Introduction
Extensive bilateral midfacial defects involving the upper jaw, palate, and sinus presents a reconstructive challenge (Panje, W.R., H.E. Hetherington, 1995). Bilateral complete maxillectomy is a relatively uncommon surgical procedure resulting in devastating effects on the cosmetic, functional, and psychological aspects of a patient’s life (Sjowall, L., C. Lindqvist, 1992). Prosthetic restorations have become the preferred method for the rehabilitation of complex mid-facial defects like the bilateral maxillectomy. They allow rapid, single stage reconstruction which is important since improvement in the quality of life is of paramount concern, for many of these patients surgery may be only palliative (Johnson, J.T., M.A. Armani, 1983). Post surgical prosthetic rehabilitation of complete maxillectomy patients is a subject seldom discussed in the literature (Sjowall, L., C. Lindqvist, 1992). Many of these patients show poor prosthetic prognosis due to lack of a stable underlying bed of supportive hard tissue for stability and retention of the prosthesis.
Bilateral maxillectomy affects a variety of functions like mastication, speech, olfactory, and gustatory sensations. These patients also experience problems like seepage of nasal secretions into the oral cavity, poor lip seal, xerostomia, (Wang, R.R., 1997) exophthalmoses, and diplopia (Panje, W.R., H.E. Hetherington, 1995). Complete rehabilitation of a bilateral maxillectomy patient can be achieved using a multidisciplinary team approach involving both surgical and prosthetic personnel.
Factors influencing the prognosis of prosthetic reconstruction in these patients are the size of the defect, availability of hard and soft tissues in the defect area to provide support for the prosthesis, (Des Jardins, R.P.,1978) proximity of vital structures, patient attitude, temperament, systemic conditions, and the patient’s ability to adapt to the prosthesis (Brown, K.E., 1970).rehabilitation of a bilateral maxillectomy patient can be achieved using a multidisciplinary team approach involving both surgical and prosthetic personnel.
Case Report:
A 56-year-old male patient reported to the department of prosthodontics of Vinayaka mission’s dental college and hospital for replacement of his existing obturator which was not retentive and patient had difficulty in speech and deglutation. The patient’s medical history revealed that he had undergone a surgical intervention for adenocystic carcinoma involving the right and left maxilla and left maxillary sinus. The resection of bilateral maxilla was done. On extra-oral examination partial zygomectomy was done , the face appeared asymmetrical and had mid-facial deficiency.(fig .1). Intra-orally the nasal septum and lateral wall of the nose could be visualised (fig .2). Orthopantamogram (OPG) (fig.3) also shows absence of maxilla . This type of resection presents a difficult situation mechanically for obturator fabrication. The upward and outward direction of the mandibular closure will tend to force the prosthesis in that direction rotating around the most anterior rests. The force of gravity will tend to dislodge the obturator in a downward direction rotating around a fulcrum through the most posterior rest . But in this particular case there was no posterior rest and so engaging the undercuts wherever possible is necessary to resist these two distinct dislodging tendencies.
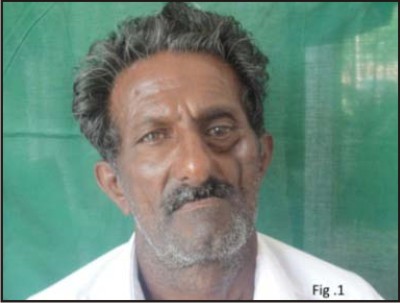 | Figure 1
 |
 | Figure 2
 |
 | Figure 3
 |
Procedure:
In order to fabricate the obturator preliminary impression was made with the low fusing impression compound material. As the impression compound is rigid, irreversible hydrocolloid material is used to record the defective areas i.e nasal septum and undercuts around it. A special tray was fabricated . The nasal aperture was blocked and Secondary impression was made with the putty (poly vinyl siloxane) elastomeric impression material. Light body elastomeric impression material was used to record the finer details of the defect area (fig.4). Master cast was made(fig.5). In this particular case neither any remaining teeth nor ridge was present for the retention of the prosthesis through clasps , only undercuts helps in this case.
The occlusal rims for maxillary and mandibular arch were fabricated. Jaw relation was done. Articulation was done. Wax try-in was done and the denture was fabricated(fig.6). Palatal surface of the denture was reduced to about 2mm thickness in order to reduce the weight of the prosthesis(fig.7). Then the prosthesis was tried in the patients. We found a compromised retention because during the process of denture fabrication few of the undercuts had to blocked out for the denture to be retrieved from the cast . Patient may be uncomfortable with the rigid denture base in those fragile areas of nasal septum and may cause soreness as well. In order to improve the retention soft reliner ( Ufi gel P, voco) was used in the tissue surface in the defect areas (fig.8). Once the soft relining was done the denture had a better retention and the patient was comfortable .
To reduce the weight of the prosthesis, the bulb portion of the obturator is generally hollowed after it has been processed into acrylic resin. Weight reduction is especially important when the obturator prosthesis is suspended without bony or posterior tooth support on the defect side, as is the case with most maxillary resection prostheses. A hollow maxillary obturator may reduce the weight of the prosthesis by up to 33%, depending upon the size of the maxillary defect. In order to give the palatal feel for the patient hollow bulb was fabricated with the lost salt technique and checked for buoyancy(fig.9). The final prosthesis was delivered to the patient and patient had better appearance and phonation and comfort. Depending upon the nature of the defect, movement of the obturator varies and creates soreness and discomfort for the patient. These pressure sores are adjusted at the post insertion and subsequent follow-up appointments. Optimal outcome of the obturator prosthesis depends on the successful integration of the prosthesis with the patient’s oral functions plus psychological acceptance of the obturator by the patient. Firmly retained prosthesis can provide the patient with psychological support during the difficult period after maxillectomy.
 | Figure 4
 |
 | Figure 5
 |
 | Figure 6
 |
 | Figure 7
 |
 | Figure 8
 |
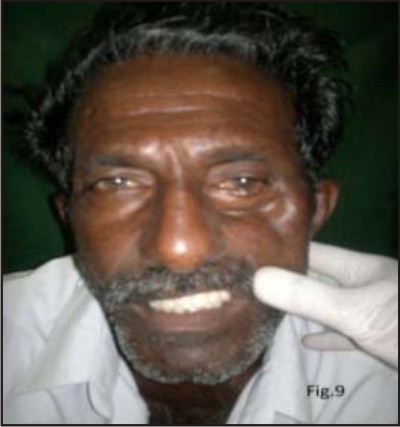 | Figure 9
 |
Discussion
In dentate patients, primary retention, support, and stability of an obturator depend on the number and distribution of remaining teeth . Engagement of soft tissue undercuts including the scar band at the skin graft-mucosal junction, may also play a significant role particularly in edentulous patients. Wide surgical resections for the control of malignancies frequently result in a small number of remaining or no teeth with complete resection of ridge. In this case scar bands, soft tissue undercuts serve as abutments for the obturator and are subjected to constant, non-axial, cantilever forces. The skin graft-mucosal junction scar band will also stretch out over time and become ineffective in helping to retain the obturator.
Structural durability is mandatory for longevity of the prosthesis. In these patients, chewing function is not confined due to the lack of support on the surgical defect side. The bulb portion of the obturator is designed so that the 3D configuration of congruous vertical and horizontal walls offset crack development and fracture propagation. Tensile stress accumulation developing along the midline of conventional complete dentures resulting in fatigue fracture .
A stable record base is critical for recording an accurate maxilla-mandibular relationship and in evaluation of the esthetics and phonetics of the wax try-in prosthesis. The fit and stability of the record base for an obturator, however, is often compromised because of the size of the surgical defect and is further compounded by the need to block out undercuts and by under-extended borders. Conventional record bases can rotate into the defects when attempting the centric relation record, resulting in an inaccurate record. A processed record base provides maximum support, retention, and stability for a maxillofacial prosthetic patient and additional steps of relining the record base with silicone resilient materials can be avoided. But in this case the undercuts extends into to fragile region into which the rigid denture base can’t be extended. Thus the soft reliners should be used in such cases.
Summary
The pre-surgical treatment planning is of great importance not only for the patient but also for the success of the surgical procedure and prosthesis. In different clinical scenarios whether in partially dentate and/or edentulous patients both hard and soft tissues are essentially required for the fabrication of a stable and functional prosthesis. During prosthodontic rehabilitation the support can be gained from within the defect and remaining structures. Retention can be achieved from the non-resected tissue, scars and bony undercuts by conventional and unconventional means.
References
1. Taylor TD. Clinical Maxillofacial Prosthetics. Quintessence Publishing Co. Illinois, USA. 2000. pg 85,105.
2. Tirelli G,Rizzo R,Biasatto M,Di Lenarda R,Argenti B,Gatto A,Bullo F.Obturator prostheses followingpalatal resection:clinical cases. Acta Otorhinolaryngol Ital.2010 Feb;30(1):33-9
3. Lethaus B,Lie N,de Beef F,Kessler P,de Baat C,Verdonck HW. Surgical and prosthetic reconstructions in patients with maxillectomy. J Oral Rehabil. 2010 Feb;37(2):138-42.
4. Laney WR. Maxillofacial prosthetics: Postgraduate Dental Handbook Series, Volume 4. PSG Publishing Company Littleton, Massacheusetts 1979.
5. Rahn AO, Goldman BM, Parr GR. Prosthodontic principles in surgical planning for maxillary and mandibular resection patients. J Prosthet Dent 1979;42:429-33.
6. Marunick MJ, Harrison R, Beumer J. Prosthodontic rehabilitation of midfacial defects. J Prosthet Dent 1985;54:553-60.
7. Yazdanie N and Manderson RD. Prosthetic management and rehabilitation of an extensive intraoral and facial defect. Int J Prosthodont 1989;2:550-4.
8. Yamamoto Y. Mid-facial reconstruction after maxillectomy. Int J Clin Oncol. 2005 Aug;10(4):218-22.
9. Ali A, Patton DW, Fardy MJ. Prosthodontic rehabilitation in the maxilla following treatment of oral cancer. Dental update 1994; :282-6. |