|
|
|
| Cemento - Ossifying Fibroma - A Case Report |
Sudhakara Reddy.K 1 , Girish Rao. S 2
1 PostGraduate Resident, Dept of Oral & Maxillofacial Surgery - RV Dental College, Bangalore
2 Professor & Head, Dept of Oral & Maxillofacial Surgery - RV Dental College, Bangalore
|
| Address For Correspondence |
Dr. Sudhakara Reddy.K
PostGraduate Resident
Dept of Oral & Maxillofacial Surgery
RV Dental College & Hospital,
JP Nagar, Bangalore
Phone : +91-08026658411
Mobile No: +919845198455
E-mail: drsudhakarareddy@gmail.com
k_sudhakarreddy@yahoo.com |
| Abstract |
| The cemento-ossifying fibroma is a central neoplasm of bone as well as periodontium affecting the jaws and other craniofacial bones. They commonly affect adults between the third and fourth decade of life and manifest as slow-growing, assymptomatic, intraosseous masses. An accurate diagnosis requires careful clinical, radiological and histological correlation in order to make an optimal treatment and an excellent outcome. They are insensitive to radiotherapy and recurrences are uncommon. Surgical enucleation or resection is the treatment of choice.
This article reports a case of 35 years old male who came to us with the history of swelling in the maxillary anterior region that was asymptomatic except in causing disfigurement. Clinically, there was an expansion of the buccal plate but not the lingual plate of the anterior part of maxillary alveolar region. The covering mucosa was normal and there was no tenderness or parasthesia. Radiographically, well-defined radiolucent area present between the permanent maxillary central incisors flecked with multiple small radiopacities. Surgical excision under local anesthesia was done, followed by primary closure. The patient was asymptomatic in the 3 years of periodic follow up. |
|
| Keywords |
| Cemento-ossifying fibroma, fibro-osseous lesions, ossifying fibroma, Cementifying fibroma |
|
| Full Text |
Introduction
Cemento - Ossifying Fibroma otherwise called as Cementifying fibroma or Ossifying fibroma is a relatively rare tumor which is classified under Fibro-osseous tumors. WHO defined it as demarcated or rarely, encapsulated neoplasm consisting of fibrous tissue containing varying amounts of mineralized material resembling bone and/or cementum. They can arise from any part of the facial skeleton and skull with over 70 per cent of cases arising in the Head and neck region.1 Cases involve mainly the mandible and maxilla but occasionally, reported in the orbitofrontal bone, nasopharynx, paranasal sinuses and skull base.
The first description of a variant of ossifying fibroma, was given by Menzel in 1872, 2 calling it a cemento-ossifying fibroma, in a 35-year-old woman with a long-standing large tumor of the mandible. It is a reactive gingival lesion that is believed to arise from cells of the periodontal ligament 3 or periosteum.
Clinical Features
This tumor is more common in young and middle-aged adults. There is a marked predilection for the female sex, which has been reported as high as 5:14. Most often, it is located in the gingival papilla between adjacent teeth. Because of the close proximity and similarity to the periodontal ligament tissue have led to the assumption that they are of periodontal tissue origin thus the term periodontoma some times is applied but this theory remains unexplained 5
The mandible is more commonly involved than the maxilla. The lesion is generally asymptomatic until the growth produces a noticeable swelling and mild deformity;
Radiographic Features
The Cemento - Ossifying Fibroma presents as a well defined unilocular or multilocular lesion with smooth contours. The maturity of the lesion will determine the degree of radio opacity. In the initial stage, it appears as a radiolucent lesion with no evidence of internal radio opacities. As the tumor matures, there is increasing calcification so that the radiolucent area becomes flecked with opacities until ultimately the lesion appears as an extremely radiopaque mass. Nevertheless, majority of the lesions demonstrate varying degrees of radiolucency. There is a centrifugal growth pattern rather than a linear one and therefore the lesions grow by expansion equally in all directions and present as a round tumor mass usually.
Histological Features
Histologically, Cemento-ossifying fibromas are well circumscribed, occasionally encapsulated, consisting of cellular fibrous tissues and thin isolated trabeculae of bones. The bone may show osteoblastic rimming and spherical deposits of calcified material, which are relatively acellular resembling cementum. As the lesion matures, the islands of cementum increase in number, enlarge, and ultimately coalesce.
Treatment
The lesion, which is usually well circumscribed and and this facilitates its extirpation from the surrounding bone, should be excised. Recurrence is rare.
Case Presentation
A 35 yrs old male patient has been referred to our unit for the swelling on his gums in the upper front region of the mouth (Figure 1). The medical, social and family histories were unremarkable.
 | Figure 1: Pre operative profile
 |
Patient noticed small swelling 6 yrs back .Initially it was 2-3mm and gradually increase to present size. Swelling was non-tender. On local examination, there is a noticeable swelling of 4×3cm extra orally on the anterior maxilla pushing the upper lip outward. Intraorally, Single diffused pale pink swelling in labial gingiva in relation to 11, 21, and 22 extending superiorly from the depth of vestibule to the gingival margin the obliterating vestibule. (Figure 2)
 | Figure 2: Pre operative Intra orally
 |
Surface is smooth and shiny. Blood vessels are seen on the superior surface of the swelling. On palpation labial swelling is non-tender, bony hard in consistency non fluctuant, fixed to underlying tissues, non compressible and non pulsative. There was an expansion of the buccal plate but not the lingual plate of the anterior part of maxillary alveolar region. Teeth 21, 22 are tender on percussion, Teeth 21 was grade-II mobility, and Teeth 22 was Grade -III mobility. Periodontal pockets measuring 1cm in length present in distal aspect of 22. Routine blood examination was done and showed Hb: 12 gm%; TLC: 12900/mm 3 ; DLC: neutrophils 65%, lymphocytes 27%, eosinophils 2%, and basophils and monocytes 0%. The erythrocyte sedimentation rate was 24 mm at 1 h, bleeding time was 2.55 min, and clotting time 6.35 min.
Radiographically, the orthopantomograph (Figure 3.1)
 | Figure 3.1: OPG
 |
showed a large radiolucent lesion with patchy mineralization extending from the lateral incisor region to the opposite side incisor region. The lesion was well demarcated with sclerotic border and heterogeneous in contrast. The lesion extended mesiodistally from the area of lateral incisor region to the opposite side incisor area and superioinferiorly from 3mm below the pyriform aperture to the apices of upper anterior teeth. No evidence of cortical erosion was noticed, though difficult to judge in orthopantomograph view. An occlusal view radiograph (Figure 3.2)
 | Figure 3.2: Occlusal View
 |
revealed a well-defined radiolucent area present between the permanent maxillary central incisors, with displacement of incisors posteriorly and to either side towards the canines. The region was flecked with multiple small radiopacities.The radiographic differential diagnosis included odontogenic keratocyst, odontogenic myxoma, cemento-ossifying fibroma, focal cemento-osseous dysplasia and central giant cell granuloma.
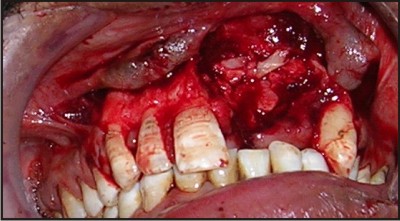
Surgical excision was planned under local anesthesia. Crevicular with releasing incision (Figure 4) given extending from canine to canine. Extraction of 21, and 22 done. Complete excision of the mass done. (Figure 5.1 & 5.2)
 | Figure 4: Incision exposing the lesion
 |
 | Figure 5.1: Excisional Lesion
 |
 | Figure 5.2: Residual Area
 |
Bone graft taken from the symphysis region has been placed in the defect followed by primary closure of the wound with 3-0 silk sutures. (Figure 6.1 & 6.2) The excised mass was sent to the pathology department for this to pathological examination which confirmed the diagnosis as cemento-ossifying fibroma. Antibiotics and anti-inflammatory agents were continued for the next 1 week. Alternate sutures were removed on the fifth postoperative day and the remaining sutures on the seventh postoperative day. Patient was followed up for 3 years post operatively and showed good result. (Figure 7)
 | Figure 6.1: Bone Graft In Place
 |
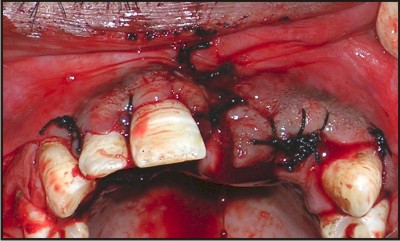 | Figure 6.2: Closure
 |
 | Figure 7: Post Operative
 |
Discussion
The cemento-ossifying fibroma is a benign osseous tumor that commonly affects adults of middle age, 30-40 years. It may present as small radiolucent areas close to the apices of teeth that could be mistaken for periodontal pathology. What is common in both cases is the lack of symptoms and non-specific radiolucency (the absence of intra-lesional calcifications).
They are composed of varying amounts of cementum, bone, and fibrous tissue. The name central cementoossifying fibroma is used because there is a spectrum of fibroosseous lesions that arise from the periodontal ligament, ranging from those with only deposition of cementum to those with only deposition of bone.
Central cementoossifying fibromas occur more frequently in women than in men. They arise in the mandible in 62% to 89% of patients, 77% occurring in the premolar region. Most are diagnosed between 20 and 40 years of age6. Central cementoossifying fibromas are asymptomatic until they cause expansion. Thus, they are generally not diagnosed until the tumor has had time to produce calcifications. They are typically well-defined, solitary radiolucencies with scattered radiopaque foci. They maintain a spherical shape, expand the surrounding cortical bone without cortical perforation, and may cause tooth divergence.
Pathologic examination of the central cementoossifying fibroma shows a proliferation of irregularly shaped calcifications within a hypercellular fibrous connective tissue stroma. The calcifications are extremely variable in appearance and represent various stages of bone and cementum deposition. Histologic differentiation between osteoid and cementum is difficult. In some cases, most of the calcified fragments are immature cementum, with basophilic coloration on hematoxylin and eosin-stained sections.
The radiographic appearance is invariably a mixture of radiolucency followed by more radiopacity which means the tumor was undergoing maturation and that ossification phase accounting for the increased density.
The differential diagnosis includes other lesions that contain radiopacities within a well-defined radiolucent mass: osteosarcoma, fibrous dysplasia, odontogenic cysts, squamous cell carcinomas, calcifying odontogenic cysts (Gorlin cysts), and calcifying epithelial odontogenic tumors (Pindborg tumors). The well-defined border of the central cementoossifying fibroma helps differentiate it from the aggressive sarcomas and carcinomas. Fibrous dysplasia has a characteristic "ground glass" appearance not seen in the central cementoossifying fibroma. The radiologic differentiation of central cementoossifying fibroma from Gorlin cysts and Pindborg tumors is difficult; the final diagnosis is based on histologic appearance. Pindborg tumors have a high association with impacted teeth .
The recommended treatment of the central cementoossifying fibroma is excision. Central cemento ossifying fibromas usually "shell out" easily at surgery, but maxillary central cementoossifying fibromas are more difficult to remove completely than mandibular central cementoossifying fibromas. This may be attributable to the difference in bone character between the mandible and maxilla and to the available space for expansion in the maxillary sinus.
Recurrence has been reported in as many as 16-28% 7of patients with mandibular central cementoossifying fibromas.
References:
1. Cemento-ossifying fibroma with mandibular fracture. Case report in a young patient Australian Dental Journal 1998;43:(4):229-33
2. Su L, Weathers DR, Waldron CA. Distinguishing features of local cementoosseous dysplasia and cementoossifying fibromas. I A pathologic spectrum of 316 cases. Oral Med Oral Pathol Oral Surg 1997; 84: 301-309.
3. Kramer IRH, Pindborg JJ, Shear M. Neoplasm and other lesions related to bone. In: WHO. Histologic typing of odontogenic tumors. Berlin. Springer-Verlag;1992. p.28-31
4. Eversole LR, Leider AS, Nelson K.Ossifying fibroma: a clinicopathologic study of sixty-four cases. Oral Surg Oral Med Oral Pathol. 1985; 60:505-11
5. Vlachou S, Terzakis G, Doundoulakis G, Barbati C, Papazoglou G. Ossifying fibroma of the temporal bone. J Laryngol Otol. 2001; 115:654-6.
6. Kuta AJ, Worley MacDonald, Kaugars GE. Central Cementoossifying fibroma of the maxillary sinus: A review of six cases. AJNR 1995; 16: 1282-1286
7. Buchner A, Ficarra G, Hansen LS: Peripheral odontogenic fibroma. Oral Surg Oral Med Oral Pathol 1987 Oct; 64(4): 432-8
|
|
|
|
|
|
|