Introduction
Smile is the most recognized expression in the world and is the cornerstone of social interaction. Smile is considered as the universal friendly greeting in all cultures. The value of attractive smile is undeniable. An attractive smile in modern society is often considered an asset in interviews, work setting, social interactions and even the quest to attract a mate. The essential goal of dentist’s world wide has been to achieve esthetically pleasing smile irrespective of their specialty. Just as a nice smile can act as a powerful communication tool, an unpleasing smile can have the equally powerful negative impact. One of the most common reasons for seeking orthodontic treatment is excessive display of gingival tissue on smiling, usually referred to as a gummy smile, which is often esthetically displeasing. Some people with excessive gingival display are self conscious or embarrassed about it, and some are psychologically affected. Etiological factors involved in the formation of gummy smile can be, Skeletal (vertical maxillary excess), Gingival (passive eruption) or Muscular (hyper functional upper lip) and treatment options range from Le fort I osteotomy, crown lengthening, intrusion, myectomy to muscle resection etc.
A non surgical treatment would be advantageous. Recently a non surgical and minimally invasive treatment option for correction of gingival smile has been suggested, which is use of BOTOX.
Botox is indicated when the gummy smile is due to hyper functional upper lip elevator muscles (muscular capacity to raise the upper lip is higher than average).
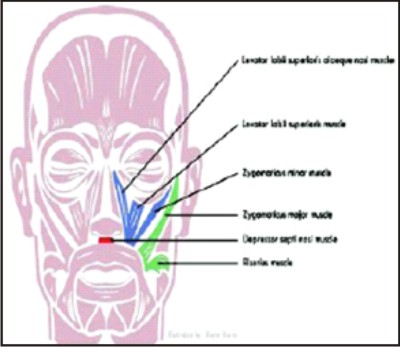
Muscles responsible for upper lip movement during smile are:
1. Levator labii superioris(LLS)
2. Levator labii superioris alaeque nasii(LLSAN)
3. Zygomaticus major
4. Zygomaticus minor
5. Depressor septii
What is Botox?
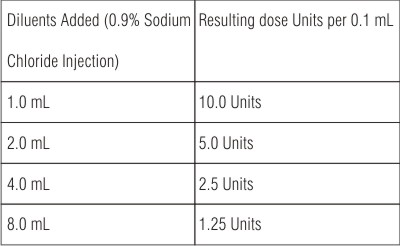
Botox is the trade name for the neurotoxin protein botulinum toxin type A produced by fermentation of anaerobic bacterium clostridium botulinum. Type A is one of the seven distinct botulinum toxins produced by different strains of the bacterium. It is a stable, sterile, vacuum-dried powder that is diluted with saline solution without preservatives for it to be injected.
The total "dose" of Botox in each vial is always 100 units but different amounts of saline solution can be used with each vial depending on the intended use
Each vial of BOTOX contains
1. 100 Units (U) of Clostridium botulinum type A neurotoxin complex,
2. 0.5 milligrams of Albumin Human,
3. And 0.9 milligrams of sodium chloride in a sterile, vacuum-dried form without a preservative.
A brief history of botox
Over the last two decades, BOTOX has been approved by the Food and Drug Administration (FDA) for therapeutic treatments of eye muscle problems (in 1989), neck problems (in 2000), and excessive sweating (in 2004). At present, it is being investigated for treating other medical conditions. In 2002, the FDA approved Allergen’s BOTOX Cosmetic for the purpose of temporarily erasing facial lines1, 2 & 3.
Mechanism of Action
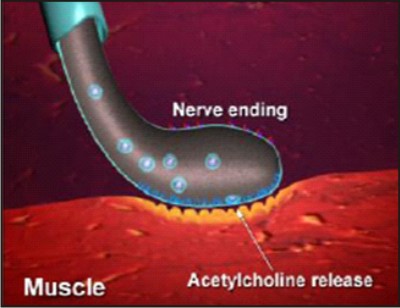
BOTOX decreases muscle activity by blocking overactive nerve impulses that trigger excessive muscle contractions or glandular activity
Phase I. Nerve-Muscle Communication is blocked
BOTOX blocks the transmission of overactive nerve impulses to the targeted muscle by selectively preventing the release of the neurotransmitter acetylcholine (ACh) at the neuromuscular junction, temporarily preventing muscle contraction. This is primarily a local effect. BOTOX may also prevent the release of pain-stimulating neuropeptides in peripheral nerves.
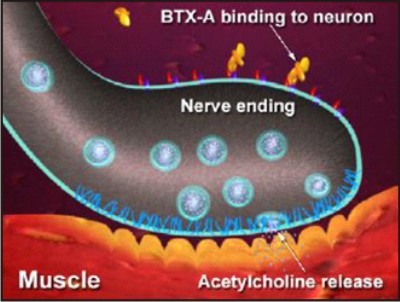 | Fig 1
 |
A) Binding (Fig-1):
The heavy chain portion of the active ingredient in BOTOX binds to the cell membrane of the motor nerve via an unidentified high-affinity “acceptor” molecule. This high-affinity binding action allows for efficient uptake of BOTOX® by the motor nerve and facilitates selective, targeted treatment at the injection site.
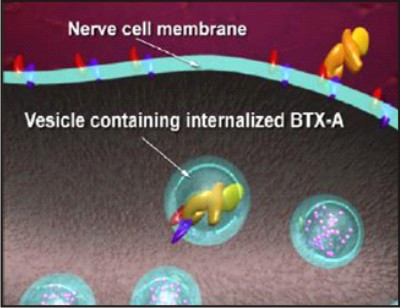 | Fig 2
 |
B) Internalizing (Fig-2):
After binding, the BOTOX protein molecule passes through the cell membrane of the motor nerve and into its cytoplasm via a process called endocytosis. It is here that the enzymatic component (light chain) of the BOTOX protein molecule is activated.
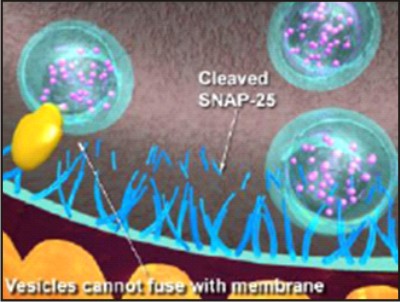 | Fig 3
 |
C) Blocking (Fig-3):
Inside the motor nerve, the light chain of the BOTOX® protein molecule cleaves apart a protein (called SNAP25) that enables vesicles which store the neurotransmitter acetylcholine to attach to the cell membrane. Cleaving SNAP25 prevents these vesicles from fusing with the membrane and prevents the release of acetylcholine into the neuromuscular junction (the space between the motor nerve and the muscle). Thus, nerve impulses that control muscle contractions are blocked decreasing muscle activity. Cleaving SNAP25 also blocks release of neuropeptides involved in the transmission of painful sensations (including substance P, glutamate and calcitonin gene-related peptide, or CGRP), theoretically reducing pain sensitization of peripheral nerves. This may be how BOTOX reduces the neck pain associated with cervical dystonia, although the exact mechanism of action is unknown.
Phase II. Nerve-Muscle Communication is restored
The effect of BOTOX is generally temporary. Previous nerve impulse activity and associated muscle contractions resume over the course of a few to several months, depending on the individual patient and the indication for which they are being treated.
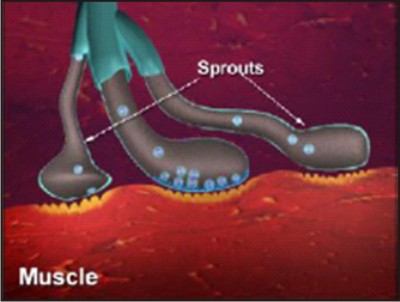 | Fig 4
 |
A) Nerve Sprouting (Fig-4):
New nerve endings sprout and connect to the muscle after the original nerve ending is blocked, renewing the ability of the nerve to cause muscle contractions.
 | Fig 5
 |
B) Original Nerve Connection Re-established (fig 5):
Eventually, the new nerve sprouts retract and the original nerve ending regains its function, suggesting that treatment with BOTOX does not permanently alter the neuromuscular junction.
Indications:
1. Strabismus
2. Cervical dystonia,
3. Blepharospasm and
4. Hemifacial spasm,
5. Hyperfunctional larynx,
6. Juvenile cerebral palsy
7. Spasticity
8. Pain and headache
9. Occupational dystonia and writer.s cramp,
Uses in dentistry:
1. Tempromandibular disorders
2. Massetric hypertrophy
3. Hemifacial spasm
4. Myofacial pain
5. Bruxism
6. Trismus, sialorrhea
7. Retraining muscles during orthodontic therapy, in patients with a very strong musculature.
8. Training the patient to get used to new dentures, especially in patients with strong irregular muscle contractions, who have been edentulous for a long time and have old dentures and they are significantly over closed.
9. Jaw line contouring by injecting into masseter muscle thus weakening it and some bulk of this muscle is reduced, resulting in a more tapered jaw line.
Procedure for injection:
For correction of gummy smile, Botox is injected into the hyperactive elevator muscles of lip blocking excessive contractions and thus prevent the lip from being pulled too far up while smiling. It will be important for the patient to avoid taking aspirin or related products, such as ibuprofen (e.g., Advil) or naproxen if possible after the procedure to keep bruising to a minimum. Prior to injection, reconstitute vacuum-dried BOTOX, with sterile normal saline without a preservative; 0.9% Sodium Chloride Injection is the only recommended diluents. Draw up the proper amount of diluents in the appropriate size syringe, and slowly inject the diluents into the vial. BOTOX should be administered within four hours after reconstitution. During this time period, reconstituted BOTOX should be stored in a refrigerator (2° to 8°C). Reconstituted BOTOX should be clear, colorless and free of particulate matter.
 |
 |
Mario Polo4, 6 has advocated injection of botox at LLS, LLSAN, LLS /ZM overlap and in severe cases at depressor nasii & OO also. The ideal dosage might be 2.5 U per side at the LLS & LLSAN, 2.5 U per side at the LLS/ZM sites, and 1.25 U per side at the OO sites.
Very recently Hwang et al5; Yonsei University College of Dentistry, Seoul, Korea have proposed a injection point for botulinum toxin-A, and named it as YONSEI POINT and they recommend a dose of 3U at each Yonsei point
 | Fig 6
 |
Yonsei point is located at the centre of the triangle formed by (Fig-6):
1. levator labii superioris [LLS],
2. levator labii superioris alaeque nasi [LLSAN],
3. and zygomaticus minor [Zmi].
How often do patients need to return for additional injections?
Effect of Botox is seen within 5-10 days and lasts about 6 months, with a range of 4 to 8 months, at which time the patient can return to repeat the process. It is important not to give injections prematurely (before the effects of the treatment have worn off), as this can result in a buildup of antibodies to Botox that would dilute the effect of further treatments.
Contraindications
1. During pregnancy or while breast feeding
2. Presence of inflammation or infection at the site of proposed injection
3. Anyone with known hypersensitivity or allergies to human albumin, Botox toxin, or saline solution.
4. Anyone with known motor neuropathy, neuromuscular disorders such as amyotrophic lateral sclerosis, myasthenia gravis, Lambert-Eaton Syndrome, muscular dystrophy, multiple sclerosis etc.
5. Anyone taking Aminoglycoside antibiotics because aminoglycosides may interfere with neuromuscular transmission and potentiate the effect of Botox therapy.
6. Anyone taking Calcium Channel Blockers.
Side effects
1. Nausea
2. Localized pain
3. Infection
4. Inflammation
5. Tenderness
6. Swelling
7. Redness, and/or
8. Bleeding/bruising
Disadvantages
1. Short term effect
2. Asymmetrical/unnatural appearance of smile sometimes due to improper injection technique
3. Cost factor
Advantages
1. Psychological benefit to the patient
2. Minimally invasive
Should dentists administer Botox therapy?
With plastic surgeons, dermatologists, internal medicine physicians, obstetricians-gynecologists,
ophthalmologists, podiatrists, nurses, physician’s assistants, and medical aestheticians (who may not even be medically trained) delivering BOTOX to patients in the oral and maxillofacial areas, it is certainly time to recognize that dentists can be just as proficient in injections than any of these healthcare providers as dentists have much expertise in the oral and maxillofacial areas and are also trained to be experts in the muscles of mastication and the muscles of facial expression which routinely receive these treatments.
Conclusion:
It is time to broaden our horizons as a profession and use all of the tools available to us. BOTOX therapy is a conservative, minimally invasive treatment that can expand our therapeutic options for the benefit of our patients and is a natural progression of where we are going in the dental industry. These procedures are easy to accomplish by general dentists with proper training.
References
1. Peck S, Peck L, Kataja M. Some vertical linear measurements of lip position. Am J Orthod Dentofac Orthop 1992; 101:519- 524.
2. Lowe N J. Botulinum toxin type A for facial rejuvenation: United States and United Kingdom perspectives. Dermatol Surg. 1998. 24: 1216.
3. Binder WJ, Blitzer A, Brin MF. Treatment of hyperfunctional lines of the face with botulinum toxin A Dermatol Surg. 1998; 24:1198-1205.
4. Mario polo. Botulinum toxin type A in the treatment of excessive gingival display; AJO DO 2005; 27(2):214-218.
5. Hwang et al. Surface anatomy of the lip elevator muscles fort he treatment of gummy smile using botulinum toxin. Angle Orthod 2009; 79(1): 70-77.
6. Mario Polo. Botulinum toxin types A (Botox) for the neuromuscular correction of excessive gingival display on smiling (gummy smile) AJO DO 2008; 133(2):195-203. |