Dentistry has entered an era in which patients no longer need to accept in which their candidacy for tooth must be dismissed because of insufficient alveolar bone volume, height, or width.
Bays (1986), Mecall and Rosenfeld (1991) concluded that tooth extraction, either traumatic or atraumatic, results in alveolar bone loss, both in width and height. According to Sevor and Meffert (1992), Grunder et al. (1999) an average of 40% to 60% of original height and width is expected to be lost after tooth extraction, with the greatest loss happening within the first year. This can negatively influence bone volume that is needed for future dental implant placement as well as proper ideal esthetic restoration.
The bone volume in the maxillary and mandibular alveolar ridges in buccolingual and apicocoronal directions influences a variety of factors related to oral health and potential restorative treatment, including the location and position of implants when placed, their subsequent success or failure, and the esthetics of the definitive restorations. 1,2,3
When dental treatment involves restoration of an extracted tooth, preservation and/or augmentation of the alveolar ridge dimensions is of paramount importance. The most predictable way to maintain the width, height, and position of the alveolar ridges is preservation at the time of tooth extraction.2, . Preserving the alveolar ridges at the time of tooth extraction helps to minimize difficulties during subsequent implant placement.2 A site planned for implant placement requires sufficient bone height and width to ensure stability and ideal soft-tissue contours.3 The minimum amount of bone recommended on the buccal or lingual aspects is 1 mm, with at least 2 mm of facial bone required for implants in the esthetic zone.3,6
One of the more difficult problems arises when it is essential or preferable to place an implant to the site of an existing compromised tooth. Central to such cases is the question of how best to manage the residual defects often associated with the extraction of periodontally hopeless teeth and to place implants successfully at those sites. A complicating factor is the need to maintain functional and esthetic hormony with adjacent natural teeth.Recent advancements in barrier membranes, bone grafting substitutes, and surgical techniques haveled to a predictable arsenal of treatment methods for clinicians to preserve or augment alveolar ridge postextraction.
Extraction socket maintenance for future implant therapy does not rule out immediate implant placement but rather provides an additional option when treatment planning implant patients.
When treatment planning for the extraction of one single-rooted tooth and subsequent implant placement, many pieces of information are needed to decide on the route of action.
The task for restoring anterior esthetics for implant therapy is demanding and requires a more rigorous treatment protocol . First, certain clinical parameters/criteria must be investigated to determine whether the case is acceptable for implant therapy.12
These criteria include but are not limited to:
-
mesiodistal space available for implant placement
-
buccolingual space available for implant placement
-
interarch space available (for potential implantsupported crown)
-
smile line (high, equigingival, or low)
-
gingival biotype (thick, average, or thin)
-
whether the case is a distal-extension situation, or whether teeth are present mesial and distal to the site of treatment
-
opposing dentition (natural teeth or a denture)
-
occlusion
-
presence of parafunctional habits, and
-
general medical and local surgical concerns.
If it is decided that implant placement will be delayed13 (not performed at the time of extraction or within 6 weeks of extraction), then it is prudent to take steps to maintain the alveolar bone dimensions to whatever extent possible.
Today there is still a dichotomy of thought regarding the timing of extraction and implant placement and according to literature no single method is a panacea rather there are specific clinical indications for each .
All of these materials or some combination thereof have demonstrated clinical efficacy for site preservation, augmentation, and implant integration at the affected site.The aim of this report is to highlight the use of specific regenerative materials and techniques to preserve the alveolar ridge after tooth extraction and/or augment the bone to accommodate anticipated implant and restorative requirements.
Case Report
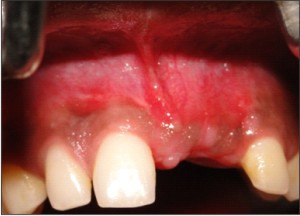
A 25 year old male presented with the chief complaint of discoloured , malaligned , extruded and rotated tooth no 21 . his dental history revealed an avulsion of tooth no 21 due to a road side accident 5 years back . Avulsed tooth was replanted after endodontic treatment. Patient is otherwise healthy with no relevant medical history . On clinical examination following relevant points were noticed . (Figure1 )
 | Figure 1: Labial View showing extruded, malalligned ,rotated 21
 |
-
Midline diastemma
-
High frenal attachment
-
Traumatic bite
-
Malalligned , extruded tooth no 21
-
Pocket approximately 5mm
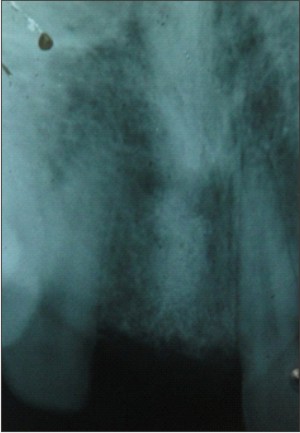
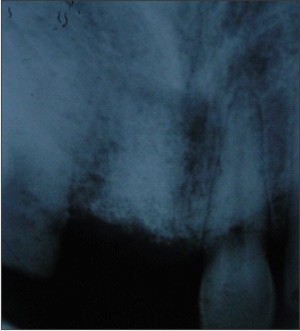
Radiographic examination (Figure 2) revealed a root that was misaligned with periapical radiolucency associated with external apical root resorption .
 | Figure 2 : Iopa Periapical Pathology and resorption around 21
 |
Patient was referred to Department of Orthodontics for consultation . Due to endodontic failure of tooth no.21 and poor bone support the prognosis of tooth was said to be hopeless and it was destined for extraction.
Simple extraction of the root at this stage could cause extreme resorption of soft and hard tissue components of ridge as well as a resulting functional and aesthetic defect . Therefore the patient was referred to Department of Periodontics and Oral Implantology for further treatment . The challenge was to prevent additional damage to the area and develop an effective treatment plan to reconstruct the hard and soft tissue .
Treatment Plan
The objective of treatment plan was to replace the central incisor with an implant supported crown restoration without interfering with the integrity and topography of adjacent gingival tissues. In order to develop an adequate implant site , the tooth was planned for extraction followed by socket augmentation procedure by guide bone regeneration
Technique
Local anesthetic was administered .
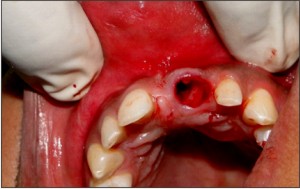
After local anesthesia was achieved the sulcular incisions was performed with a 15 scalpel to rupture the supracrestal attachment apparatus. Periotomes were then applied to severe the subcrestal attachment apparatus. Straight periotomes were used as it was single-rooted teeth.(Figure3 )
 | Figure 3: Extraction of 21 with Periotome
 |
The instrument was used first to complete rupture of the gingival fibers at the cervical area of the tooth. During this procedure, the long axis ofthe blade was angled converging at approximately 20° from the tooth long axis. This maneuver ensured that the tip of the periotome blade was located within the crest of the alveolar bone only, thus preventing the blade from sliding out of the ridge and lacerating the gingiva. The blade was thrust to the depth of the gingival sulcus and the gingival attachment was severed circumferentially. procedure was repeated again to ensure that all gingival fibers were severed. The instrument was then inserted into the periodontal ligament space and moved repeatedly in a mesiodistal direction, on the whole circumference of the root, severing the periodontal ligament immediately below the alveolar crest.
The periotome was then pushed further down into the periodontal ligament toward the root apex. Tooth was then extracted.
Following tooth removal(Figure 4), sharp curettage was carried out to remove remnants of periodontal ligament as well as any soft tissues such as peri-radicular cysts. These tissues may harbor pathogenic bacteria that may lead to postoperative complications. After debridement, socket was evaluated . On evaluation defect on buccal plate and palatal perforation was revealed . .(Figure 5 & 6)
 | Figure 4 : Extracted tooth showing the resorption on mesial aspect of root
 |
 | Figure 5 : Inspection of Socket after Extraction
 |
 | Figure 6 : Removal Of Granulation tissue with bone curette
 |
Then perforation of the socket cortical plate (decortication) was done as it is helpful in establishing blood supply to the graft from the adjacent bone. This was achieved by by scraping the walls of the socket with either curettes or rotary instruments. This procedure triggers the regional acceleratory phenomena (RAP), which is known to stimulate new bone formation and graft incorporation..
Mucoperiosteal flap was then raised and inspection site was again.(Figure 7)
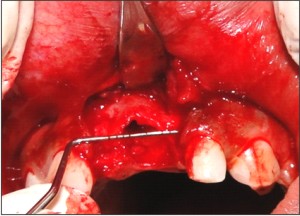 | Figure 7 : Evaluation of buccal wall defect after raising mucoperiosteal flap
 |
A section of membrane material ( Proguide ) was then cut to fit over the site, extending 3 to 4 mm beyond the socket margins onto sound host bone. Then with the help of vicryl suture, sling was made so that membrane could fit over the extracted site with tenting effect.(Figure 8)
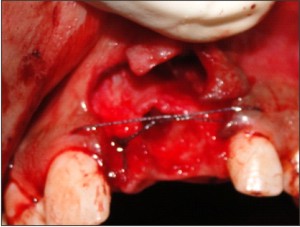 | Figure 8 : Vicryl suture holding opposite papillae to give tenting effect
 |
The bone graft material was then inserted into the extraction socket to provide a stable osteoinductive/ osteoconductive environment during the healing process.The graft material was moistened with sterile saline to form a cohesive paste that could be delivered to the extraction site. Using a periosteal elevator, the material was delivered to the extraction site and was packed gently to the apex of the site.
The membrane was trimmed to maintain a 1.0 mm margin from adjacent tooth roots to facilitate reattachment of the papilla to the interdental bone.(Figure 9 )
 | Figure 9 : Putting Gtr membrane inside the socket to cover palatal wall defect
 |
The subperiosteal dissection of the flap was extended to achieve a passive and stable fit of the membrane directly over the bone.(Figure10)
 | Figure 10 : A pplication of membrane over the buccal wall defect after bone graft is inserted
 |
Suturing were accomplished with interrupted sutures((Vicrylt, Ethicon Inc, Somerville, NJ).
Excessive tension on the flaps was avoided to maximize blood flow within the flap and avoid necrosis of the flap margins.
Follow Up
Postoperatively the patient was instructed to rinse with a 0.2% chlorhexidine solution and to avoid mechanical plaque removal over the operated site for 2 weeks(Figure11). Sutures were removed 2 weeks after surgery, and patients was reviewed monthly .
 | Figure 11 : Post operative labial view
 |
Results
Healing progressed uneventfully. No adverse tissue reactions were noted. Epithelialization occurred approximately 2 weeks postoperatively. According to radiographic analysis complete bone fill was predictably noted after 6 months (Figure 12,13,14,15) and fixture installation could be performed anytime according to the standard protocol.
 | Figure 12 : At Baseline (1 week)
 |
 | Figure 13 : Iopa (After 2 months)
 |
 | Figure 14 : Labial view (After 6 months)
 |
 | Figure 15 : Iopa (After 6 months)
 |
Conclusion
Myriad regenerative products (eg, bone allografts, cancellous bone, bioactive modifiers, PRGF, fibrin membranes) in combination with careful treatment strategies are helping to change the face of implant and restorative dentistry and contributing to more predictable long-term results. Given the propensity for the alveolar ridges to resorb after tooth extraction and/or as a result of atrophy, it behooves clinicians to understand the benefits and elements of socket and bone preservation/augmentation techniques and the materials that can be used for these purposes to enhance the ultimate outcome of implant placement and subsequent restorative treatment
Bibliography
1. Drakos D, Engler-Hamm D. Ridge preservation: why and when. Implants. 2006;3:20-23.
2. Levine RA, Horowitz RA. Bone reconstructive surgery for implant site preparation. Functional Esthetics & Restorative Dentistry.2007;Series 1 (No. 2): 20-28; a supplement to Inside Dentistry, 2007, Vol. 3 (No. 7).
3. Sonick M, Hwang D. Tooth extraction—an opportunity for site preservation. Contemp Esthetics. 2007 Feb;11(2):36-41.
4. Petrungaro PS, Amar S. Localized ridge augmentation with allogenic block grafts prior to implant placement: case reports and histologic evaluations. Implant Dent. 2005;14:139-148.
5. Schropp L, Wenzel A, Kostopoulos L, et al. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent. 2003;23:313-323.
6. Spray JR, Black CG, Morris HF, et al. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol. 2000;5:119-128.
7. Iasella JM, Greenwell H, Miller RL, et al. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans. J Periodontol. 2003;74:990-999.
8. Nevins M, Camelo M, De Paoli S, et al. A study of the fate of the buccal wall of extraction sockets of teeth with prominent roots. Int J Periodontics Restorative Dent. 2006;26:19-29.
9. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19 (Suppl):43-61.
10. Wang HL, Cooke J. Periodontal regeneration techniques for treatment of periodontal diseases. Dent Clin North Am. 2005; 49:637-659, vii.
11. Block MS, Degen M. Horizontal ridge augmentation using human mineralized particulate bone: preliminary results. J Oral Maxillofac Surg. 2004;62 (9 Suppl 2):67-72.
12. Tassos Irinakis, , Moe Tabesh. Preserving the socket dimensions with bone grafting in single sites: an esthetic surgical approach when planning delayed implant placement. J Oral Implantol .2007; 33:156-63
13. Mayfield LJA. Immediate, delayed and late submerged and transmucosal implants. In: Lindhe J, ed. Proceedings of the 3rd European Workshop on Periodontology: Implant Dentistry. Berlin: Quintessence; 1999:520–534. |