Introduction
The word ‘Ergonomics’ was derived from the Greek words: ‘Ergon’ which means work; and ‘nomos’ meaning natural laws. The very root of this comparatively young branch of science goes back to the early 1900s, but it appeared as an identifiable profession in late 1940 after world war –II. An insight into the accidents of bomber pilots of similar nature revealed a mismatch between cockpit design (controls and displays) and the limitation of the capabilities of the pilots. It was emphasized that in all working conditions, the human limits and capabilities should be studied prior to job or machine design. Thus ‘Ergonomics’ emerges as a technique that brings together several disciplines to solve problems arising from the incompatibility of man, machine and work environment. The international Labor Organization (ILO) defines ergonomics as ‘the application of human biological sciences in conjunction with the engineering sciences to achieve the optimal mutual adjustment of man and his work, the benefits being measured in terms of human efficiency and well being. In simpler terms, it can be defined as a science of fitting the physical, physiological and psychological requirement of a job to the capabilities of the workers with the goal of making the workplace more comfortable in order to improve health, safety and productivity. The principles of ergonomics touch all aspects of our life and can be applied in work place, at home and even in recreational and leisure activities.
Musculoskeletal Disorders (MSD)
According to World Health Organization about 58% of the world’s population over the age of 10 years spend one third of their time at work and about 30 – 50% of the workers are exposed to significant physical occupational hazards [1].
The manual exertions required for performing a task is one of the major areas of ergonomic consideration. This is often described in terms of cardio respiratory or musculoskeletal workload. As regards to the musculoskeletal workload, the work always brings with it an inevitable risk of mismatch between the mechanical capabilities of the worker and job demand in conjunction with improper work process, hand tool use and ambient conditions. Thus manual work often imposes strain on our musculoskeletal system that culminates into work related mechanical trauma often described as musculoskeletal disorders (MSD).
MSDs were recognized as having occupational etiologic factors as early as the beginning of the 18th century. Italian physician Brernardino Ramazinni in his famous publication, De Morbis Artificum (Diseases of worker) first pointed out a definite relation between the manual work and the strain imposed on the musculoskeletal systems of our body which result in work related injuries.
After 1970's various occupational factors leading to MSD were examined using epidemiologic methods, and the work-relatedness of these conditions began appearing regularly in different scientific literatures which indicated that there exists a strong and consistent relationship between work exposure and MSDs [2-5]. Today MSDs appear to be the most common cause of severe long term pain and physical disability and account for 23% of total cost of illness. It has been estimated that between 50 – 70% of workforce in developing countries is at a risk of developing musculoskeletal disorder owing to the various ergonomic risks factors present in their workplace [6] . Studies have shown that these disorders can affect any part of the body, but the most affected areas are low back [7] neck, shoulder, elbow and wrist [8]. The common signs and symptoms of MSD are presented in Table 1.
Table. 1 Signs and Symptoms of MSDs
Signs
-
Decreased range of motion
-
Loss of normal sensation
-
Decreased grip strength
-
Loss of normal movement
-
Loss of coordination
Some Symptoms of MSDs
-
Excessive fatigue in the shoulders and neck
-
Tingling, burning, or other pain in arms
-
Weak grip, cramping of hands
-
Numbness in fingers and hands
-
Clumsiness and dropping of objects
-
Hypersensitivity in hands and fingers
Cumulative Trauma Disorder (CTD) and Ergonomic risks factors
The modern era has observed a radical change in both office and industrial work environment. The advent of automation and mechanization has introduced a myriad of dexterous hand–intensive work processes. Although these work methods are not very arduous in nature but involve various ergonomic risks factors that contribute to different soft tissue injuries and disorders of the nerve, tendons, tendon sheaths and muscles of the upper extremities, which are collectively referred to as Repetitive Strain Injury - RSI or Cumulative Trauma Disorders- CTD [8, 9, 10]. Today this is considered as a new age health issue that is affecting millions worldwide.
A number of ergonomic risk factors are responsible for this kind of injuries and can also precipitate and aggravate the condition. These factors include repetition, awkward posture, force, static exertion, and contact stress. Table 2 provides a definition for these risks factors.
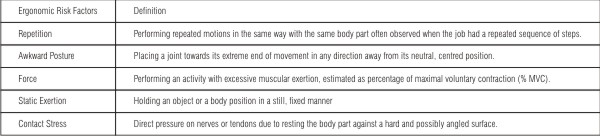 | Table 2. Definitions Of Various Workplace Risk Factors Contributing To CTS
 |
Prevalence of MSD’s among Dental Professionals
Like all other occupations, the dental profession is also burdened with occupational health problems and hazards of various kinds among which the musculoskeletal disorder is a major one [11].
Although modern dentistry although considered as a least hazardous occupation [12] but still the risks of musculoskeletal disorders in dental practice remains conspicuously high. In the last two decades a considerable interest has grown in ergonomics and work related musculoskeletal disorders associated with dental practice. The prevalence of musculoskeletal disorders among dentists and other dental professionals is manifested mainly as neck shoulder hand wrist pain (also classified as upper extremity musculoskeletal disorder) and low back pain.
Prevalence of Upper Extremity Musculoskeletal Disorder (UEMSD)
High rates of occurrence of UEMSD in dental professionals are well documented, including regional neck and shoulder pain, shoulder tendonitis, neuropathy, tension neck syndrome and trapezius myalgia and carpal tunnel syndrome [13-18] A recent updated review on the prevalence of for neck symptoms has reported a rate of varying between 17–73% for dentists, 54–83% for dental hygienists and 38–62% for dental assistants. For shoulder symptoms, ranges were 20–65% for dentists, 27–76% for dental hygienists and 62% for dental assistants [19].
Prevalence of low back pain
A persistence low back pain has been defined as a pain in the lower back occurring for most of the time during last 12 months [20]. This is also considered as the annual prevalence of low back pain. Literatures revealed that annual prevalence rates for low back pain are quite high in dental profession.
A self reported annual prevalence of LBP was found to be 50% and 55% for Danish and Israel dentist [21,22]. Similar reports of 54% prevalence of LBP were obtained for Australian (Queensland) [23] and Flemish dentists in Belgium [24]. However some higher rates of LBP of 64% and 74% was reported among dentists of New South Wales , Australia and Saudi Arabia respectively [25, 16]. A lower rate of 43% was reported among Hong Kong dentists [26].
Ergonomic risk factors in dental procedures.
In conjunction with the prevalence study of MSDs among the dentists, researches have also focused on ergonomic characterization of dentists work. These studies have revealed various ergonomic risks factors associated with dental procedures contributing to MSDs.
Awkward postures have been identified as the major etiologic factor for upper extremity musculoskeletal disorders. The range of awkward occupational postures may include pinch grips, wrists deviations, ulnar /radial bending forearm pronation/ supination, shoulder elevation / abduction, neck rotation and flexion. All these postures are associated with a variety of upper extremity CTDs [27] and are influenced by the interaction of many occupational and individual factors including work station layout, equipment and tool features and workers anthropometry [28].
Modern seated dentistry is more ergonomically designed than the old standing procedures. Research suggested that this transition from a standing to seated posture, has not reduced the prevalence rate of MSD [25] but part of body affected has moved from the lower back to the neck, shoulders, and arms [29].
The work of a dentist is conducted in a small 2/ 2½ inch workplace which represents the patient’s mouth. The work procedures are extremely precise and require steady hands and often require repeated or sustained muscular exertions with limited range of motion. Moreover, improper positioning of both patient and dental worker often increases the static work load and awkwardness of their postures particularly in relation to neck and shoulder conditions. There is a well -documented relationship that these types of work characteristics is a major etiologic factor for upper extremity musculoskeletal discomfort for dentists [30, 31]. Problems such as rotator cuff syndrome, tension neck syndrome (TNS), involving painful neck spasms and trigger points, have also been found to be associated dental hygiene work [31].
Observational studies on dental procedures have revealed a high frequency of neck bending [16] and neck flexion [21] during work period which was found to be well correlated occurrence of cervicobrachial disorders among the dentists [32]. Along with awkward head and neck postures the work also required to hold the upper arm to be elevated for a prolonged period of time. Studies have revealed that these create a high static muscle load in the neck and shoulder regions particularly in the trapezius [29] and supraspinatus muscle [21, 33].
Dental procedures are also visually demanding. Difficulties in direct visualization inside the mouth also cause awkward posture. Dentists often rotate their necks to the left with the side
bend to the right for better visibility. In a study it was noted that this is likely to strengthen the muscles on one side while weakening the opposing muscles, thus resulting in the inability to rotate the neck to the right with side bending to the left [32]. Similarly, the forward viewing posture frequently used by dental workers can lead to weakening of the stabilizer muscles of the shoulder blades, leading to rounded shoulder posture [29].
Studies have also indicated that handedness was a clear determinant of whether dentists left or right sided pain [18]. Forward leaning postures are also common in dentistry which was also found to be a significant contributor in increasing the neck and shoulder pain of dentists [34].
Various endodontic and surgical procedures require long time. Forceful clinical tasks such as scaling requires wrist flexion for grasping small vibrating tools in extremely awkward wrist postures with repetitive movements. These are identified as the causative occupational factors for carpal tunnel syndrome [10]. Various studies have corroborated these factors with the occurrence of carpal tunnel syndrome, median nerve dysfunction and reduced tactile perception among dentists [35 – 40].
Non - occupational risks factors
The prevalence of MSD among dental practitioners appeared to be multifactorial; with a significant contribution from various confounding variables that include demographic and psychosocial and anthropometric factors. Working hours, work habits, gender, perceived level of stress, experience and personal characteristics [15, 23, 25, 41-43] all are found to be associated with MSD. There are also studies which report a high association of MSD with less work satisfaction, poor quality of health and more anxiety among dentists [44,45]. Besides there are various pre existing medical conditions that can acts as potential non- occupational risks factors for CTD observed among dental practitioners.
Application of Ergonomic principles can help in reducing MSD
In spite of various positive epidemiological findings there is still an ongoing debate on the potentiality of various risk factors of dental procedures in causing MSD among dentists [46, 47]. These studies have indicated that establishing a relationship between the dental tasks and ergonomically related disorders remains speculative. Quantification of the exposure to ergonomic risk factors in dental practice appears to be the most important fact in order to gain a much detail insight on the potentiality of the dental procedures on the causation of MSD. Thus a need for more systematic ergonomic studies aiming at analyzing various dental tasks both qualitatively and quantitatively has been indicated.
Ergonomic studies have indicated that regular periodic rest periods and job rotation can be used effectively to reduce the incidence of CTD in different group of workers [48]. This can also be introduced in dental practices to reduce the overall job stain and occurrence of MSD among dental practitioners. Improvement of hand tool design is also effective in reducing the ergonomic risk factors for CTD [49]. Majority of the dental instruments are held in pinch grip. Therefore changing the handle design may offer an inexpensive opportunity for reducing hand wrist stress during dental practice [47].
Conclusion and Recommendation
Musculoskeletal disorders are high among dentists. Pain in low back, neck, shoulder , hand and wrist and some associated musculoskeletal disorders and injuries are a major health problem for dental practitioners. These disorders and injuries may result in absence from work for extended periods away from work that may decrease work performance, job satisfaction and can also increase anxiety and stress.
It seems that there is a wide scope of reducing various problems arising out of dental practices. Principles of design ergonomics can be applied for redesigning of work station and work tools to promote more neutral working postures. Well organized job rotation and tasks planning can be introduced to reduce the cumulative musculoskeletal stress that may appear from prolonged work exposure. Furthermore, dentists could be trained for increasing the awareness of various ergonomic issues. These sorts of training can encourage them in adapting micro breaks during their jobs and to practice some regime of flexibility and strengthening exercises. This can be a great help in reducing the overall burden of musculoskeletal work load among dentists.
In spite of a multitude of overseas literatures available on MSD among dentists, studies among Indian dentist on similar issues are conspicuously low. This may be due to the fact that Ergonomics as a subject is still not that popular and has been not added in regular curriculum of different Varsities. Therefore it seems natural that awareness about good ergonomic practices is lacking among general population and the dentists are also no exception. In this context it therefore appears that the Dental Council of India should take interest in ergonomic issues as these concepts are extremely important for dental offices. Initiative should also be taken to include the subject as a part of dental curriculum particularly in bachelor level. This will not only help to build ergonomic awareness among dental students but will also widen the scope of ergonomic research in the context of dental practices.
References
1. World Health Organization. Global strategy on occupational health for all. WHO. Geneva; 1995.
2. Hagberg m, Silverstien B, Wells R, Smith R, Hendrick H P et al, (Eds). Work related musculoskeletal disorders. In A handbook for prevention, London: Taylor and Francis; 1995.
3. Musculoskeletal disorders (MSDs) and workplace factors: a critical review of epidemiologic evidence for work-related musculoskeletal disorders of the neck, upper extremity, and low back. DHHS (NIOSH) Publication no. 97–141. Washington (DC): US Department of Health and Human Services, National Institute for Occupational Safety and Health; 1997. URL:http://hinarigw.who.int/whalecomwww.cdc.gov/whalecom0/niosh/ergosci1.html
4. Latko WA, Armstrong TJ, Franzblau A, Ulin SS, Werner RA, Albers JW. Cross-sectional study of the relationship between repetitive work and the prevalence of upper limb musculoskeletal disorders. Am J Ind Med 1999; 36: 248–59.
5. Evanoff BA. Work-related musculoskeletal disorders: examining the research base epidemiology: physical factors. In: Work-related musculoskeletal disorders. Report, workshop summary, and workshop papers. Washington (DC): National Academy Press; 1999. p. 152–4.
6. Jacobson & Lindgren. What costs illness? National Board of Welfare. Stockholm: Sweden; 1996.
7. Troup JDG, Edwards F. manual handling and lifting. An Introduction and literature review with special reference to the back. London: HMSO; 1985.
8. Armstrong TJ, Foulke JA, Joseph BS and Goldstein S. 1982. An investigation of cumulative trauma disorders in a poultry processing plant. American Indust Hygiene Assoc J; 43: 103 – 116.
9. Armstrong TJ. Ergonomics and cumulative trauma disorders. Hand Clinics. 1986; 2: 553 – 566.
10. Silverstein BA, Fine LJ, Armstrong TJ. Occupational factors and carpal tunnel syndrome. American Journal of industrial medicine, 1987; 11. 343- 358
11. Babich S and Burakoff RP. Occupational hazards of dentistry. A review of literature from 1990. N Y state dentistry J. 1997, 63: 26-31.
12. Scully C, Cawson RA, Griffiths M, Ch 1. Mortality and some aspects of morbidity . In : occupational hazards to Dental Staff. 1-21. British medical Journal, London; 1990.
13. J. Osborn, K. Newell, J. Rudney and J. Stoltenberg, Musculoskeletal pain among Minnesota dental hygienists, J Dent Hyg. 1990; 64: 79–85.
14. M. Atwood and C. Michalak, The occurrence of cumulative trauma in dental hygienists, Work: Am J of Prevention Assessment and Rehab 1992; 2: 17–31
15. I. Akesson, B. Johnsson, L. Rylander, U. Moritz and S. Skerfving, Musculoskeletal disorders among female dental personnel – clinical examination and a 5-year follow-up study of symptoms, Int Arch Occup Environ Health . 1999; 72: 395–403.
16. K.A. Al Wazzan, K. Almas, S.E. Al Shethri and M.Q. Al- Qahtani, Back & neck problems among dentists and dental auxiliaries. J Contemp Dent Prac. 2001; 2: 17–30.
17. Crawford, G. Gutierrez and P. Harber, Work environment and occupational health of dental hygienists: a qualitative assessment. J Occup Environ Med. 2005; 47: 623–32.
18. T.Yee, L. Crawford and P. Harber,Work environment of dental hygienists, J Occup Environ Med. 2005; 47: 633–39.
19. Morse T, Bruneau H, Dussetschleger J. Musculoskeletal disorders of the neck and shoulder in the dental professions. Work. 2010; 35: 419–429
20. Punnett L, Robins JM, Wegman DH, Keyserling WM. Soft tissue disorders in the upper limb of female garment workers. British J Indust Med 1985; 11: 417-425
21. L. Finsen, H. Christensen and M. Bakke, Musculoskeletal disorders among dentists and variation in dental work, Appl Ergon. 1988; 29(2), 119–125.
22. Ratzon NZ, Yaros T, Mizlik A, Kanner T. Musculoskeletal symptoms among dentists in relation to work posture. Work; 15: 153-8.
23. Leggat PA, Smith DR. Musculoskeletal disorders self-reported by dentists in Queensland, Australia. Aust Dent J. 2006; 51(4): 324-7.
24. Gijbels F, Jacobs R, Princen K, Nackaerts O, Debruyne F. Potential occupational health problems for dentists in Flanders, Belgium. Clin Oral Investig. 2006; 10: 8-16.
25. Marshall E.D., Duncombe L.M.,. Robinson R.Q and. Kilbreath S.L, Musculoskeletal symptoms in New South Wales dentists. Aust Dent J. 1997; 42: 240–6.
26. Ka T, Chin E, Ho A, Hung W, Lai J. Self reported occupation related health problems in Hong Kong Dentists. Hong Kong Dent J. 2006; 3: 39-44.
27. Armstrong TJ ergonomics and cumulative trauma disorders of hand and wrist in J M Hunter, LH Schneider, E J Mackin and A D Callahan (eds), Rehabilitation of the hand surgery and therapy 1990 (Philadelphia: the C.V. Mosby Co., Philadelphia RA: 1175-1191
28. Keyserling WM, Armstrong TJ, Punnett L. Ergonomic job analysis: a structured approach for identifying risk factors associated with overexertion injuries and disorders. Applied Occupational and Environmental Hygiene 1991; 6: 253 – 263
29. Valachi and K. Valachi, Mechanisms leading to musculoskeletal disorders in dentistry, J Am Dent Assoc. 2003; 134: 1344–1350.
30. L. Fine and B. Silverstein, Work-related disorders of the neck and upper extremity, in: Occupational Health, (Fourth ed.), B. Levy and D.Wegman, eds, Philadelphia: Lippincott Williams and Wilkins, 2000, pp. 515–535.
31. M. Sanders and C. Michalak-Turcotte, Preventing workrelated MSDs in dental hygienists, in: Ergonomics and the Management of Musculoskeletal Disorders, (2nd ed.), M. Sanders, ed., St. Louis, MO: Butterworth Heinemann, 2004, pp. 448–469.
32. B.L. Rundcrantz, B. Johnsson and U. Moritz, Occupational cervico-brachial disorders among dentists. Analysis of ergonomics and locomotor functions. Swed Dent J. 1991a; 15: 105–115.
33. T. Oberg and U. Oberg, Musculoskeletal complaints in dental hygiene: a survey study from a Swedish county, J Dent Hyg. 1993; 67: 257–261.
34. R.M. Barry, W.R.Woodall and J.M. Mahan, Postural changes in dental hygienists. Four-year longitudinal study, J Dent Hyg. 1992; 66: 147–150.
35. R. Lundstrom and A. Lindmark, Effects of local vibration on tactile perception in the hands of dentists, J Low Freq Noise Vib. 1982; 1: 1–11.
36. J.C. Conrad, K.J. Conrad and J.S. Osborn, Median nerve dysfunction evaluated during dental hygiene education and practice (1986–1989). J Dent Hyg. 1991 a; 65: 283–8.
37. J.C. Conrad, J.B. Osborn, K.J. Conrad and T.C. Jetzer. Peripheral nerve dysfunction in practicing dental hygienists, J Dent Hyg. 1991 b; 64: 382–7.
38. J.C. Conrad, K.J. Conrad and J.B. Osborn, Ashort-term, three year epidemiological study of median nerve sensitivity in practicing dental hygienists, J Dent Hyg. 1993; 67: 268–72.
39. J.A. Lalumandier and S.D. McPhee, Prevalence and risk factors of hand problems and carpal tunnel syndrome among dental hygienists. J Dent Hyg. 2001; 75: 130–4.
40. D. Anton, J. Rosencrance, L. Merlino and T. Cook, Prevalence of musculoskeletal symptoms and carpal tunnel syndrome among dental hygienists. Am Journal of Indust Med. 2002; 42: 248–257.
41. Jacobsen N, Aasenden R, Hensten – Pettersen A 1991. Occupational health complaints and adverse patient reactions as perceived by personnel in public dentistry. Community Dent Oral Epidemiol. 1991; 19: 155-9
42. Chowanadisai S, Kukiattrakoon B, Yapong B, Kedjarune U, Leggat PA. Occupational health problems of dentists in southern Thiland. Int Dent J. 2000; 50: 36-40
43. Alexopoulus EC, Staathi IC Charizani F. Prevalence of musculoskeletal disorders among dentists. BMC Musculosskeletal Disord. 2004; 5: 16
44. B.L. Rundcrantz, B. Johnsson and U. Roxendal Moritz U. Occupational cervico-brachial disorders among dentists. Psychossocial work environment, personal harmony and life satisfaction. Scand J Soc Med .1991 b; 19: 174-180
45. Lindfors P, Thiele UV Lundberg U. Work characteristics and upper extremity disorders in female dental health workers. J Occup Health. 2006;48: 192-197
46. Bramson JB, Smith S. Romagnoli G. Evaluating dental office ergonomics risk factors and hazards. JADA. 1998; 129: 174-83.
47. Guay AH. Commentary: Ergonomically related disorders in dental practice. JADA. 1998; 129: 184-6
48. Armstrong TJ, Lifshitz Y. Evaluation and design of jobs for control of cumulative trauma disorders. In: Industrial hygiene science series: Ergonomic interventions to prevent musculoskeletal injuries in industry. Chelsea, Mich.: Lewis; 1987:111-5.
49. Silverstein BA, Fine LJ, Armstrong TL. Carpal tunnel syndrome: causes and a preventive strategy. Seminars in Occupational Medicine. 1986; 1: 213-23 |