|
|
|
| Central Giant Cell Granuloma Of The Jaws - A Rare Case Report |
Divyalakshmi.M.R. 1 , K.S. Nagesh 2 , Asha R. Iyengar 3 , Reshma V.J. 4
1 Assistant Professor, Department of Oral Medicine and Radiology - D.A.P.M.R.V. Dental College and Hospital, Bangalore
2 MDS Principal, Professor and HoD - DAPM R.V Dental College, Bangalore.
3 Professor, Department of Oral Medicine and Radiology - DAPM R.V Dental College, Bangalore.
4 Post Graduate Student, Department of Oral Medicine and Radiology - D.A.P.M.R.V. Dental College and Hospital, Bangalore
|
| Address For Correspondence |
Dr. DIVYALAKSHMI.M.R., Assistant Professor
Department of Oral Medicine and Radiology
D.A.P.M.R.V. Dental College and Hospital, Bangalore
Karnataka, India
E-mail: divsmr@gmail.com
Ph No: 91-9611285858, 91-8022445754
Fax No; 080-26658411 |
| Abstract |
| Individuals affected by ectodermal dysplasia syndromes have abnormalities of the glands, tooth buds, hair follicles, and nail development. In addition to these, ectodermal dysplasia causes anodontia and hypodontia intraorally. Partial or total anodontia results in some loss of function, such as chewing, and affects aesthetics. Prosthodontic rehabilitation can be accomplished with fixed, overdenture, complete, or implant-retained prostheses. For rehabilitation, it is crucial to know the age, number and condition of present teeth, and the state of growth of the patient. A 13-year-old male patient who visited our clinic was treated by a multi-disciplinary team of surgeons, orthodontists, and prosthodontists. An overdenture was planned, and an implant-supported prosthesis was considered for when the patient had finished growing. A tooth supported overdenture was planned for prosthetic rehabilitation after considering his growth and the number and condition of his present teeth. |
|
| Keywords |
| Ectodermal dysplasia, anodontia, overdenture |
|
| Full Text |
Introduction
Central giant cell granuloma (CGCG) is an uncommon benign intraosseous lesion that occurs almost exclusively in the jaws, introduced for the first time by Jaffé in 1953. The World Health Organization has defined CGCG as a localized benign but sometimes aggressive osteolytic proliferation consisting of fibrous tissue with haemorrhage and haemosiderin deposits, with presence of osteoclast-like giant cells and reactive bone formation1. More than 60% of cases occur in children and individuals under 30 years of age2. The lesions occur more commonly in the mandible than in the maxilla with a ratio of 3:1 being reported3. Lesions are more common in the anterior region of the jaws, and mandibular lesions frequently cross the midline. The clinical behaviour of CGCG varies from a slowly asymptomatic swelling to an aggressive lesion that manifests with pain, root resorption and cortical perforation.
Case Report
A 21 year old female patient presented with a swelling with respect to the left lower third of the face since 8 months which was initially smaller in size and gradually increased to the present size. History revealed that the swelling was not associated with pain and there were no secondary features present. There was no history of any trauma to that region. The patient had not taken any treatment for the same. There was no relevant medical and dental history reported.
On extra oral examination a gross asymmetry of the face was seen which was due to a diffuse swelling measuring about 5 x 2 cms with respect to the left lower third of the face. The swelling extended mesiodistally from the midline to 1 cm from the angle of the mouth and superoinferiorly from the angle of the mouth to the lower border of mandible. There was no local rise in temperature and the skin over the swelling appeared normal with no evidence of sinus, discharge or visible pulsations. On palpation the swelling was non tender and bony hard in consistency with no secondary changes appreciated. There was no paraesthesia present with respect to that region.
On intraoral examination there was buccal cortical plate expansion extending from mesial aspect of left lateral incisor to the distal aspect of left first molar causing obliteration of the vestibule in that region. The gingiva and the overlying mucosa appeared normal. There was no gross swelling present in relation to the labial mucosa . The region was non tender and bony hard on palpation. Hard tissue examination revealed no abnormality and none of the teeth were tender, displaced or mobile. Pulp vitality test was carried out for the mandibular left quadrant, which revealed left first premolar to be non vital and the other teeth showed variable response.
Based on patient history and thorough clinical examination a provisional diagnosis of a benign odontogenic tumor with respect to mandibular left posterior region was arrived upon. The differential diagnosis of ameloblastoma, central giant cell granuloma, calcifying epithelial odontogenic tumor and aneurysmal bone cyst were considered.
Routine haematological investigations showed values within the normal limits. The various radiological investigations carried out were conventional panoramic radiograph, lateral oblique view of body of the mandible and Computed Tomography. Panoramic radiograph revealed a diffuse radiolucency measuring 1.5 x1 cm extending from the periapical region of mandibular left canine to mandibular left first molar with root resorption in relation to mandibular left second premolar (Figure 1) . Computed tomography with 3D reconstruction showed a diffuse hypointense area extending from the alveolar process with respect to the left premolar region encroaching to the inferior cortical border of the mandible (Figure 2).
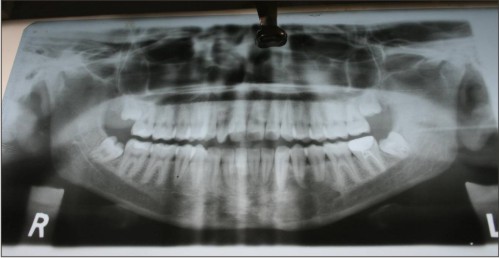 | Picture 1 - Panoramic Radiograph Showing Diffuse Radiolucency In The Periapical Region Of 33,34,35,36
 |
 | Picture 2 - Ct Showing Diffuse Hypointense Area In The Left Premolar Region Encroaching The Inferior Cortical Border Of Mandible
 |
An excisional biopsy and thorough curettage was carried out from the mandibular left premolar - molar region under local anesthesia and extraction of left central incisor to left first molar were done. (Figure 3). Histopathological examination revealed fragments of bone with attached cellular lesion composed of diffusely arranged polygonal cells with round nucleus and multinucleated giant cell seen scattered in the stromal cells with the diagnosis of central giant cell granuloma of the mandible.
 | Picture 3 - Image Showing Surgical Excision Of The Lesion
 |
Four dental implants were successfully placed and loaded, and an implant-supported prosthesis was constructed, providing a satisfactory dental restoration. The patient is currently under follow up at regular intervals.
Discussion
Central giant cell granuloma is a relatively common lesion of the jaws that is generally thought to be reactive rather than neoplastic in nature4. The etiopathogenesis of the CGCG of jaw bones has not been clearly established but it has been suggested that it is the result of an exacerbated reparative process related to previous trauma and intraosseous haemorrhage that trig-gers the reactive granulomatous process5. Central giant cell granuloma has been classified based on the clinical and radiographic features into4 :-
1. Aggressive lesion:Characterized by rapid growth, pain, expansion and / or proliferation of the cortical bone, root resorption and high recurrence rate.
2. Non-aggressive lesion: Characterized by slow growth that does not perforate the cortical bone or induce root resorption and has low recurrence rate.
The recurrence rate varies between 13-49% 6. Studies have reported a mean interval between diagnosis and initial treatment and stated that very few recurrences were manifested after 2 years of initial treatment. The various features correlating to an increased risk of recurrence are clinical activity of the lesion (72% of recurrence in the aggressive forms, 3% of recurrence in the nonaggressive forms), young age group, perforation of cortical bone and tumor size.
Cental Giant Cell Granuloma is considered as a non reparative lesion that grows if untreated. Conventional management of central giant cell granuloma include surgery with aggressive curettage. More aggressive and recurrent lesions require resection, leading to major deformity of the jaws thus causing facial disfigurement. Hence various non-surgical approaches have been indicated which include administration of intralesional corticosteroids 7, calcitonin therapy 8 and use of alpha interferon therapy.
Conclusion
Central giant cell granuloma is a rare entity of the head and neck region. Though a benign tumor, Central giant cell granuloma may be a locally destructive lesion in some cases and if left untreated may cause facial disfigurement thus compromising the quality of life of the individual.
References
1. Krameri R,Pindborg JJ and Shear M:Histologic typing of odontogenic tumors.2nd Ed.Berlin.Spinger Verlag,1991:31
2. Carlos R and Sedano H:Intralesional corticosteroids as an alternative treatment for central giant cell granuloma.Oral Surg Oral Med Oral Pathol Oral Radiol Endod.2002;93:161-6.
3. Kaffe I , Ardekian L,Taicher S: Radiographic features of central giant cell granuloma of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.1996;81:720-6
4. Hegde R.J Central Giant Cell Granuloma in a child:A case Report.J Indian Soc Ped Prev Dent September 2004 22(3).
5. Pedro Infante Cossío ,Rafael Martínez de Fuentes , Andrés Carranza Carranza , Daniel Torres Lagares , José Luis Gutierrez Pérez: Recurrent central giant cell granuloma in the mandible: Surgical treatment and dental implant restoration. Med Oral Patol Oral Cir Bucal 2007;12:E229-32.
6. de Lange J, van den Akker HP, Klip H. Incidence and disease-free survival after surgical therapy of central giant cell granulomas of the jaw in the Netherlands. Head Neck 2004;26:792-5.
7. Khafif A, Krempl G, Medina JE. Treatment of giant cell granuloma of the maxilla with intralesional injection of steroids. Head Neck 2000;22:822-5.
8. Pogrel M A. Calcitonin therapy for central giant cell granuloma. J Oral Maxillofac Surg 2003;61:649-53. |
|
|
|
|
|
|