INTRODUCTION
Eyes are generally the first features of face to be noticed. Removal of this organ either due to tumors,
trauma or any other condition not only cause unaesthetic look but also there is loss of function and has
a psychological effect on the patient. Thus, ocular prosthesis should be provided as soon as possible
for the psychological well being of the patient. A congenital anomaly or pathology may necessitate an orbital evisceration or an orbital enucleation. The surgical procedure of evisceration is where the contents of the globe are removed, leaving the sclera intact. A more invasive procedure is enucleation where the entire eyeball is severed from the muscles and optic nerve. Exenteration, the most radical, involves removal of the contents of the orbit.
CASE REPORT
A 55-year-old male was referred to Department of Prosthetic Dentistry from the Ophthalmology
Department. On history it was found that the patient was suffering from malignant melanoma of the
right eye and the eye had to be enucleated. So surgery was done and the eye was enucleated . On examination of the patient 15 days after the surgery, it was decided that a custom-made ocular
prosthesis would be the best to meet the needs of the patient as the extra effort that is put into
fabrication of a custom-made prostheses would enhance the esthetics and functional results rather
than a stock ocular prosthesis
Evaluation of patient ocular defect
In a case of evisceration the extra ocular muscles are left intact and hence good mobility of the prosthesis is possible. So it becomes mandatory to do the defect evaluations. In according to standard procedure; the palpebral fissure was observed both in open and closed position to rule out any abnormality. Evaluation of the muscular control of the palpebrae and the internal anatomy of the socket in resting position and full excursive movement was performed. Mobility of the posterior wall of the defect was assessed. Condition of conjunctiva, depth of fornices, and presence of cul de sac was noted.
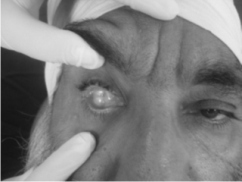 | Fig 1: Pre Operative
 |
Materials and Techniques -
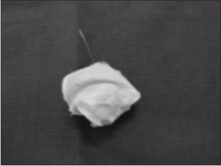
Impression and wax pattern fabrication-The impression of the anophthalmic eye socket was sought by introducing an impression material into the eye socket using a disposable syringe and projecting it out between the lids. The impression material used here was irreversible hydrocolloid (ALGINATE).After the impression material was set, the impression was removed and invested in dental gypsum in order to obtain a positive cast of the eye socket. Subsequently the gypsum cast was coated with a separating medium and white paraffin wax was then shaped in an empirical approximation of the anterior curves of the investment form.
 | Fig 2 : Impression Of Defect
 |
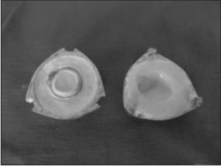
 | Fig 3 : Internal Surface Of Defect
 |
Trying the scleral wax pattern
Wax was added or trimmed from the basic sclera pattern until satisfactory contours of the eyelids were achieved in open and closed positions .
Technique of Iris Disc Placement
1 Transparent graph grid was used to attach iris disc.
2 Certain guidelines were marked on patients face.
3 The facial markings were transferred to grid by placing it on patients' face in place
 | Fig 4 : Try In Of Sclera Wax Pattern
 |
 | Fig 5 : Try In Of Sclera Wax Pattern
 |
Transparent Graph Grid
Markings were made on grid template on X-axis from A to H starting from midline and on left side from A' to H'. Similarly from 1 to 7 on Y-axis and 1' to 7' on left side. The distance between each marking was 1cm on both X and Y axes.
Guidelines on Patients Face
A vertical midline was marked passing through the forehead crease, glabella, tip of the nose and chin. The distance from the right eye medial canthus to the midline and left eye medial canthus to the midline was measured. This distance standardized the midline marking and was used to reposition the grid template each time during the try-in visit.
Evaluation with Grid Placed
The patient was asked to gaze straight at an object kept 4 feet away .The operator then marked the vertical lines coinciding with the with the medial and distal extremities of the iris of the natural eye. Similarly the horizontal lines referring to the centre, inferior and superior limits of the iris were marked. The facial markings were transferred to the grid template by placing it on the patients face .These markings were transported to the side of the defect. These markings were transferred to the sculptured wax pattern and the iris button attached to it.
Investing, Dewaxing, Packing
The finished pattern was invested in a small two piece brass flask. A two part mold was constructed by the prototype ocular prosthesis by using dental gypsum in a two piece brass flask, the anterior portion of the mold was invested, a separating medium was applied and the posterior portion of the mold was then invested. The flask was then placed in a dewaxing bath for 20 min. The anterior and posterior portions of the flask were separated. The iris disc was shade matched with the adjacent eye and cut out from a stock eye. The color of the sclera was selected using tooth color acrylic shade guide. Rayon thread fibrils were used to simulate vasculature, by monomer polymer syrup method. The selected shade of the sclera was matched with the heat cure resin which was then packed in the two piece flask. The flask was kept for curing for a period of two hours and thirty minutes to avoid any residual monomer.
 | Fig 6 : Dewaxing Of Eye Prosthesis
 |
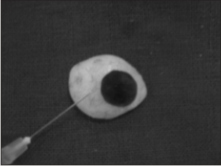 | Fig 7: Dewaxing Of Eye Prosthesis
 |
Placement Of Ocular Prosthesis
The Patient Was Instructed On The Aspects Of Insertion And Easy Removal Of The Prosthesis. Final Prosthesis Polished And Placed Into The Ocular Defect.
 | Fig 7 : Post Operative Photograph
 |
]
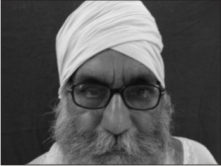 | Fig 8 : Post Operative Photograph
 |
Patient Follow up
The patient was asked to return on day 1, 2 and 7 for follow-ups after the prosthetic insertion.There after a 6 month follow-up was done for prosthesis evaluation and adjustment.
Discussion
The rehabilitation of the orbital defect is a complex task. A custom ocular prosthesis is a good option when reconstruction by plastic surgery or the use of osseointegrated implants is not possible or not desired. Systemic conditions and financial constraints may limit their use.
Advantages of a custom ocular prosthesis are:
1 Retains the shape of the socket.
2 Prevents collapse of the lids.
3 Provides proper muscular activity of the lids.
4 Prevents accumulation of fluid in the cavity.
5 Maintains palpebral opening similar to natural eye.
6 Has a gaze similar to natural eye.
7 Mimics coloration and proportions of natural eye
Conclusion:
The use of custom made ocular prosthesis has been a boon to the average patient who cannot afford the expensive treatment options available .The procedure used here is cheaper ,affordable and can be carried out in a small clinical set-up. This method has provided good results from patient esthetics, acceptance, and satisfaction points -of-view. Eye glasses that were used concealed the background effect and enhanced psychological comfort.
REFRENCES
1. A M Bhatt: Recent advances in the modeling of extraoral defects: JIPS: Oct-Nov: 2005: vol 5(4): 180-184.
2. Clinical Maxillofacial Prosthetics - Thomas D. Taylor.
3 Ivaniss Burgos, Daniel Nieves, Erick Rodriguez and Veronica Sanchez. : mechanics of biomaterials: eye prosthetic devices (ophthalamic tantalum clip/ conformer, artificial eye, absorbable implant, eye sphere, extraocular orbital implant, keratoprosthesis, intraocular lens, scleral shell, aqueous shunt ) May 2005 Applications of Engineering Mechanics in Medicine, GED-University of Puerto Rico.
4. Maxillofacial Rehabilitation - Prosthodontic and surgical consideration John Beumer.
5. Michael O. Hughes. : Ocular Implants and Orbital Reconstruction:Two Follow-Up Cases. Journal of Ophthalmic Prosthetics 2005.
6. P J Doshi et al.: Prosthetic management of patients with Ocular defects: JIPS: Jan-March 2005: vol 5(1): 37-38.
7. Varoujan A Chalian: Extraoral prosthetic: 286-294. |