Introduction
Peripheral Ossifying fibroma (POF) is a solitary, non-neoplastic gingival growth which usually arises as a reactive response to local irritation such as trauma, microorganisms, plaque, calculus, restorations and dental appliances. POF commonly arises from the interdental papillae and thought to arise from the periodontal ligament.1
Clinically POFs are sessile or pedunculated, usually ulcerated and erythematous or exhibit a colour similar to the surrounding gingiva. Although being reported to reach more than 6 cm, they are usually less than 1.5 cm in diameter, and the diagnosis can be made by clinical inspection and biopsy.2 Some authors have called it fibrous epulis, calcifying fibroblastic granuloma, or peripheral fibroma with calcification. Histologically, it is a non-encapsulated mass of cellular connective tissue with randomly distributed calcifications and/or mature bone.3 Most lesions are <2cm in size, although larger lesions occasionally occur. Furthermore, the lesions have female predilection and recurrence rate is considered high for benign reactive proliferation and it probably occurs due to incomplete initial removal, repeated injury, or persistence of the local irritants.4,5 POF can occur at any age range but exhibit a peak incidence between the second and third decades, but few cases occurring in children have also been reported. In vast majority of the cases, there is no apparent underlying bone involvement visible on a roentgenogram. However on rare occasions, there does appear to be superficial erosion of bone.5 Clinical findings alone are not sufficient for diagnosis of POF because there are other conditions that may have similar clinical appearances and clinical courses such as irritation fibroma, pyogenic granuloma or PGCG. Therefore biopsy and histologic examination is required for definitive diagnosis.6
Basically, the lesion presents varying stages of fibroma with ossification as the name POF implies. However, ossification and calcification may not be evident in all the cases, particularly in early cases of lesion growth. After elimination of local etiological factors like plaque, calculus, ill-fitting dentures and poor quality restoration, local surgical excision is the preferred treatment. Excision should include the periodontal ligament and periosteum at the base of the lesion in order to reduce the chance of recurrence.6 The lesion may recur after excision and in fact repeated recurrences are not uncommon. In the series of Cundiff, 16% of cases recurred, while in a series of 50 cases reported by Eversole & Rovin7, the recurrence rate was 20%.
Case Report
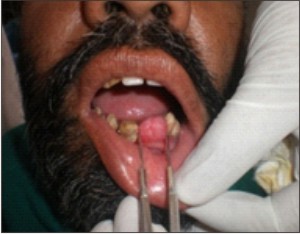
A 45 year old male patient reported to the Department of Periodontics with a chief complaint of growth and swelling in the anterior edentulous region of the lower arch since 1 year which had gradually increased in size. There was no associated pain or pus discharge although there was some mild bleeding associated with brushing. History revealed that patient had a similar growth about 4-5 years back, though smaller in size, in the same region (teeth were present at that time) i.e. interdental region of the front teeth which he got excised from local dentist. Lesion recurred about 1 year back which increased in size gradually and the adjacent teeth got exfoliated about two months back. On intraoral examination, the single dome shaped growth measuring approximately 1.5 cm mesiodistally and 2 cm buccolingually over the residual alveolar ridge starting anteriorly over the labial alveolar mucosa going over the alveolar ridge to end posteriorly over the lingual alveolar mucosa and extending distally upto the attached gingiva of lower left lateral incisor was observed ( Fig - 1, 2).
 | Fig 1. Photograph showing the mesio-distal dimension of the lesion.
 |
 | Fig 2. Photograph showing the vertical dimension of the lesion.
 |
It was non-tender, sessile and was firm to hard in consistency and the colour of the lesion was pale pink in colour with no ulceration.
Radiograph revealed only soft tissue shadow and no radiological signs of involvement of alveolar ridge were observed. The oral hygiene status of the patient was very poor with no associated habits. Based on the above clinical findings a differential diagnosis of irritation fibroma, pyogenic granuloma, peripheral gaint cell granuloma or a peripheral ossifying fibroma was considered.
After a routine blood examination, a thorough oral prophylaxis was done and under local anaesthesia excisional biopsy was done using both a scalpel and an electrocautery device under antibiotic coverage (Fig - 3).
 | Fig 3. Photograph showing the involved area after the complete excision of the lesion.
 |
Thorough curettage of adjacent periodontal ligament and periosteum was carried out to prevent recurrence. Adjacent teeth were scaled to remove any local irritants and the excised tissue was sent for histopathological examination.
Histopathologic Examination
The tissue (Fig - 4) was submitted to the oral pathology division for histopathologic diagnosis. The H&E stained section of the submitted tissue showed hyperplastic parakeratinised epithelium with normal elongation. The rete ridges were elongated with forking effect. The stromal connective tissue was fibrocellular, showing interlacing collagen fibres along with varying amounts of vascularity. The stromal tissue was also showing metaplastic component with empty lacunae. The mineralized component was round to oval in shape and appeared basophilic. Discrete amount of chronic inflammatory cells were also seen. The overall features were suggestive of Peripheral Ossifying Fibroma.(Fig - 5, 6, 7)
 | Fig 4. Photograph showing the excised mass to be sent for histopathological examination.
 |
 | Fig 5. Histopathological picture showing elongated rete ridges with forking effect.
 |
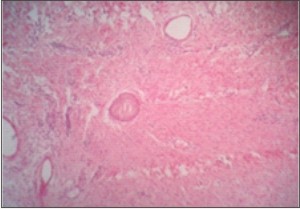 | Fig 6. Histopathological picture showing the fibrocellular connective tissue stroma and metaplastic component with empty lacunae.
 |
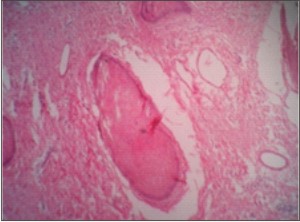 | Fig 7. Enlarged view showing the mineralized component (round to oval in shape).
 |
Discussion
POF is a relatively uncommon, solitary, non-neoplastic gingival growth, coined by Eversole and Rovin.1,7 Confusion has prevailed in the nomenclature of POF with various synonyms being used, such as peripheral cementifying fibroma, ossifying fibro epithelial polyp, peripheral fibroma with calcification, peripheral fibroma with osteogenesis, peripheral fibroma with cementogenesis, calcifying or ossifying fibrous epulis and calcifying fibroblastic granuloma.
The etiopathogenesis of POF is uncertain, though an origin from the cells of periodontal ligament has been suggested.2 The reasons attributed for origin from periodontal ligament include exclusive occurrence of peripheral ossifying fibroma in the gingiva, the proximity of gingiva to the periodontal ligament and the presence of oxytalan fibers within the mineralized matrix of some lesions.
The widely accepted etiopathogenesis for POF is the inflammatory hyperplasia of the cells of the periosteum or periodontal ligament as there is excessive proliferation of mature fibrous connective tissue in response to gingival injury, gingival irritation, subgingival calculus or a foreign body in the gingival sulcus. Chronic irritation of the periosteal and periodontal membrane causes metaplasia of the connective tissue and resultant initiation of formation of bone or dystrophic calcification.8
Clinically POF arises as a solitary nodular mass, either pedunculated or sessile and tend to arise from the interdental papillae. Multicentric POF can also occur in the oral and maxillofacial region, and have been observed in conditions associated with known genetic mutations, such as, nevoid basal cell carcinoma syndrome, multiple endocrine neoplasia type II, neurofibromatosis and Gardner syndrome.
Radiographically the features of POF tend to vary. Foci of calcifications have been reported to be scattered in the central area of the lesion, but not all lesions demonstrate.8 Underlying bone involvement is usually not visible on a radiograph but in rare instances, superficial erosion of bone can be seen.
Microscopically the features of POF consist of
1) intact or ulcerated stratified squamous surface epithelium;
2) fibrous connective tissue with varying numbers of fibroblasts;
3) sparse to profuse endothelial proliferation;
4) mineralized material consisting of mature, lamellar or woven osteoid, cementum – like material, or dystrophic calcifications;
5) chronic inflammatory cells in the lesion .
Athough peripheral giant cell granuloma (PGCG) clinically resembles POF,the latter lacks the purplish or bluish discolouration associated with PGCG and radiographically show small specks of calcification. The diagnosis of PGCG was ruled out on the basis that lesion lacked extravasated red blood cells and deposits of haemosiderin.9 Abundant haemorrhage is characteristically found throughout the lesion of PGCG whereas the biopsy showed metaplastic component with empty lacunae with mineralized component which appeared basophilic, a feature suggestive of Peripheral Ossifying Fibroma.
The diagnosis of pyogenic granuloma was ruled out on the basis that the lesion of pyogenic granuloma presents as soft friable mass which bleeds on minimal manipulation and histological picture lacked profuse endothelial proliferation characteristic of pyogenic granuloma and moreover and the mineralised component was also evident in the lesion more suggestive of POF.
The treatment of choice was surgical excision and as POF had a fairly high recurrence rate. If surgical intervention in an early stage is not done, POF can become large, causing extensive destruction of adjacent bone and significant functional or esthetic alterations.10 So, the mass should be excised deep into the periosteum with complete removal of all irritants which was performed in this case. The recovery was uneventful and the patient had remained tumour-free for 6 months. Although the POF is a benign reactive lesion, the recurrence rate is fairly high. Therefore, the patient is still on regular follow up.
References
1. Yadav R, Gulati A. Peripheral ossifying fibroma : a case report. J Oral Sci 2009;51:151-4.
2. Moon WJ, Choi SY, Chung EC, Kwon KH, Chae SW. Peripheral ossifying fibroma in the oral cavity: CT and MR findings. Dentomaxillofac Radiol 2007;36(3):180–2.
3. Satish BNVS, Kumar P. Peripheral Ossifying Fibroma of Hard Palate – A Case Report. International Journal of Dental Clinics 2010:2 (2): 30-34
4. Walters JD, Will JK, Hatfield RD, Cacchilo DA. Excision and repair of Peripheral ossifying fibroma; A report of 3 cases. J Periodontol 2001;72:939-44.
5. Das UM, Azher U. Peripheral Ossifying Fibroma. J Indian Soc Pedod Prev Dent 2009; 27: 49-51.
6. Kumar SK, Ram S, Jorgensen MG, Shuler CF, Sedghizadeh PP. Multicentric peripheral ossifying fibroma. J Oral Science 2006; 48(4); 239-43.
7. Eversole LR, Rovin S. Reactive lesions of the gingiva. J Oral Pathol 1972;1(1):30–8.[ref. J Indian Soc Pedod Prev Dent; 27: 49-51]
8. Terry Farquhar et al, Peripheral Ossifying fibroma: A Case Report; JCDA 2008; 74(9); 809-12
9. Falaschini S, Ciavarella D, Mazzanti R, Di Cosola M, Turco M, Escudero N, Bascones A, Lo Muzio L. Peripheral giant cell granuloma:immunohistochemical analysis of different markers. Study of three cases Av.Odontoestomatol 2007; 23 (4): 189-196.
10. Bodner L, Dayan D. Growth potential of Peripheral ossifying fibroma. J Clin Periodontol 1987;14:551-4. |