|
|
|
| Peripheral Ossifying Fibroma - A Case Report |
Hemant Batra 1 , Neeraj Sharma 2 , Anubha Gulati 3 , Sheeba Mohindra 4
1 Prof & HOD, Dept.of Oral & Maxillofacial Surgery - Dr. HSJ Institute Of Dental Sciences, Panjab University, Chandigarh
2 Sr. Asst.Prof, Dept.of Oral Medicine & Radiology - Dr. HSJ Institute Of Dental Sciences, Panjab University, Chandigarh
3 Assoc. Prof, Dept Of Oral Pathology - Dr. HSJ Institute Of Dental Sciences, Panjab University, Chandigarh
4 Assoc. Prof, Dept Of Oral Pathology - Dr. HSJ Institute Of Dental Sciences, Panjab University, Chandigarh
|
| Address For Correspondence |
Dr. Hemant Batra
Prof And Hod
Dept. Of Oral And Maxillofacial Surgery
Dr. HSJ Institute Of Dental Sciences
Panjab University
Chandigarh
Email: hemant_batra69@yahoo.com |
| Abstract |
| Peripheral ossifying fibroma (POF) is one of the several common reactive hyperplastic lesions of the gingiva. It arises from the gingival corium, periosteum, and periodontal ligament. Commonly used synonyms for POF include calcifying fibroblastic granuloma, peripheral fibroma with calcification, peripheral cementifying fibroma, and calcifying or ossifying fibrous epulis. This article presents a case of peripheral ossifying fibroma in a 55-year-old female along with the clinical, histopathologic, and radiographic features and treatment details. |
|
| Keywords |
| peripheral ossifying fibroma, gingival enlargement, fibroma |
|
| Full Text |
Introduction
The peripheral ossifying fibroma(POF) is a common gingival lesion manifesting as a localized gingival enlargement typically measuring less than 1.5 cm at its greatest dimensions. It varies from pale pink to cherry red in color, can be either pedunculated or sessile and is typically located in the interdental papilla region.1,2,3 It is more common in the young women. The majority of lesions occur during a person's second decade, with a declining incidence in later years.4 The lesion may cause a separation of the adjacent teeth, and occasionally minimal bone resorption can be seen beneath the lesion.5
Case Report
A 55 years old female patient reported to the department of oral medicine and radiology with an exophytic growth in the oral cavity which has been gradually increasing since the past three months. The swelling started as a small nodule. The patient did not give any significant medical history. Intraoral examination revealed poor oral hygiene and neglected dental condition. A well-demarcated, non-tender, firm, focal, sessile nodular growth arising from the gingiva of the maxillary left central and lateral incisors was seen. The oval-shaped mass was 1.5 cm x 2 cm in size, with a reddish pink color, smooth surface, and distinct edges. (Figure 1) Bleeding on probing was noted. An intraoral periapical radiograph and orthopantomogram of the maxillary central incisors showed no underlying bone involvement. Incidentally, an impacted mesiodens could be seen on the radiographs. (Figure 2) Clinically, differential diagnoses for the growth were pyogenic granuloma, peripheral odontogenic fibroma, fibroma, and peripheral giant cell granuloma. A provisional diagnosis of pyogenic granuloma was made for the gingival growth.
Under local anesthesia, the lesion was completely excised. (Figure 3) The excisional biopsy was submitted for histological analysis. The histo pathological examination of the lesion revealed the prominent area of highly cellular fibrous connective tissue showing collagen fibers and proliferating plump fibroblasts, and focal areas of round to ovoid calcifications. The covering stratified squamous epithelium was parakeratinized with focal areas of acanthosis. The underlying connective tissue was infiltrated with inflammatory cells and showed few dilated blood vessels engorged with red blood cells. (Figure 4 and 5) The diagnosis was POF according to both clinical and histopathological patterns. A five-month postsurgical follow-up showed no evidence of recurrence.
 | Figure 1. Intra-oral view showing a sessile growth arising from the gingiva of maxillary left central and lateral incisors.
 |
 | Figure 2. Orthopantomogral showing no underlying bone involvement. An impacted mesiodens is seen.
 |
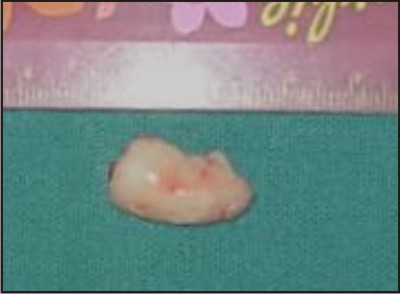 | Figure 3. Excised tissue.
 |
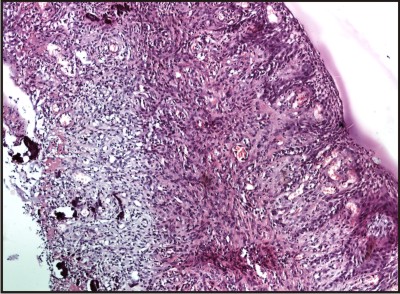 | Figure 4. Histopathological picture showing fibrous connective tissue covered with stratified squamous epithelium.
 |
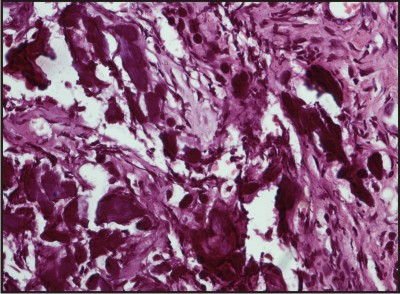 | Figure 5. Round to ovoid cementum like calcifications seen. H-E staining X40.
 |
Discussion
The POF occurs almost exclusively on the free margin of the gingiva and usually involves the interdental papilla. The fact that the lesion emerges from the periodontal ligament and is not seen in edentulous areas suggests its origin to be the connective tissue elements of the periodontal ligament.6 Dental calculus, plaque, dental appliances, ill-fitting crowns, and rough restorations are considered to be the irritants causing its growth.7 Factors such as a high female predilection and a peak occurrence in the second decade of life also suggest of hormonal influences.8 Sixty percent of the lesions occur in the maxilla, with more than 50% occurring in the incisor- canine region.9,10 The associated teeth are usually not mobile.
Roentgenographically, in a vast majority of cases there is no apparent underlying bone involvement visible. On rare occasions, there appears to be superficial erosion of bone.11 Radiopaque foci of calcifications have been reported to be scattered in the central area of the lesion, but not all lesions demonstrate radiographic calcifications.12 A minor adjustment of exposure settings (decrease of kilovolt peak; increase of milliampere) is recommended for showing the tiny radiopaque foci.
The clinical features are not sufficient for the diagnosis of POF because there are other conditions that may have similar clinical appearances and clinical courses such as pyogenic granuloma and peripheral giant cell granuloma. Therefore biopsy and histopathological examination is required for definitive diagnosis.
In the present case the findings except for age correlated the general characteristics and there was no underlying bone involvement. The patient had poor oral hygiene, which probably contributed with etiopathogeny of the POF.
Considerable confusion has prevailed in the nomenclature of POF with various synonyms being used such as peripheral cementifying fibroma, ossifying fibro-epithelial polyp, peripheral fibroma with osteogenesis, peripheral fibroma with cementogenesis, peripheral fibroma with calcification, calcifying or ossifying fibrous epulis and calcifying fibroblastic granuloma.13
Histopathologically, the lesions show excessive proliferation of mature fibrous connective tissue. Chronic irritation of the periosteal and the periodontal membrane causes metaplasia of the connective tissue and resultant initiation of formation of bone or dystrophic calcification.12 There are three types of mineralized tissue in the POF: dystrophic calcification, bone (woven or lamellar), and cementum- like material. The dystrophic calcification is most prevalent in ulcerated lesions.4 Ossification or calcification may not be evident in all cases, particularly in the earlier stages of lesional growth.
It is suggested that there is no absolute histological distinction between bone and cementum, and as the so-called cementum-like globules of calcification are seen in fibro-osseous lesions in all membrane bones, it is unrealistic to separate the ossifying and cementifying lesions and it is speculated that the fibro-osseous lesions might represent stages in the evolution of a single disease process passing through the stages of fibrous dysplasia to ossifying fibroma to cementoid lesions.14
After the elimination of the local etiological factors like plaque, calculus, ill fitting dentures and poor quality restorations, local surgical excision of POF is the preferred treatment. Excision should include the periodontal ligament and the periosteum at the base of the lesion in order to reduce the chances of recurrence. However, total excision of the lesion in the maxillary anterior region can result in an unsightly gingival defect unless appropriate efforts are taken to repair the periosteal defects.1 Various different surgical techniques like lateral sliding flap of full thickness or partial thickness, subepithelial connective tissue graft, or coronally positioned flap may be used to manage this defect and minimize patient esthetic concerns. Recurrence rates of 8-20% have been reported.14,15 The recovery of our patient was uneventful and is on regular follow-up.
Conclusion
In conclusion, a slowly growing soft-tissue mass in the anterior oral cavity should raise a suspicion of a reactive gingival lesion such as POF. It is a benign fibro-osseous lesion with significant growth potential. Histopathological examination is essential for accurate diagnosis. Once diagnosed, POF should be treated by total excision to prevent recurrence.
References
Kfir Y, Buchner A, Hansen LS: Reactive lesions of the gingiva. A clinicopathological study of 741 cases. J Periodontol 51:655, 1980
1. Walters JD, Will JK, Hatfield RD, Cacchillo DA, and Raabe DA. Excision and repair of the peripheral ossifying fibroma: a report of 3 cases. J Periodontol 2001;72(7):939-944.
2. Neville, et al. Text book of oral and maxillofacial Pathology. 2nd ed. West philadelphia:Saunders 2004.p. 451-452.
3. Martin S. Greenberge, et al. Burket's Oral medicine. 11th edn. Hamilton: BC Decker Inc, 2008:133-134.
4. Buchner A, Hansen LS. The histomorphologic spectrum of peripheral ossifying fibroma. Oral Surg Oral Med Oral Pathol. 1987;63(4):452-461.
5. Norman K. Wood, Paul W. Goaz. Differential Diagnosis of Oral and Maxillofacial Lesions. 5th edn. St Louis: Mosby, 2006:143-144.
6. Marx RE, Stern D. Oral and maxillofacial pathology: a rationae for diagnosis and treatment.Quintessence pubishing, Illinois 2003:25
7. Gardner DG: The peripheral odontogenic fibroma: An attempt at classification. Oral Surg Oral Med Oral Pathol 1982;54:40-48.
8. Kenney JN, Kaugars GE, Abbey LM. Comparison between the peripheral ossifying fibroma and peripheral odontogenic fibroma. J Oral Maxillofac Surg. 1989;47(4):378-382.
9. Buchner A, Hansen LS: The histomorphologic spectrum of peripheral ossifying fibroma. Oral Surg Oral Med Oral Pathol 1987;63:452-461.
10. Poon C, Kwan P, Chao S. Giant peripheral ossifying fibroma of the maxilla: Report of a case. J Oral Maxillofac Surg 1995;53:695-8.
11. Rajendran R. Benign and malignant tumors of oral cavity. In: Shafer WG , Hine MK, Levy BM. Shafer's Textbook of Oral Pathology. 5th ed. Philladelphia, PA: W.B. Saunders Co; 2006:113-308.
12. Kendrick F, Waggoner WF. Managing a peripheral ossifying fibroma. J dent Child 1996;63:135-138.
13. Kumar SK, Ram S, Jorgensen MG, et al. Multicentric peripheral ossifying fibroma. J Oral Sci. 2006;48(4):239-243.
14. Langdon JD, Rapidis AD, Patel MF. Ossifying Fibroma-One Disease or Six? An Analysis of 39 Fibro-Osseous Lesions of the Jaws. Br J Oral Surg 1976;14:1-11.
15. Kenney JN, Kaugars GE, Abbey LM. Comparison between the peripheral ossifying fibroma and peripheral odontogenic fibroma. J Oral Maxillofac Surg 1989;47:378-82.
16. Cuisa ZE, Brannon RB. Peripheral ossifying fibroma: A clinical evaluation of 134 pediatric cases. Pediatr Dent 2001;23:245-8. |
|
|
|
|
|
|