Introduction: A large percentage of population suffers from periodontal disease and the sequelae of periodontal therapy. More specifically the periodontal surgical procedures can result in gingival recession and open gingival embrasures, commonly referred to as black triangles. These can be a cause of concern for the patient both functionally and aesthetically. Patient's consciousness and awareness of aesthetics make it imperative for today's discussion to understand and treat gingival recession and open gingival embrasures. It is not always possible to perform repeat surgical procedures to correct these problems and in this context a gingival prosthesis may be of value.
Black triangle can be defined as "Any interproximal soft tissue loss due to periodontal disease, traumatic, mechanical or chemical preparation or crown lengthening procedures"- G.PT-8 (1).
Gingival recession or gingival atrophy can be defined as "exposure of the tooth by the apical migration of the gingiva." (2).
Classifications:
Nordland and Tarnow classified the loss of papilla height into 4 classes based on three anatomical landmarks: interdental contact point, facial apical extent of CEJ and the interproximal coronal extent of the CEJ (3) (fig. 1). They are:
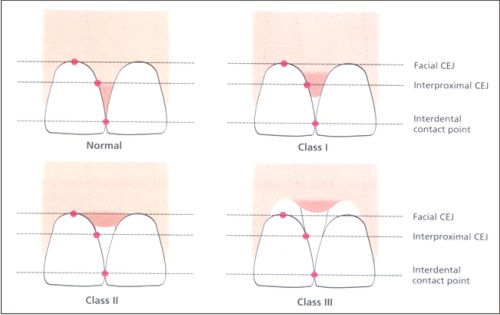 | Fig 1
 |
Normal: Interdental papilla fills the gingival embrasure to the apical extent of the interdental contact point/ area.
Class I : The tip of the interdental papilla is located between the contact point and the most coronal extent of the interproximal cemento-enamel junction (CEJ).
Class II: The crest of the papilla is at or apical to the interproximal CEJ but coronal to the facial CEJ.
Class III: Crest of the papilla is at or apical to the facial CEJ.
Various classifications have been proposed to describe gingival recession which include classifications by Sullivan and Atkins(1968) (4) , Mlineck (1978) (5), Liu and Salt (1980) (6), Bengue et al (1983) (7), Preston D Miller Jr (1985) (8), Mahajan's Modification - A Original Hypothesis (2010) (9), and the most followed classification being Mliller's classification.
Miller classified gingival recession into the following classes (8) (Fig.2).
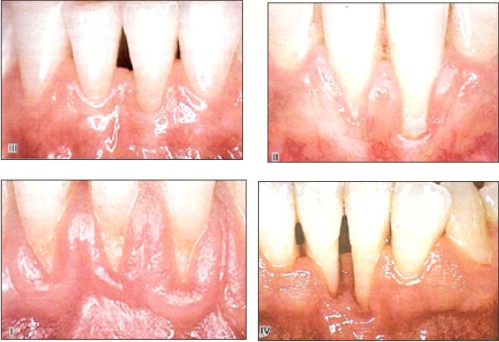 | Fig. 2. Millers Classification Of Gingival Recession From Top Left To Right Class I And II, A And Bottom Left To Right Class III And IV
 |
Class I: This includes marginal tissue recession that does not extend to the mucogingival junction. There is no loss of bone or soft tissue in the interdental area.
Class II: Class II consists of marginal tissue recession that extends to or beyond the mucogingival junction. There is no loss of bone or soft tissue in the interdental area.
Class III: In Class III, there is marginal tissue recession that extends to or beyond the mucogingival junction; in addition, there is bone and/or soft tissue loss interdentally or there is malpositioning of the tooth.
Class IV: There is marginal tissue recession that extends to or beyond the mucogingival junction with severe bone and soft tissue loss interdentally and/or severe tooth malposition.
Ajay Mahajan pointed out some drawbacks associated with the Miller's classification and suggested some changes to the Miller's classification in the year 2010 (9).
Class I: Gingival recession defect not extending to the MGJ.
Class II: Gingival recession defect extending to the mucogingival junction/beyond it.
Class III: Gingival recession defect with bone or soft-tissue loss in the interdental area up to cervical 1/3 of the root surface and/or malpositioning of the teeth.
Class IV: Gingival recession defect with severe bone or soft tissue loss in the interdental area greater than cervical 1/3rd of the root surface and/or severe malpositioning of the teeth.
Sequelae Of Black Triangles:
1. Phonetic problems
2. Aesthetic problems
3. Oral hygiene maintenance problems
Sequelae Of Gingival Recession:
1. Increased susceptibility of the teeth to caries,
2. Increased susceptibility to loss of tooth structure in the form of cervical abrasions ,
3. Sensitivity,
4. Hyperaemia of the pulp and associated symptoms,
5. Phonetic problems,
6. Oral hygiene problems and resulting plaque accumulation.
Gingival recession is mainly caused due to the cumulative effect of minor pathologic involvement and repeated minor direct trauma to the gingiva (2). The various etiological factors attributed to gingival recession include:
1. Faulty tooth brushing technique,
2. Tooth malposition,
3. Friction from soft tissues (gingival ablation) ,
4. Gingival inflammation,
5. Abnormal fraenum attachment,
6. Trauma from occlusion, and
7. Masochistic habits.
Management:
Management of gingival recession can be done by two approaches (2)
1. Surgical
2. Nonsurgical
Surgical Approach:
i) Free gingival auto graft
ii) Free connective tissue auto graft
iii) Pedicle auto graft
Coronally positioned
Laterally (horizontally) positioned
Semilunar pedicle (Tarnow)
iv) Sub epithelial connective tissue graft (Langer)
v) Pouch and tunnel technique
vi) Guided tissue regeneration
vii) Combined techniques
viii) Periosteal pedicle grafts (10)
NONSURGICAL APPROACH: This is done by
i) Correction of traumatic oral hygiene procedures (11) : if the causative factor for gingival recession is traumatic oral hygiene procedures, they should be discontinued immediately initially and modified subsequently.
ii) Orthodontic realignment of malposed teeth (11): in cases of diastemas and divergent roots or malposed teeth they should me orthodontically treated.
iii) Gingival veneering by using
1. Composites (12, 13): The newer composites are more colour stable and wear resistant, and the latest generation of dental bonding agents allows the bonding of composites to dentin, various metals, and porcelain. Disadvantages of this approach include chances of debonding, discoloration, seepage of fluids through the tooth-composite interface. .
2. Porcelain laminates (14): advantages are biocompatibility, color stabilization, and nonporous surface, which prevents plaque adherence better than composite resin. Disadvantages include requirement of skill, difficult to repair.
iv) Gingival prosthesis
SURGICAL APPROACHES for interdental papilla management include:
i) Papilla recontouring
ii) Papilla preservation
iii) Papilla reconstruction
NONSURGICAL methods include:
i) Correction of traumatic inter dental oral hygiene procedures
ii) Restorative procedures
iii) Orthodontic approach
iv) Prosthetic approach by means of Gingival prosthesis
A remarkably simple, yet affective procedure for the management of both gingival recession and loss of inter dental papilla is the use of gingival prosthesis.
GINGIVAL EPITHESIS: it is a removable mask or prosthesis that aesthetically and functionally camouflages lost gingival tissues.
Indications:
i) In inter dental defects with > 5 mm gap between contact point and alveolar crest
ii) When the patient cannot undergo repeated surgical procedures
Contra Indications:
i) Patients with poor or unstable periodontal health
ii) Poor oral hygiene
iii) Patients with high caries activity
Advantages:
I) Non-invasive
ii) Easy maintenance
iii) Slight splinting action on the teeth can be provided
iv) Economical
Disadvantages:
i) Poor patient compliance
ii) Food impaction and associated bacterial growth
iii) Chances of breakage or discoloration of the prosthesis
Various materials that can be used are:
i) Auto and heat polymerizing acrylic resins
a. Rigid
b. flexible
ii) Copolyamide
iii) Soft silicone materials
Advantages of using flexible materials over rigid materials are that they are more comfortable, easy to be made distal to canines, more retentive and less chances of breakage.
Advantages of rigid materials are that they are more resistant to staining, economical and more resistant to discoloration.
CASE REPORT 1:
A female patient, aged 48 years, came to GITAM Dental College and Hospital with chief complaint of gaps between her upper front teeth. On clinical examination it was noticed that generalized bleeding on probing and, periodontal pockets of around 3 to 5 m.m. were present in addition there were black triangles present between the maxillary anterior teeth due to loss of interdental tissues. The diagnosis was chronic generalized periodontitis and the patient was treated by means of conventional periodontal flap surgery.
On 6 months post-operative recall it was noticed that there were reduced bleeding scores, improvement in the clinical attachment levels and reduced probing depths. But still there were noticeable amount of gaps between her teeth resulting in an unpleasant smile. She was not willing for any more surgical procedures and hence a gingival prosthesis was planned.
Procedure:
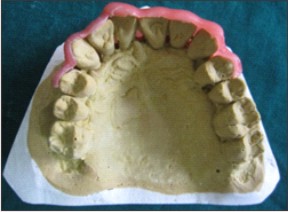
A preliminary impression of the maxillary arch (fig.3) was made using irreversible hydrocolloid impression material (algitex, DPI, India) and was poured in type III dental stone (dentstone, neelkanths healthcare products, India).
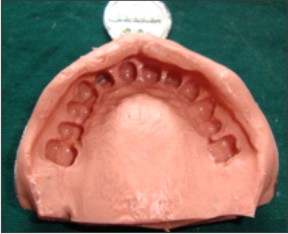 | Fig 3
 |
Over the preliminary cast two sheet thickness of modelling wax spacer was placed from first premolar to opposite first premolar such that it extends from the depth of the vestibule apically, onto the incisal surfaces incisally (fig.4). Three relief stops were given one anteriorly on the incisal edge of central incisor, two on both the occlusal surfaces of the first premolars (fig.5) acting as vertical stops during placement of the special tray. A special tray was then fabricated using an autopolymerizing acrylic resin covering the wax spacer, with a handle extending from the centre of the tray (fig.6) and the tray was checked in the patients mouth for proper placement and removal.
 | Fig 4
 |
 | Fig 5
 |
 | Fig 6
 |
A palatal stop was made (fig.7) of the palatal portions of the maxillary teeth intraorally by using a polyvinyl siloxane putty material (Aquasil, Dentsply, Germany). The putty palatal stop was removed from patients mouth after the material set and the interdental extensions of the putty stop were trimmed (fig.8) such that 3/4th of the labio-palatal interdental areas would be recorded by the final impression material.
 | Fig 7
 |
 | Fig 8
 |
Polyether impression material (Impregum, 3M, Germany) was chosen as the final impression material as it would not chemically combine with the putty index and hence easy to separate from the palatal putty stop, improved tear strength, improved accuracy and improved rigidity over other elastomeric impression materials.
Just prior to final impression making the wax spacer was removed from the special tray and the tray was perforated (fig.10) for mechanical interlocking of the final impression material. The putty stop was placed in the mouth; tray adhesive was applied to the special tray, final impression material was mixed and loaded in the special tray and was impression was made (fig.11). After the material set special tray with final impression and the palatal stop were removed separately respectively.
 | Fig 9
 |
 | Fig 10
 |
 | Fig 11
 |
The impressions were reoriented extra orally and the impression was poured in type IV dental stone ( Diestone plaster, Neelkanth Healthcare products, India) (fig.12).
 | Fig 12
 |
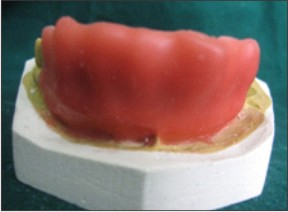
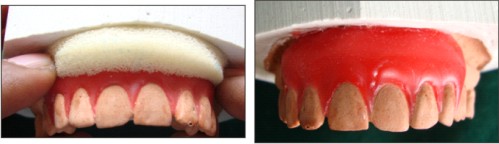
One layer of modelling wax (modelling wax, Hindustan, India) was made into wax pattern of the desired shape and contours of the prosthesis and it was properly carved, stippling was done by using a course sponge (16) (fig.14)
Flasking, dewaxing and acrylization were done in usual manner by using high impact heat cure denture base resin material (lucitone). The prosthesis was properly trimmed, polished and was inserted in the patient's mouth(fig.15). On 1 week and 1 month post insertion recall the patient was very much satisfied with the results and expressed her satisfaction.
 | Fig 13
 |
 | Fig 14
 |
 | Fig 15
 |
Case Report 2:
A 40 year old female patient presented with chief complaint of mobility of her upper front teeth and gaps between the teeth. On clinical examination it was noticed that around 5 mm periodontal pockets, Grade II mobility of the maxillary anterior teeth and generalized gingival recession with slightly malposed maxillary anterior teeth (Mahajan's classIII gingival recession defect). The patient was diagnosed as a chronic periodontitis patient and was treated with full mouth periodontal flap surgery. After 6 months recall similar prosthetic approach had been followed and a gingival epithesis was delivered to the patient (fig.16). The patient was quite satisfied with the aesthetic improvement achieved by using a gingival prosthesis
 | Fig 16
 |
Aftercare:
The prosthesis should be removed after food intake and should be thoroughly cleaned. It should not be worn during night times. It should be kept in denture cleaning solution whenever not in use and should never be left outside the moistened environment as it may cause distortion. Brushing the prosthesis helps prevent the appliance from becoming permanently stained. It's best to use a brush that is designed for cleaning dentures. A regular, soft-bristled toothbrush is also acceptable. Avoid using a brush with hard bristles, which can damage the prosthesis.
Discussion:
Gingival prosthesis is of considerable importance, especially in patients whose systemic health makes them unsuitable for repeated surgical treatments and who desire improved aesthetics following surgical treatment. It is a non-invasive, simple, economical treatment option with easy maintenance subsequent to insertion. Prostheses made of newer materials such as silicones (Gingivamoll, Detax, Germany) and flexible denture base materials are more advantageous as they are flexible enough to engage the undercuts and to be retentive without any harmful forces on the involved teeth. Poor patient compliance due to its removable nature, chances of discoloration (mainly with flexible materials), breakage and retention problems (mainly with rigid materials) are the drawbacks of the gingival prosthesis treatment.
Conclusion:
Gingival prosthesis is of great importance in masking soft tissue defects thereby improving esthetics and phonetics of the patients with recessed periodontal tissues. It is non-invasive; easy to maintain, with a slight splinting action on the teeth and is also an economical mode of treatment. In the case reports presented here, the gingival prosthesis masked the black triangles between the maxillary anterior teeth and improved the aesthetics of the patient significantly. Hence gingival prosthetic mode of treatment should be considered as a dependable treatment option.
References:
1. The Glossary of prosthodontic terms. J Prosthet Dent 2005;94:57
2. Carranza's Clinical Periodontology, 10th Edition
3. Nordland W.P. and Tarnow DP. A classification system for loss of papillary height. J Periodontol 1998;69:1124-1126
4. Sullivan H.C. and Atkins J.H.: Free autogenous gingival grafts. III. Utilization O Grats In The Treatment Of Gingival Recession, Periodontics, vol. 6:152, 1968.
5. Mlinek A, Smukler H, Buchner A. The use of free gingival grafts for the coverage of denuded roots. J Periodontol 1973;44:248-54.
6. Liu WJ, Solt CW. A surgical procedure for the treatment of localized gingival recession in conjunction with root surface citric acid conditioning. J Periodontol 1980;51:505-509.
7. Benque E.P., Brunel G., Gineste M., Colin L., Duffort J., Fonvielle E. Gingival recession. Parodontol J 1984; 3: 207-241
8. Miller PD Jr. A classification of marginal tissue recession. Int J Periodontics Restorative Dent. 1985;5:8-13.
9. Ajay Mahajan. Mahajan's Modification of the Miller's Classification for Gingival Recession. Dental hypothesis, Vol 1, No 2, 2010
10. Ajay Mahajan. Periosteal pedicle graft for the treatment of gingival recession defects: a novel technique. Australian Dental Journal 2009, Vol: 54, Issue: 3, Pages: 250-254.
11. Giovan Paolo Pini Prato, Roberto Rotando, Pierpaolo Cortellini, Carlo Tinti, Robert Azzi. Interdental Papilla Management: A Review And Classification Of The Therapeutic Approaches. International journal of periodontics and restorative dentistry, Vol. 24, No. 3, 2004
12. Arvind Shetty , Rasika Jagtap: Periodontics a part of cosmetic makeover. Scientific Journal, vol. 1, 2007.
13. Alternative method of conservative aesthetic treatment for gingival recession. J Prosthet Dent 1997; 77:561-3
14. An alternative treatment approach to gingival recession: gingiva-colored partial porcelain veneers: A clinical report. J Prosthet Dent 2007; 98: 82-84
15. The use of porcelain laminate veneers and a removable gingival prosthesis for a periodontally compromised patient: A clinical report. J Prosthet Dent 2005; 93: 315-7
16. Achieving predictable gingival stippling in labial flanges of gingival veneers and complete dentures. J Prosthet Dent 2007;97:118. |