Introduction
Arthroscopy was first described by Takagi in 1939.In 1975 Ohnishi demonstrated the use of this technique in the TMJ. Murakami and colleagues (1984) described the scientific and clinical considerations of TMJ arthroscopy. Holmlund and Helsing, using cadaver specimens, described their soft tissue landmarks for location of the puncture sites. The first report of diagnostic TMJ arthroscopy was also performed in 1975. Helsing also was the first to describe initial findings such as fibrillation of the temporal cartilage and articular disc. Arthroscopic examinations of the TMJ have generally been confined to the superior joint space. Inferolateral approaches to the inferior joint space have, however, been described. Numerous studies examined the diagnostic accuracy of arthroscopy by comparing the arthroscopic findings with follow-up surgical dissection results on cadavers and others correlated arthroscopic findings with histology and. The purpose of this article is to present a review of the literature on the relevant anatomy, indications, techniques, intra- and post-operative complications for diagnostic arthroscopy. Diagnostic accuracy is also presented as a part of this review of the literature.
Tmj Anatomy
The TMJ is a bilateral diarthrosis between the glenoid fossa and the condyle of the mandible. The connective tissue capsule is reinforced by the strong lateral temporomandibular ligament and a medial ligament, incomplete at the medioanterior half of the joint. The articular disk divides the joint into two non-communicating compartments. It is composed of fibrous connective tissue, although with advancing age ,it is not uncommon for areas to undergo hyalinization. It is biconcave in shape with a thin intermediate zone bounded by thicker anterior and posterior bands. It is attached to the articular capsule anteriorly, medially, and laterally. Posteriorly, it is anchored to the tympanic plate and the condyle by the retrodiscal tissue which is highly vascular and innervated loose areolar connective tissue. The joint extends posteriorly from the squamotympanic and petrotympanic fissures to the articular tubercle anteriorly.The articulating surfaces are covered with fibrocartilage. Synovium lines the joint cavities. During translation, the retrodiscal tissue expands within the glenoid fossa to occupy a greater volume as a result of the opening of numerous arteriovenous connections. Condyle-eminence contact at the intermediate-zone during function is believed to be partly responsible for coordinated condyle-disk movement.
Patient Selection
The indications2,4,5,6 include patients with signs and symptoms of intracapsular disorders such as disc displacement, hypomobility, osteoarthritis, arthritides, pseudotumors, post-traumatic complaints and synovitis with adhesive capsulitis; unresponsive for at least 3 months of conservative therapy are candidates for TMJ arthroscopy. Contraindications to arthroscopy are similar to those for other elective procedures such as any medical condition that places the patient at an increased risk from general anesthesia or the surgical procedure itself. Local contraindications include skin or ear infections, possible tumor seating, and severe or advanced fibrous ankylosis resulting in severe limitations and movement of the condyle. Emotional instability, obesity that prevents the joints from being palpated adequately are also considered contraindications.
Diagnostic Arthroscopic Equipment
The basic set of instruments used include telescopes(arthroscopes) mostly with a 2.0mm diameter (diameter range 1.7mm-2.7mm)but ultrathin telescopes with a 0.7mm diameter have also been developed1,a 30°rod-lens telescope with sheath and sharp and blunt trocars, fibre-optic or fluid light cable, automatic flash unit with halogen or xenon light source. Still photographic materials include a video camera, video recorder and video printer.
Arthroscopic Anatomy
Synovial pouches
Synovium appears arthroscopically as a soft, folded, translucent membrane interspersed with red capillary projections, and is bordered by the glenoid process on the posterosuperior edge, the superior lamina of the posterior ligament , and the posterior band on the posteroinferior side, the glenoid fossa on the superior boundary, the intermediate zone between the articulating surface of the disk and the articular eminence anteriorly , and the disk surface that lies anteroinferiorly. The anterior pouch of synovium is less folded. Its boundaries are the disc posteriorly and inferiorly, and the anterior slope of the articular eminence posteriorly and superiorly.
Glenoid Fossa
This structure appears as a rounded, concave area of bone. Occasionally, synovial lining with capillary projections can be identified in the glenoid fossa,
Articular Eminence
This appears arthroscopically as a rounded protuberance that is suspended from the superior wall of the joint space anteriorly and has a steep upward slope .This protuberance is covered with a layer of fibrocartilage that varies in texture and color depending on the amount of degeneration that has occurred. Normal fibrocartilage appears as a smooth surface that is white or blue-white in colour.
Intra-articular disc
The disc appears as a milky white structure with a smooth surface. Its interaction between the condyle and the articular eminence can be observed with mandibular motion. A distinct border of synovial tissue and the posterior and anterior disc attachments can be easily recognized.
(FIG.1.A,B)
 | Fig.1. Left Joint Under Normal Conditions, A. Upper Compartment: Posterior Disk Attachment, B. Posterior Band Of The Disk
 |
Condyle
It presents as a round, highly reflective area. The colour of the fibrocartilaginous covering of the condyle is pure white in normal unaffected joints.
Capsule
In the upper compartment, the anterior capsule is thin,, membrane-like. The anterior half of the medial capsule is also extremely thin and almost translucent. Posteriorly, the medial capsule, reinforced with fibrous tissue, serves as another important landmark during TMJ arthroscopy. In the lower compartment, the anterior capsule is extremely thin and directly overlies the upper belly of the lateral pterygoid muscle3.
Arthroscopic Procedure
Routine diagnostic arthroscopy can be performed under local anesthesia which can be combined with intravenous sedation, using a short acting benzodiazepine such as midazolam but in patients with markedly impaired TMJ mobility general anesthesia should be preferred. The patient is positioned, prepared and draped in the standard manner for TMJ surgery. Anatomic landmarks (zygomatic and condylar processes, articular eminence) are outlined with a sterile skin marker for placement of the irrigation and arthroscopic cannulas.
First, the upper compartment is distended with 2ml of lidocaine injection, slowly, until resistance is felt. Infero-lateral approach is used to gain good access to the posterior part of the upper compartment of the TMJ11. Other’s include the endaural and anterolateral approaches. Routine puncture of the lower compartment is avoided for only the posterior non-functional parts of the disk and condyle are visualized, and there is always atleast some risk of damaging the lateral disk attachment. Two entry points are marked, which are 10 mm and 15mm on the line, anterior to the posterior border of the tragus. A 18 gauge needle is used to puncture the skin at the more anterior point. The aim is to contact the zygomatic bone superiorly to the glenoid fossa, before slipping the needle downward into the superior joint space. A sharp trocar enclosed in a cannula is inserted at the posterior point from an infero-lateral approach towards the glenoid fossa(FIG.2).
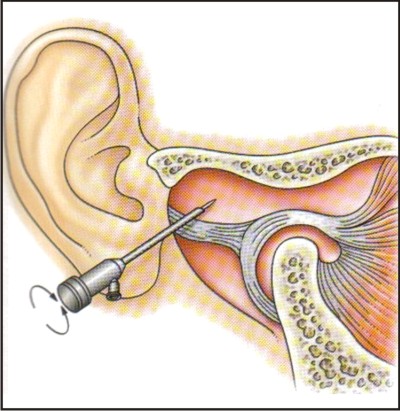 | Fig.2. Insertion Of A Sharp Trocar
 |
The sharp trocar is exchanged for a blunt one when the joint capsule is punctured. The trocar is then withdrawn and the arthroscope, connected to a camera attachment, is introduced through the cannula(FIG.3.).
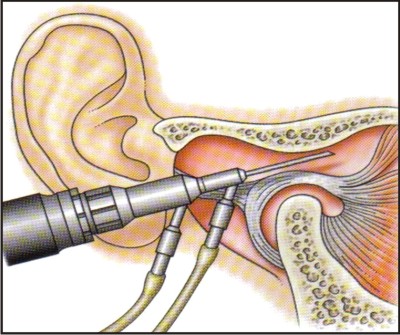 | Fig.3.Insertion Of The Arthroscope
 |
The superior joint surfaces should come into view on the colour TV monitor. The arthroscope is then used to slowly and systematically scan the space to assess the status of the joint structures.
Arthroscopic Examination
It begins with the identification of the arthroscopic landmarks - the boundary between the disk and the posterior disk attachment, the medial capsule, the inferior part of the eminence, and the anterior capsule.With the outflow being monitored continually, arthroscope is rotated slowly and examiner first identifies the posterior disk attachment as it is the predominant location for inflammation. Loss of the well-defined boundary between the posterior part of the disk and the posterior disk attachment indicates degenerative changes usually found in joints with chronic locking and osteoarthritis.
The arthroscope is then moved in a more medial direction to visualize the medial capsule. After withdrawing the arthroscope slightly, it is directed antero-medially and with the slight closure of mouth it slips under the eminence into the anterior recess. During withdrawal of the arthroscope, the temporal cartilage and disk surface should be evaluated (FIG.4).
 | Fig.4.Pronounced Fibrillation Of The Central Part Of The Disk
 |
Signs of osteoarthritis, such as fibrillation may be located mainly on the posterior slope of the eminence. Disk perforations are usually detected in the lateral, central, and posterior parts. In some cases, the lower compartment can be examined through a large disk perforation from the upper compartment.
The examination completes after thorough irrigation to remove any blood clots and suction of excess fluid through the arthroscopic sheath. The skin punctures are closed with surgical tape.
Complications
Intraoperative and postoperative complications are seldom associated with diagnostic arthroscopy, however, TMJ arthroscopy is associated with few complications1,3,7,4,5, as follows:
1. Vascular injury to the temporal vessels
2. Extravasation of the irrigation fluid causing extensive edema
3. Scuffing
4. Damage to middle ear
5. Broken instruments and
6. Infection
7. Irreversible changes in the articular tissues
These complications can be prevented by acquiring adequate knowledge of the joint anatomy, pre-operative radiographic examination, training on cadavers, proper handling of the instruments and using correct technique. Experience with open TMJ surgery facilitates the management of complications.
Accuracy Of Diagnostic Arthroscopy
The diagnostic accuracy of upper-compartment TMJ arthroscopy has been investigated in human cadaver(Holmlund and Hellsing, 1985; Liedberg and Westesson, 1986; Kurita etal., 1989; Bibber al, 1989) and in patient series (Goss et al., 1987; Holmlund, 1989). Liedberg and Westesson (1986) 10showed this method to have a low diagnostic sensitivity (ranging from 0.21 to 0.67) but a high diagnostic specificity (ranging from 0.93 to 1.00) when used to detect major morphological defects of the intracapsular tissues. This variation in sensitivity and specificity was related to that areaof thejoint being visualized. Calculated positive predictive values for these data were from 0.92 to 1.00, and the negative predictive values were from 0.52 to 0.77. On the other hand, Holmlund and Hellsing (1985) reported arthroscopy to have a high diagnostic accuracy for other disease processes (i.e.,100% accuracy for arthrosis and 57% for remodeling). Kurita et al. (1989) studied the diagnostic accuracy of TMJ arthroscopy at detecting TMJ adhesions and disk perforations. They found higher diagnostic accuracy values for the adhesions than for the perforations (1.00/1.00 vs. 0.96/0.76 in terms of positive/negative predictive values). Bibbet al. (1989) reported that the abnormal soft-tissue morphology discovered in subsequent dissection was not completely discovered by any of the imaging procedures, including tomography, arthrography, and arthroscopy. In a patient series, Goss et al. (1987) reported good agreement, with the exception of one case, between the findings derived from arthroscopy and thosefrom subsequent open surgical arthrotomy (as the "gold standard") in 12 TMJs. Holmlund (1989) also compared the intracapsular findings discovered during arthroscopy with those from open surgical arthrotomy in 28 consecutive joints from 21 patients. Holmlund (1989) calculated high diagnosticaccuracy for the detection of osteo-arthrosis (sensitivity,0.95, and specificity, 0.88), and for synovitis (sensitivity, 0.95, and specificity, 0.89) by arthroscopic visualization.. These early studies provided important initial information about the diagnostic value of arthroscopy, but they also had many drawbacks. For example, these studies utilized only small numbers of cadaver specimens of persons who were quite elderly at the time of their death. Several studies correlating arthroscopic findings with histologic3 and immunohistochemical findings in synovial biopsies show close agreement regarding inflammation.
Summary
Diagnostic TMJ arthroscopy has overcome most of the problems of plain radiography, tomography and arthrography. The very high resolution thin section CT scan and MRI are superior in showing a displaced disc but are limited by their expensive cost and inability to reveal intracapsular pathology. Thus, TMJ arthroscopy has come a long way becoming an important aid in the diagnosis of temporomandibular disorders(TMD) and thus has opened wide avenues in their management.
Refrences:
1. Applebaum EL, Berg LF, Kumar A, et al. Otologic complications following temporomandibular temporomandibular joint arthroscopy. Ann Otol Rhinol Laryngol1988; 97:675–9.
2. Amato J, Israel H. Temporomandibular Joint Arthroscopy in Asymptomatic Subjects: Preliminary findings. Columbia Dental Review 1999: 4:3-4.
3. F.R. Carls, A. Hochstetter , M. Makek and W. Engelke . Diagnostic accuracy of TMJ arthroscopy in correlation to histological findings . Journal of Cranio-Maxillofacial Surgery Volume 23, Issue 2, April 1995, Pages 75-80
4. Holumlund .Arthroscopy. In:Fonseca J.Raymond .Textbook of Oral and Maxillofacial surgery.W.B.Saunders,2000; Pages 255-275
5. Heffez L, Blaustein D. Diagnostic arthroscopy of the temporomandibular joint. Oral Surgery Oral Medicine Oral Pathology 1987; 64 : 653-70.
6. Holmlund A, Hellsing G. Arthroscopy of the temporomandibular joint. A comparative study of arthroscopic and tomographic findings. Int J Oral Maxillofac Surg 1988: 17: 128-33.
7. Holmlund A. Diagnostic TMJ arthroscopy. Oral Surg Oral Diagn. 1992;3: 13-8
8. Israel H. Arthroscopy of the temporomandibular joint. In: Peterson L, Indresano T, Marciani R, Roser S, editors. Principles of oral and maxillofacial surgery. Philadelphia: J.B. Lippincott, 1992 2015-40
9. Jeffrey J. Moses TMJ Arthroscopic Surgery—Current Concepts, Rationale, and Technique Journal of Oral and Maxillofacial Surgery, Volume 63, Issue 8, Supplement 1, August 2005, Pages 123-124.
10. Jonas Liedberg and Per-Lennart Westesson :Oral Surgery, Oral Medicine, Oral Pathology Volume 62, Issue 6, December 1986, Pages 618-624
11. Joseph P. McCain, Bruce Sanders, Michael G. Koslin, James D. Quinn, Philip B. Peters, A.Thomas Indresano. Temporomandibular joint arthroscopy: A 6-year multicenter retrospective study of 4,831 joints. Journal of Oral and Maxillofacial Surgery, Volume 50, Issue 9, September 1992, Pages 926-930
12. Murakami K, Ono T., Temporomandibularjoint arthroscopy by inferolateral approach. Int J Oral Maxillofac Surg 1986; 15: 410-417.
13. Murakami K and G.T. Clark .Diagnosis of Intracapsular Pathology Associated with Temporomandibular Joint Disorders Adv. Dent. Res. 1993; 7; 120
14. Douglas G. Nuelle. Caution with arthroscopic surgery Journal of Oral and Maxillofacial Surgery, Volume 45, Issue 5, May 1987, Page 382
15. Sanders B. Efficacy of temporomandibular joint arthroscopy: a retrospective study [Discussion]. J Oral Maxillofac Surg 1993; 51:17-21.
16. Sanders B. Arthroscopic management of internal derangements of the temporomandibular joint. Oral Maxillofac Surg Clin North Am 1994; 6:259-69.
17. Tarrow W. Allen. Arthroscopic Diagnosis and Surgery of the Temporomandibular joint.J Oral Maxillofac Surg; 1988;46:282-289.
18. T. Bjornland, M. Rorvik, H. R. Haances, J. Teige: Degenerative changes in thetemporomandibular joint after diagnostic arthroscopy. An experimental study in goats. Int. J. Oral Maxillofac. Surg. 1994; 23: 41-45. |