in the diabetic group and fifteen patients (8.2%) in the non-diabetic group.
Postoperative Healing In Relation To Different Operators:
No significant difference in postoperative infection was found between the two groups of operators (Dental surgeon and Dental students). All extractions in case of infection were performed by both Dental surgeons and Dental students.
Discussion:
The concern of cross-infection during dental procedures, such as hepatitis B virus and human immunodeficiency virus (HIV), have prompted Health Authorities to recommend guidelines for the prevention of cross-infection. The Centre for Disease Control1 have published recommended infection control practices for dentistry. In their general guidelines for glove selection, published in 1988, the Center for Diseases control2 recommended use of sterile gloves during procedures involving contact with mucous membranes, unless otherwise indicated and during other patient care or diagnostic procedures that do not require the use of sterile gloves. It is noted here that the dental profession is currently working in a practice environment, in which the use of universal precaution has greatly increased the cost of treatment. The dentists also need to be concerned about the legal profession using litigation as a platform for setting standards of care, rather than such standards being determined by sound clinical evidence. This raises the question of whether the cost of a common dental procedure, such as exodontia, can be reduced by the use of clean gloves rather than sterile gloves.The use of clean gloves not only fulfils the standard of universal infection control and is considerably cheaper than the individually packed sterilized gloves.
The clinical use of Sterile and non-sterile gloves has been studied previously. Anderton and Aidoo3 investigated the ability of non-sterile, disposable gloves to reduce the level of microbial contamination introduced during enteral feeding. No contamination was reported while using non-sterile.
Giglio et al.4 revealed an interesting finding that microbiological swabbing from the palm of the worn gloves immediately before surgery indicated that bacterial organisms were present on 50% of sterile gloves and on 80% of clean gloves. They suggested that contamination of the sterile gloves was likely to be due to the improper gloving technique by the operators.
In this present study additional results found are:
1. The root or crown fracture during forceps extraction has no statistical influence on wound healing.
2. It was surprising to note that the incidence of acutely infected and dry sockets was slightly higher when the teeth were removed completely.
3. The indications for extraction were also confirmed to have no specific influence on developing a specific socket complication, except a small chance of developing infected and dry sockets from pre-operative retained roots or periapical pathology.
This study also found no difference in socket complications between the undergraduate dental students and qualified dental surgeons, which is reassuring for patients to be treated in teaching institutions.
Conclusion:
The result of this study helped to define the glove selection process.The study concluded that the use of sterile surgical gloves does not offer an advantage over clean gloves in minimizing socket inflammation, infection, as well as a dry socket following dental extraction. The use of clean gloves not only fulfils the standard of universal infection control but is considerably cheaper than the individually packed sterilized gloves; which is a significant consideration in developing countries like India. Hence, it is suggested that the cheaper, non-sterile, but clean, gloves can be worn during routine exodontic procedures, thereby reducing the cost of barrier technique and universal precaution.
References:
1. Centers for Disease control. Recommended infection control practices for dentistry. MMWR 1986; 36:237-242.
2. Centers for Disease control. Updates: Universal precautions for prevention of transmission of human immunodeficiency virus, hepatitis B virus, and other blood born pathogenesis in health-care settings. MMWR 1988; 37:377-382, 387-388.
3. Anderton A. Aidoo K E. The effect of handling procedures on microbial contamination of enteral feeds- a comparison of the use of sterile versus non-sterile gloves. J Hosp Infect 1991; 17:297-301.
4. GIGLIO JA, ROWLAND RW, LASKIN DM,GRENEVICK L, ROLAND RW. The use of sterile versus nonsterile gloves during out-patient exodontia [published erratum appears in Quintessence Int 1995 Aug; 26(8): 533]. Quintessence Int 1993: 24:543-545.
5. L. K. Cheung, L. K. Chow, M. H. Tsang, L.K.Tung: An evaluation of complications following dental extractions using either sterile or clean gloves. Int. J. Oral Maxillofac. Surg. 2001; 30:550-554.
6. Curi MM, Dib LL, Kowalski LP. Management of refractory osteoradionecrosis of the jaws with surgery and adjunctive hyperbaric oxygen therapy. Int J Oral Maxillofacial surg 2000:29;430-434.
7. Davies HT, Carr RJ. Osteomyelitis of the mandible : a complication of routine dental extractions in alcoholics. Br J Oral Maxillofac surg 1990: 28; 185- 188.
8. Devlin H, Garland H, Sloan P. Healing of tooth extraction sockets in experimental diabetes mellitus. J Oral Maxillofac surg 1996: 54; 1087-1091.
9. Tong AC, Leung AC, Cheng JC, Sham J. incidence of complicated healing and osteoradionecrosis following tooth extraction in patients receiving radiotherapy for treatment of nasopharyngeal carcinoma. Aust Dent J 1999: 44; 187- 194.
10. Vundiniabola S, Pirone C, Williamson J, Goss AN. Hyperbaric oxygen in the therapeutic management of osteoradionecrosis of facial bones. Int J Oral Maxillofac surg 2000: 29; 435-438. |