Introduction:
Distraction Osteogenesis, also called "callus distraction", "callotasis" & "osteo-distraction" is a relatively new technique for orthodontists and maxillofacial surgeons which have revolutionized the correction of major skeletal deficiencies. Distraction osteogenesis is the process of slow bone expansion in which new bone is generated in an osteotomy gap in response to tension stresses placed across the bone gap. Distraction osteogenesis has been used to avoid the problems associated with conventional surgery and to begin correction at an earlier age.
Distraction Osteogenesis is a biologic process of new bone formation between the surfaces of bone segments that are gradually separated by incremental traction. Specifically, this process is initiated when distraction forces are applied to the callus tissues that connect the divided bone segments, and continues as long as these tissues are stretched. The traction generates tension that stimulates new bone formation parallel to the vector of distraction. Importantly, distraction forces applied to bone also create tension in the surrounding soft tissues, initiating a sequence of adaptive changes termed distraction histogenesis. Under the influence of tensional stresses produced by gradual distraction, active histogenesis occurs in adjacent tissues, including gingiva, skin, fascia, muscle, cartilage, blood vessels, and peripheral nerves. These adaptive changes in the soft tissues allow larger skeletal movements while minimizing the potential relapse seen with acute orthopedic corrections.
History of distraction osteogenesis:
1905 - First bone distraction was performed by, for the treatment of shortened femur.
1927 - Lengthening of tibia was done by Abbott
1954 – Gravil Ilizarov11, a Russian orthopedic surgeon, began his work on the lower extremity using techniques that combined compression, tension & then repeated bone compression to heal fractured long bones with segmental defects. He pioneered the radical concept that bone generation could be reinitiated by the piezoelectric effect of tension, rather than compression. Ten to fifteen years later, he expanded his technique to include the treatment of shortened lower extremities.
1975 - Bell & Epker2 - Described a technique of rapid palatal expansion to increase the width of maxilla using a Haas appliance.
1976 - Michieli & Miotti - Reproduced Snyders work,using an Intra Oral device.
1989 - McCarthy et al - First human mandibular distraction. Remmler et al described experimental fronto-facial advancement with Distraction Osteogenesis technique in animals.
1993 - Fast midface distraction with buried devices was performed. Steven.R.Cohen Buried midface distraction on a child with Anopthalmia & Left cranio- facial microsomia.
1994 & Early 1995 - First case of Multi- directional midface distraction.
1997 - Chin & Toth4- Lefort III advancement with gradual distraction using internal devices.
1999 - Polley & Figueroa1- Discussed the management of severe maxillary deficiency in childhood & adolescence performing Distraction Osteogenesis with an external adjustable, rigid distraction device.
Indications:
Cranio-racial microsomia (unilateral / bilateral).
Niger's syndrome.
Treacher Collins syndrome.
Aperts syndrome,
Ctouzon's syndrome.
Pierre Robin syndrome.
TMJ ankylosis.
Hypoplasia of the maxilla and mandible.
Post traumatic growth disturbances.
Regeneration of mandibular condyle.
Distraction of mandibular symphysis to correct anterior crowding.
Post traumatic deformity (midfacial retrusion or mandibular collapse).
Atrophy of edentulous segments.
Oncologic mandible defects.
Contraindications:
Several factors can limit or preclude the use of distraction osteogenesis (DO) to correct craniofacial deformities. Few absolute contraindications to the use of this technique exist. However, caution is advised in patients who, for one reason or another, will not comply with the distraction regime. From a surgical standpoint, an adequate bone stock is necessary to accept the distraction appliances and to provide suitable opposing surfaces capable of generating a healing callus. Therefore, in patients who have undergone several craniofacial procedures in the past, the facial skeleton may exist in several small discontinuous fragments unsuitable for distraction. In these cases, bone grafting the gaps first may be possible, followed by distraction on a delayed basis.
Advantages:
-
No need of autogenous bone grafting.
-
Gradual distraction of not only the hard tissues but of the soft tissues also.
-
Multi-directional expansion of the face.
-
Skeleton in all three planes of space.
-
Ease to open & close the mouth & ease of mastication.
-
Reduced length of hospitalization & operating time.
-
Effective when applied at a younger age group.
-
Good stable results.
Disadvantages:
A number of problems can arise with the distraction process (e.g. patient non fusion of the segments undergoing distraction). These problems necessitate a repeated surgical procedure to re-osteotomize the bone segments. Infection at the distraction site may impair the osteogenesis process. During the consoli¬dation phase, non-union or delayed union results if micromovement across the segment occurs. Excessive scarring is also possible, particularly when using external devices. Finally, there is a relative lack of control in repositioning the bone segments when compared with conventional surgery, which leads to less than ideal final position. Cutaneous scarring resulting from transcutaneous fixation pins. Appliances are bulky and need patient compliance.
How Does It Work????
The underlying principle of Distraction Osteogenesis, as described by
Ilizarov, is "the mechanical induction of new bone between bony surfaces that are gradually distracted." The process of Distraction Osteogenesis begins with careful preoperative assessment and planning, which are critical to success. At the initial surgery, osteotomies are performed and the distraction device is inserted. A waiting period (latency phase) is allowed to elapse during which bone healing is initiated’ at the bony gap. In this early period, periosteal integrity is restored and callus formation begins12, 13 & 14. The bone segments at either end of the gap are then progressively distracted over a period of several days (distraction phase) during which osteogenesis is induced, thus producing a so-called "regenerate of immature bone" is laid down between the cut bone ends. Over time, the bone remodels into a more mature state (con¬solidation phase), and the surrounding soft tissues adapt to their new positions arid lengths The histology and physiologic principles underlying Distraction Osteogenesis have been well documented in long bones and, more recently, in the craniofacial skeleton. During the distraction phase, when a bone heals, collagen fibres first grow in the blood clot between the broken ends of the bone, forming a web. Then, mineralization, or ossification, of the bone occurs, causing hardening of the collagen web. Distra¬ction osteogenesis is possible because as the collagen fibres begin to harden, the fibrous layer is able to stretch and widen so as older fibres covert into bone, the newer fibres are able to stretch if tension is gradually applied to the broken bone. Bone remodeling begins during the consolidation phase and continues over 1-2 years, eventually transforming the regenerate into a mature osseous structure similar in size and shape to the adjacent bone. In addition to bony changes, effects on the adjacent soft tissue occur in response to osseous distraction. Muscle and soft tissue mass increase via a process referred to as "distraction histogenesis". Clinically, this offers a distinct advantage because several craniofacial anomalies have soft tissue hypoplasia in addition to deficient bony structures. Neurovascular elements contained within distracted bony segments are also stimulated regenerate.
Diagnosis & Treatment Planning:
Pre-operative clinical evaluation is similar to the examination carried out in preparation for orthognathic or cranio¬facial surgery. Note the forehead, orbital, zygomatic, external ear position & contour of the chin; inferior border & angle of the mandible. Functional clinical examination should include mandibular excursions & TMJ function. Nerve functions are also examined. All patients require careful clinical assessment and photographic documentation of their condition. Frontal and lateral cephalograms and a mandibular Panorex view are obtained in virtually all patients. Three-dimensional CT scanning is also useful.
The role of orthodontics in treatment using DISTRACTION OSTEOGENESIS falls in three temporal phases:
Predistraction treatment planning & orthodontic preparation
Orthodontic / orthopedic therapy during distraction & consolidation
Post consolidation orthodontic / orthopedic management.
Pre-distraction treatment planning:
This begins with careful appraisal of the dentition. Dental mal-relations must be eliminated that would mechanically interfere with the movement of the tooth bearing segment during distraction. Fabrication & use of distraction stabili¬zation appliances which facilitate vector control during distraction & maintain transverse maxillo-mandibular relationship during distraction.
Indications for these appliances are
For patients who do not require specific tooth movement before distraction.
Are not in full orthodontic bands or brackets.
Are very young & non-compliant.
Maximum segment anchorage.
Distraction stabilization appliances consist of banded maxillary expansion appliance & a mandibular lingual holding arch attached to two bands on either sides.
Orthodontic treatment during distraction & consolidation:
Active orthodontics may continue throughout the treatment which may include use of bands & brackets, elastics, head gear, acrylic guidance appliances, etc. Interarch elastic traction applied during distraction has shown to influence the vectors of distraction in the vertical, Antero-posterior & transverse directions. The most important use of elastic traction during distraction is to prevent Latero-gnathism (frequently seen in the unilateral distraction of the mandible).
Orthodontic therapy after distraction & consolidation:
After distraction the appliance is removed. The postdistraction orthodontic needs depend on whether the mandibular distraction was unilateral or bilateral. In non-growing bilateral distraction patient, orthodontic finishing is completed at this time. In unilateral distraction patient, it mostly involves occlusal plane management, correction of dental midlines, correction of maxillo-mandibular disharmony. Orthodontic treatment of the growing children may consider future distraction or orthognathic surgery.
Biological forces:
The biological force (arising from the surrounding neuromuscular envelope) & mechanical force (under the clinician’s control) that shape the regenerate are key elements in determining the appliance position. The desired change in shape & function can be achieved by selecting & controlling the force vectors (vertical, horizontal or oblique).
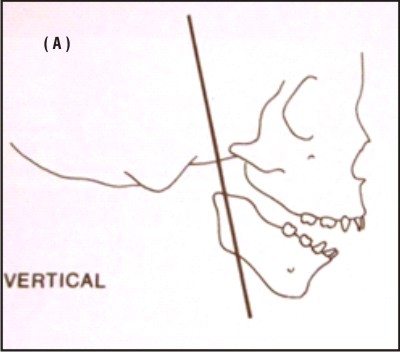 | Fig-2 Orientation Of Device In Different Plane Of Action
 |
Device placement can be described as vertical, horizontal or oblique (FIG-2)
Vertical device placement causes an increase in the vertical dimension of the mandibular ramus. The mandible auto rotates in a counterclockwise direction & the lower incisors take a more advanced position & a posterior open bite may result Horizontal device placement causes sagittal advancement of the mandible. The mandible rotates in a clockwise direction resulting in an openbite & the gonial angle opens. Oblique device placement results in an increase in both horizontal & vertical dimensions of the ramus & body. Uniplanar devices have a straight screw that elongates in a linear fashion when activated. Multiplanar devices have either a curvilinear track or combination of screws that expand in linear, angular & transverse direction.
INTRA-ORAL Mandibular Distraction Osteogenesis:
Distraction Osteogenesis has been shown to be an effective technique for mandibular widening & lengthening where traditional orthognathic surgery has important limitations. The Intra Oral approach of Distraction Osteogenesis prevents damage to inferior alveolar nerve & the developing dental follicles, avoids donor site morbidity, eliminates hypertrophic scars,& minimizes the need for blood transfusions. The Intra Oral device is placed either on the mandibular first molar teeth & first bicuspids or on the second molars & premolars. The device is placed anteriorly to prevent interference with the tongue. The distractor is cemented 1-2 days before surgical intervention. The device is activated 2mm seven days after surgery. Rate of distraction is 1 mm/day, activated once a day. Orthodontic tooth movement should not begin until removal of the distraction appliance, 8-12 weeks after surgery 5, 6 & 7. After the stabilization period of 8-12 weeks progressive forces is carried out. Either a tooth-borne or bone-borne appliance may be used to widen the mandible. Device fixation is achieved with three arms anchored to the bone & one arm secured to the dental arch. The appliance is activated 2mm immediately after placement.
The distractor screw must be parallel to the occlusal plane to prevent an anterior open bite from forming. To prevent any TMJ problems 6oz class II elastics are used bilaterally for 2 months after the initiation of distraction. The device is removed after completion of the stabilization period & osseous bone regeneration.
A combined maxillary & mandibular Distraction Osteogenesis is performed in patients with hemifacial microsomia. Mandibular distraction in adults leaves the patient with a severe alteration in the occlusion requiring complex orthodontic treatment. To avoid this problem, an incomplete Lefort I osteotomy is perform simultaneously with the mandibular corticotomy.
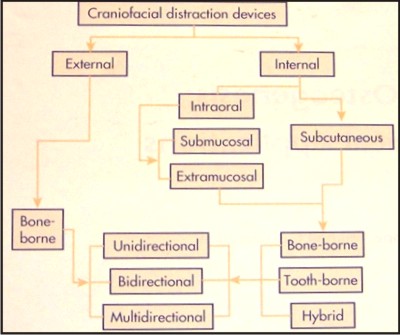 | Fig-1 Classification Of Distraction Appliances
 |
Bone borne distractor (FIG-1):
1. External Unidirectional distraction16,17 & 18: (McCarthy-1992)
The distractor consists of single calibrated rod with two clamps which holds two 2mm half pins that are placed on either side of the osteotomy. Approx. 20-24mm of bone stock is necessary to place this device (FIG-3).
Disadvantages of this type of distractor includes
Scarring due to pins.
Difficulty predicting the direction in which the distraction would proceed.
Inability to change the direction of distraction once the process has started.
2. External Bi-directional distraction:
Provides an additional degree of freedom over unidirectional device. Bi-directional distraction is necessary for correction of the two steps occlusal plane and ramus deficiency.
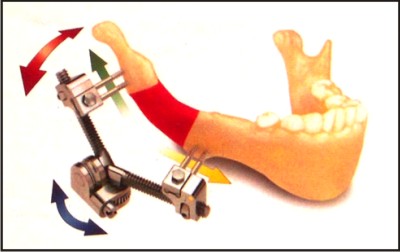
3. Multiplanar Distraction19 (FIG-4):
Two arms extend from the housing with pin clamps at either ends. Each quarter turn results in an expansion of 0.25mm. Each arm is 20mm in length for a total linear expansion of 40mm. Two activation screws enable changes in transverse & vertical angulations.
4. Internal Distraction:
Due to the criticism of the external distractors, internal distractors were developed to eliminate the problems of facial scarring, pin tract infections & high visibility. McCarthy in 1995 introduced an intraoral distraction appliance tested on the canine model. Vasquez & Diner developed two internal distractors for lengthening of mandibular body & other for ramus.
TOOTH - BORNE APPLIANCES20:
Razdolsky-1997- Introduced a completely tooth borne Intraoral distractor capable of linear changes (ROD device). Current technique starts by fitting preformed SS crowns to one tooth on either side of the anticipated osteotomy site. A rubber base impression is then taken & an intraoral distractor is fabricated in laboratory.
a. Mandibular widening8,9 & 10:
Described by Guerrero & Constasti. Indications include transverse deficiency as in Brodies syndrome & certain congenital problems. First devices used were same as those used for maxillary expansion. Harper et al & Bell et al performed mandibular midline | osteotomies in adult monkeys by employing cemented Hyrax type expansion appliance.
b. Maxillary Distraction Osteogenesis:
Maxillary hypoplasia is a common finding in patients with repaired orofacial clefts. Rigid External Distraction (RED) device enables to manage patients with severe maxillary hypoplasia.
The RED system consists of: - Cranial halo that provides skeletal anchorage & is attached using scalp screws.
Vertical bar - Extends from cranial halo & is used to attach the horizontal bar.
Horizontal bar - Carries the distraction screws which are attached to the eyelet of the splint with a surgical wire so as to enable forces to be applied to the maxilla.
The horizontal bar can move up & down the vertical bar. Vector of distraction can| be controlled by adjusting the position of the horizontal bar & the eyelets. Latency period is 3-4 days. Rate distraction is 1mm/day & consolidation period is 2-3weeks. After consolidation period the device is removed, the external traction hooks & the eyelets cut & night time use of facemask is initiated.
Maxillary advancement by Distraction osteogenesis has many advantages over conventional orthognathic procedures:
Can be done at young age
Direction of distraction can easily be controlled by the RED device
Minimal morbidity & blood loss
No need for bone grafts
Minimal relapse
Can be easily removed without anaesthesia after distraction
The only limitation of this technique is in patients who lack teeth or adequate bone in the cranial vault. Complication includes velopharyngeal incompetency.
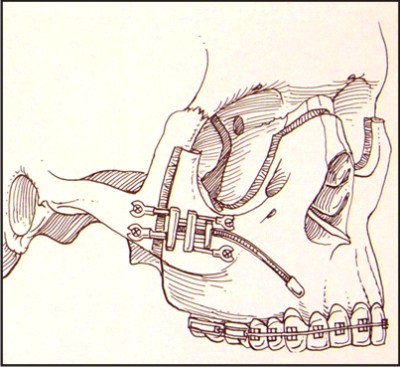
MIDFACE DISTRACTION OSTEOGENESIS (FIG-6):
Midface distraction can be carried out by intra-oral as well as extra-oral devices. Development of Modular Internal Distracrion (MID) system permits wide spread use of buried distraction devices throughout the craniofacial region. Clinical indications include
Cleft lip & palate
Hemifacial microsomia
Mid face hypoplasia
Syndromic craniosynostosis
Treacher collins syndrome
 | Fig-3 Unidirectional Distractor For Mandibular Advancement
 |
The MID device allows the surgeon to fabricate custom internal distraction devices for virtually any region of the craniofacial skeleton. In children's with Syndromic craniosynostosis & severe midface retrusion, monobloc osteotomies can be performed at younger than lyr of age. In children aged 4-7yrs, monobloc or lefort III subcranial osteotomy can be done with less operative morbidity. In children with cleft lip & palate distraction should be performed at 6yrs of age to correct midface deficiency. In children undergoing midface distraction, an acrylic bite block is attached to the mandible to simulate the increase in the vertical dimension of the maxilla after distraction. Surgical hooks are placed on the anterior dentition as well on the molar bands for application of reverse headgear. The main advantage of midface distraction is reduction of infectious complications like epidural abscess.
Dental distraction15:
Liou & Huang (1998) stated that the process of osteogenesis in the periodontal ligament during orthodontic tooth movement is similar to the osteogenesis in the mid-palatal suture during Rapid Palatal Expansion (FIG-5). They proposed a new concept of distracting the periodontal ligament to elicit rapid canine retraction in three weeks. At the time of first premolar extraction, the interseptal bone distal to the canine is undermined with a bone bur, grooving vertically inside the extraction socket along the buccal & lingual sides & extending obliquely towards the socket base. A tooth borne appliance (custom made) is then placed to retract the canines into the extraction space.
Haluk Iseria et al developed a new technique of rapid canine retraction through distraction osteogenesis. Full retraction of the canines was achieved in mean time of 10.05 (±2.01) days. The anchorage teeth were able to withstand the retraction forces with minimal anchorage loss, distraction technique is an innovative method that reduces overall orthodontic treatment time by nearly 50%, with no unfavorable effects on surrounding structures.
 | Fig-6 Maxillary Protraction Distractor
 |
 | Fig-4 Multidirectional Distractor
 |
ALVEOLAR DISTRACTION (FIG-7):
It involves mobilization, transport & fixation of a healthy segment adjacent to the deficient site. Alveolar distraction to increase the vertical height of an edentulous ridge by approximately 9mm was successfully performed in dogs.
Indications:
Primary indications are combined deficiency of the bone & the soft tissue and compromised wound healing environment.
Secondary indication is for expansion of alveolar housing for creating site for implant placement, to improve ridge esthetics for pontic, to improve periodontal environment of adjacent teeth, to expand alveolus for orthodontic tooth movement.
Limitations:
Minimum quantity of bone is present.
Transport & anchorage segment should have adequate strength.
Expansion occurs only in the direction of the transport.
Complications:
Complications are fracture of the transport, anchorage segment and premature consolidation. The atrophied superior aspects of the ridge are resected & a segmental osteotomy of the healthy bone is performed. The ridge is placed & after latency period of 5 days distraction is proceeded at a rate of lmm/day for 9 days. The device is retained for 10days. After 6 weeks, osseointegrated implants is placed in the greatly increased mass of bone. At the original location of the segment, is left a regeneration chamber which has the natural capacity to heal by filling the bone.
Future directions:
The future development of Distraction Osteogenesis in craniofacial applications will probably establish a more complete understanding of the biology of new bone formation under the influence of gradual traction.
Major trends may include: refinement of distraction protocols, modification of osteotomy techniques, further improvement of distraction devices and enhancement of regenerate maturation with pharmacologic agents. With technologic advancements, distra¬ction devices have become smaller and more sophisticated than early versions.
Development of new techniques to monitor distraction regenerate formation & remodeling. Distraction osteogenesis may even be teamed with endoscopic techniques to allow the placement of these devices with minimal surgery. Preliminary studies of rabbits have shown that distraction performed in the presence of recombinant human bone morpho-genetic protein placed into the distraction site accelerates bone formation. Several new developments are on the horizon in the field of craniofacial Distraction Osteogenesis. A successful combination of endoscopic techniques to create osteotomies and insert distraction devices will move distraction into the field of minimally invasive surgery. New work using bioresorbable materials may lead to the implementation of devices that do not require a second surgical procedure to remove them and following resorption leave no trace that they had ever been inserted In addition, use of microproce¬ssors and miniature motorized distraction devices may provide the ability to insert submerged appliances capable of auto-distraction according to pre-programmed data.
Conclusion:
Osteodistraction provides a means whereby bone can be remodeled into different shapes to more adequately address the nature of skeletal deformities: & asymmetries. Many of the congenital deformities that require extensive muscu¬loskeletal movements may be addressed with fewer procedures eventually achieving the same structural, functional; & esthetic results commonly seen with.' modern orthognathic procedures.
Future may witness the use of the concepts of distraction osteogenesis to achieve better, faster & more efficient tooth movement The applications of distraction osteogenesis in treating both simple and complex deformities of the craniofacial skeleton are restricted neither by the mechanical configuration of the distraction device nor by the biological capacity of the human body but are actually only limited by the boundaries of our imagination.
References:
1. Figueroa AA, Polley JW, Ko WC: Maxillary distraction for the management of deft maxillary hypoplasia with a rigid external distraction system, Semin Orthod 5:46, 1999.
2. Fisher E, Staffenberg DA, McCarthy JG, et al: Histopathologic and biochemical changes in the muscles affected by distraction osteogenesis of the mandible, Plast Reconstr Surg 99:366, 1997.
3. Cope IB, Samchukov ML, Cherkashin AM: Mandibular distrac¬tion osteogenesis: a historical perspective and future directions, Am Jr Orihod Dentofacial Orthop 115:448, 1999.
4. Chin M, Toth BA: Distraction osteogenesis in maxillofacial surgery using internal devices: review of five cases, Oral Maxillofac Surg 54:45, 1996.
5. Gil-AJbarova J, Melgosa M. Gil-AJbarova O, et al: Soft tissue behavior during limb lengthening: an experimental study in lambs, Pediatr Orthop 6:266. 1997.
6. Gonzalez M: Lengthening and widening the mandible by intraoral distraction osteogenesis, Master of Science dissertation, Dallas, Texas, 1998, TAMUHS-Baylor College of Dentistry.
7. Gropp H, Wangerin K: Intraoral distraction osteogenesis for lengthening of the mandibular ascending ramus. In Diner PA, Vasquez ZT, editors: International Congress on Cranial and Facial Bone Distraction Processes, Paris, France, Bologna, Italy, 1997, Monduzzi Editore.
8. Guerrero CA: Expansion mandibular quirurgica, Rev Venez Ortod 48:1, 1990.
9. Guerrero CA: Expansion rapida mandibular. Rev Venez Ortod 1-2:48, 1990.
10. Guerrero CA, Bell WH: Intraoral distraction osteogenesis: maxillary and mandiublar lengthening, Adas Oral Maxillofac Surg Clin North Am 7(11:111-151, 1999.
11. Ilizarov GA: Basic principles of transosseous compression and distraction osteosynthesis, Ortop Travmatol Protez 10:7, 1975.
12. Ilizarov GA: The tension-stress effect on the genesis and growth of tissues. I. The influence of stability of fixation and soft-tissue preservation, Clin Orthop 238:249, 1989.
13. Ilizarov GA: The tension-stress effect on the genesis and growth of tissues. II. The influence of the rate and frequency of distraction, Clin Orthop 239:263, 1989.
14. Bell WH, Gonzalez M, Guerrero CA, et al: Intraoral widening of the mandible by distraction osteogenesis: histologic and radiographic assessment, Oral Maxillofac Surg 55:97, 1997.
15. Liou EJ, Huang CS: Rapid canine retraction through distraction of the periodontal ligament Am Jr Orthod Dentofacial Orthop 114:372, 1998.
16. McCarthy JG: The role of distraction osteogenesis in the recon struction of the mandible in unilateral craniofacial microsomia, Clin Plast Surg 21:625, 1994.
17. McCarthy JG. Schreiber JS, Karp NS, et al: Lengthening the human mandible by gradual distraction, Plast Reconstr Surg 89:1.1992.
18. McCarthy JG, Staffenberg DA, Wood RJ, et al: Introduction of an intraoral bone-lengthening device* Plast Reconstr Surg 96:978, 1995.
19. McCarthy JG, Williams JK, Grayson BH, et al: Controlled multiplanar distraction of the mandible: device development and clinical application, Craniofac Surg 9:322, 1998.
20. Razdolsky Y, Pensler JM: Skeletal distraction for mandibular lengthening with a completely intraoral tooth-borne distractor. In Diner PA, Vasquez ZT, editors; International Congress on Cranial and facial Bone Distraction Processes, Paris, Prance, Bologna, Italy, 1997, Monduzzi Editore. |