|
|
|
| Dental Orthopedic Appliance For Nasoalveolar Molding Of Unilateral Cleft Palate - A Clinical Report |
Lakshya Kumar 1 , Sunit Kr. Jurel 2 , Khurshid A. Mattoo 3 , Durga Shanker Gupta 4 , Akanksha Yadav 5
1 Lecturer, Department of Prosthodontics - Faculty of Dental Sciences (Upgraded KGMC), Lucknow
2 MDS, Lecturer Department of Prosthodontics, Faculty of Dental Sciences - C.S.M. Medical University (upgraded K.G.M.C.), Lucknow, Uttar Pradesh, India
3 Professor, Department of Prosthodontics - Subharti Dental College, Meerut, Uttar Pradesh
4 MDS (Oral and Maxillofacial Surgery) Assistant Professor Department Of Oral and Maxillofacial Surgery - Teerthanker Mahaveer Dental College and Research Center, Moradabad (U.P)
5 - Practitioner
|
| Address For Correspondence |
Dr. Sunit Kumar Jurel
C/O Er. R.B.Singh, 18/373,
Indira Nagar, Lucknow (UP).
Phone : +919453604322, +918853725087
E-mail: dentistmj1110@yahoo.co.in |
| Abstract |
| This article describes fabrication of an appliance that is to be used as a presurgical management of a patient with cleft palate. The molding of the affected complex is carried out in two stages, first is the alveolar molding which is carried out by the oral plate, that is retained extraorally and the second stage involves fabrication of a nasal stent which molds the nasal complex and also reduces the pressure on the nasal cartilage by removing the force, that is exerted as a result of drooping of the tissues. The appliance, after wearing, approximated the cleft segments close together which minimized the extent and the number of surgeries. |
|
| Keywords |
| unilateral cleft palate, oral plate, nasal stent, nasoalveolar molding. |
|
| Full Text |
Introduction
In a surgical correction of a unilateral or bilateral cleft lip and palate, it is ideal that prior to surgery, deficient tissues should be expanded and malpositioned structures should be repositioned. This provides a foundation for a less invasive surgical repair. Use of presurgical infant orthopedic (PSIO) appliances or molding palate therapy has aided significantly in reducing the size of the clefts. Since its introduction by Mc neil in 1950, various techniques for molding the intra oral alveolar segments closer together have been described.1, 2.
Pre-surgical nasoalveolar molding includes not only the reduction in the size of the intraalveolar cleft; but also the active molding and positioning of the surrounding soft tissues affected by the cleft, including the deformed soft tissue and cartilage in the cleft nose. This is accomplished through the use of a nasal stent, which is based on the labial flange of a conventional oral molding plate and enters the nasal aperture. The stent provides support and gives shape to the nasal dome and alar cartilages. Pre - surgical nasoalveolar molding should be employed in early management of cleft anomaly. Close coordination between pre - surgical management and surgery greatly improves upon the results which are overall improvement in esthetics of nasolabial complex, minimize extent of surgery and overall number of surgical procedures.
Clinical Case Report
A male baby, aged 8 months, had to undergo a surgery for his cleft palate by the team of doctors which included prosthodontists. The role of a prosthodontist was to develop an appliance that would perform nasoalveolar molding. Oral examination of the child revealed a unilateral cleft palate on the left side of the maxilla. The patient was clinically evaluated by all the members of the interdisciplinary cleft palate team including the prosthodontist. The patient was examined for the presence of any unusual undercuts or tissue abnormalities. The treatment plan included presurgical nasolabial molding to be accomplished by an oral plate and a nasal stent followed by the surgery.
The primary impression was made using a high viscosity elastomeric impression material. A special tray was fabricated using self cure acrylic. The final impression was made again with heavy body addition silicone, with the infant fully awake, face held down. The impression material registered all the border regions of the maxilla and premaxilla so as to get maximum tissue coverage for retention (Fig 1).
 | Fig.1 : The Defect
 |
From this impression two casts were poured, one as the working cast upon which the intra oral molding plate would be fabricated while the second cast would remain as a permanent record. The defect on the cast was now filled with wax to approximate the contour and topography of an intact arch prior to the fabrication of the oral portion of the molding appliance. Following this a two layer base plate wax was adapted which was later processed with heat cure acrylic resin.
At the delivery appointment, the oral molding appliance was carefully fitted in the patient’s oral cavity. After initially inserting the oral molding appliance, the baby was observed for several minutes while the clinician stabilized the appliance against the palate. This was done to ensure infants ability to easily suckle without gagging or struggling.
The tissue surface of the appliance was also modified to begin the initial molding of the greater and lesser alveolar segments on either side of the cleft. This was achieved through the selective removal of acrylic from the region into which one desires the alveolar bone to move. At the same time a soft liner (permasoft) was added to line the appliance to a thickness of approximately 1- 1.5 mm in the region from which the bone was to be reduced or moved.
After this, an external retentive button was developed with self cure acrylic resin on the oral plate. This retentive button serves to facilitate both the positive seating of the appliance to the palatal tissues and to secure the retentive bands extraorally.
The goal of the intra oral molding therapy should be to have the gingival tissues contact on either side of the ridge although a successful surgical result may be obtained even when a small cleft (1 -2mm) remains between the alveolar ridges.
Fabrication Of A Nasal Stent
Once the oral molding plate was fastened and used by the patient till cleft gap was reduced to approximately 6 mms (which took about a month of wearing the oral molding plate), the next step was carried which was to fabricate a nasal stent which will serve as a custom tissue expander that slowly corrects the flattening of the cleft lip nasal deformity. The nasal stent is a projection of acrylic that is formed by the careful addition of small amounts of cold cure acrylic resin until the stent was positioned inside the nasal dome on the cleft side of the nose (Fig 2).
 | Fig.2 : Impression Making
 |
The nasal stent was then trimmed by 1-2 mm from all sides, and is lined by a soft liner (permasoft).The appliance was modified and adapted at each subsequent visit by adding and removal of the soft liner.
The goal of nasal orthopedics during the later appointments was to ensure that while the lip segments are drawn together, the columella was repositioned to a midline location. The shape of the nostril and alar rim was also carefully molded to resemble the configuration of the unaffected side.
The appliance was now ready to carry nasal molding (Fig. 3 and Fig 4).
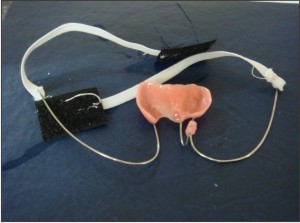 | Fig.3 : Prosthesis (Tissue Surface View)
 |
 | Fig.4 : Prosthesis In Place
 |
Instructions And Maintainence
The patient’s parents were instructed that the appliance should be worn continuously by the infant up to the time of the surgery and that it has to be removed at the operating room only. A weekly basis, follow-up protocol was given and at each appointment the progress was monitored. The retention of the appliance and the effectiveness of the taping done by the parents, were also regularly monitored.
Discussion
The retentive button was positioned facing downward on the labial flange at a 45 0 angle relative to the occlusal plane, thus allowing clearance for the upper and lower lips. The length of the two retentive buttons should not hamper mother from feeding the baby as the device needed to be worn continuously to be effective.
The fabrication of the nasal stent was done by making impression of the unaffected nostril using putty impression material. The procedure determined the actual thickness of the nasal stent. The orientation of the nasal stent was such that the nasal tip and dome on the cleft side were projecting outward and towards the cleft side. This served as a custom tissue expander that slowly corrected the flattening of the cleft lip nasal deformity. It also served to bring the columella into a more midline position. As nasal stenting progressed each week the nasal tip and dome on the cleft side began to appear more symmetric when compared with the non cleft side when the stent was in place.
The nasal stent also exerted a reciprocal intraoral molding force against the alveolar segments. As the nasal tissues pushed against the nasal stent this force was transmitted down along the nasal stent and provided additional force that aided in reducing the dimension of the intraoral defect. After the first wearing of nasal stent, the position of the nostrils changed as the alveolus was lifted, so it became important that during subsequent visits the nasal stent thickness was increased on one side (superiorly) and reduced on the other side (inferiorly). This was accomplished easily by using a soft liner than a self cure acrylic resin.
Summary And Conclusion
The nasoalveolar molding provided a safe, effective and lasting improvement in the esthetics of the nasolabial complex in the patient with unilateral cleft palate. The extent of surgery was minimized as all the tissue that was occupying the cleft before nasoalveolar molding was repositioned to its original position. Moreover nasal cartilage deformity was prevented by removing the forces that was exerted by drooping tissues.
References
1. Latham R. Orthodontic advancement of the cleft maxillary segment: A preliminary report. Cleft Palate J 1980; 17:227.
2. Mylin W. The pin retained prosthesis in cleft palate orthodontics. Cleft Palate J 1968:5:219.
3. Cutting C. Cleft lip nasal construction. In: Rees TD, LaTrenta GS (cds). Aesthetic Plastic Surgery, Vol 1. Second edition, Philadelphia; Saunders, 1994:497
4. McComb H. Primary correction of the unilateral cleft lip nasal deformity: A 10 year review. Plast Reconstr Surg 1985;75:791
5. McNeil C. Orthodontic procedures in the treatment of congenital cleft palate. Dent Rec 1950; 70:126.
6. Salyer K. Primary correction of the unilateral cleft lip nose: A 15 year experience. Plastic Reconstr Surg 1986; 77:558.
7. Santiago P, Grayson B, Gianoutsos M, Kwon S, Brecht L, Cutting C. Reduced need for alveolar bone grafting by pre-surgical orthopedics and primary gingivoperiostioplasty. Cleft Palate Craniofac J 1998; 35:77. |
|
|
|
|
|
|