Introduction
The conditioning of the enamel surface with phosphoric acid (Bunonocore,1955)1 and the development of composite resin cements (Bowen,1962)2 revolutionized aesthetic dentistry and practice of orthodontics. Traditional methods of bonding orthodontic brackets to teeth have relied on the use of the acid etch technique to achieve adequate retention. However, primary concern to the clinician is the maintenance of a sound enamel surface after removal of the bracket
Despite the numerous publications in the field of orthodontic bonding, the orthodontic literature lacks studies that identify the most suitable bracket base-cement combinations. Similarly, there is no information on the interaction between bracket base design and cement particle size. Furthermore, bracket base-cement bond failure still occurs and this is costly to both patients and clinicians and may prolong treatment time. Given the wide variety of orthodontic bracket base designs and the myriad of bonding cements available today, it is important to identify bracket base-cement combinations that are clinically practical, provide adequate shear bond strength, result in minimal or no damage to enamel during bonding, orthodontic treatment and debonding.
The purpose of this study was to identify the shear bond strength of a light cure Resin modified Glass ionomer cement with three different types of brackets (Titanium, Stainless Steel and Ceramic) and the enamel damage on debonding.
Aims And Objectives
The Aims and Objectives of this study were:-
1. To compare the shear bond strength of Resin Modified Glass ionomer cement with three different types of brackets: - Titanium, Stainless Steel and Ceramic.
2. Comparision of the enamel loss on debonding the bracket with the help of scanning electron microscope among the three different types of bracket materials.
3. Quantifying the adhesive remaining on the tooth surface after debonding the bracket by Adhesive Remnant Index (ARI) and Comparision of the ARI among the three different types of bracket material .
Materials And Methods
Thirty human premolars were collected and stored in 1% thymol and they were cleaned with water, pumice, and a rubber cup, and then rinsed with water. The samples were mounted in acrylic resin cylinders and were randomly divided into three groups of 10 each, to be bonded with the following premolar brackets (SEM photograph I):
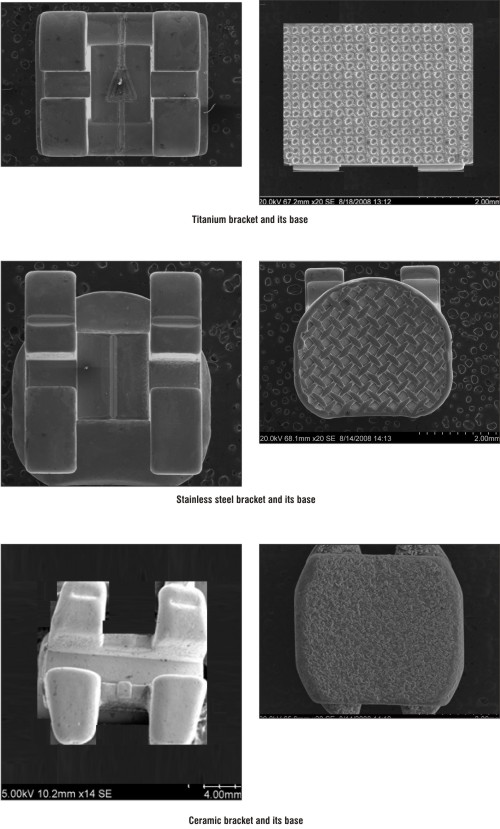 | SEM PHOTOGRAPH – I: Types of brackets and their bases
 |
Group 1 Dentaurum Discovery titanium brackets (Eqilibrium ti) with laser-etched pads.
Group II 3M Unitek Stainless Steel brackets (Gemini) with 80 gauge micro-etched woven mesh bonding pad.
Group III 3M Unitek ceramic brackets (clarity) machined, integral, microetched base with mechanical undercuts.
Conditioned (etched) bonding protocols were followed for Fuji Ortho LC cement. When the enamel surface was conditioned, it was conditioned by brushing 37% Phosphoric acid on to the labial surface. The conditioner was left undisturbed for 30 seconds and then rinsed thoroughly with distilled water for 30 seconds. The enamel surface was not dried but was moistened with distilled water just before bonding. The Fuji Ortho LC cement was mixed following manufacturers guidelines. One level spoonful of powder and two drops of liquid were dispensed on to a mixing pad. The powder was incorporated into liquid in two equal portions. The first portion was mixed into the liquid for 10 seconds. The second part was then added and mixed for another 10-15 seconds. The total mixing time did not exceed 20-25 seconds. Each bracket was bonded to the buccal surface so that slot lies parallel to the incisal edge of the premolar. Each mix was used to bond two brackets only. Then the cement was light cured, using a dentsply visible-light-curing unit for 20 seconds on the mesial and distal sides of the bracket base, for a total of 40 seconds. Upon completion of bonding and curing procedures, each specimen was stored for 24 hours in deionized distilled water at 37°C in container.
The shear bond strength of brackets were find out by using the Instron universal testing machine (3654). Each specimen was clamped in a holding ring so that the bracket base was parallel to the direction of the force. The sharpened chisel blade suspended from the upper arm of the testing machine was placed at the bracket enamel interface just short of contact in an incisogingival direction. Using a crosshead speed of 0.5mm/minute the bracket bases were shear tested to failure. The maximum force was recorded in Newtons (N) and converted to megapascals (MPa). Mean shear bond strength were calculated for each group .The values were compared by the analysis of variance (ANOVA).
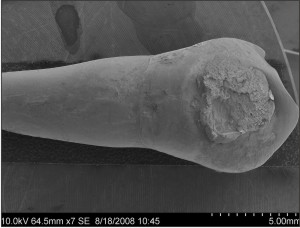
After debonding, all the specimens were carefully collected and were mounted on an aluminum Scanning electron microscope stud so that the labial surfaces were at 45 angulation. Al1 the specimens were then sputter coated with 3 nm of gold in a Polaron E5 coating unit and viewed with a Hitachi-S-3304 SEM at an operating voltage of 10 kV. Scanning electron microscopy views of each specimen were obtained at 7x, and 750x magnifications.
3 SEM photographs from the three different groups at 7x magnifications were taken to study the tooth after debonding the individual brackets, 3 SEM photographs were taken at 750x magnifications to study the enamel surface underlying the bracket base after debonding the individual brackets . Visual analysis was made to investigate compatibility of each bracket base surface characteristic with the Fuji ortho LC depending on the amount of adhesive remaining on the tooth surface. The Adhesive Remnant Index (ARI) was used to quantify and the amount of cement left on the tooth following debonding of the bracket. AR1 Scoring Index (Artun and Bergland, 1984) 3
0 No cement left on the tooth
1 Less than half of the cement left on the tooth
2 More than half of the cement left on the tooth
3 Al1 of the cement left on the tooth plus a distinct impression of the bracket base.
Results
The results were statistically analysed using the following statistical analysis. One way analysis of variance (ANOVA analysis) indicating the significant different among the bracket types (p 0.001). Titanium brackets had the highest mean shear bond strength and perform significantly differently from other two bracket materials.
Group I: Dentaurum Discovery Titanium brackets with laser etched pads (Eqilibrium ti) showed mean shear bond strength of 8.23+ 0.74 Mpa9 (Table I). The ARI scoring index shows (Table II), 10 % of the total sample size under the grade 0 which implies that there was no adhesive left on the tooth on debonding the bracket in the above mentioned 10% of the sample size,10% of the total sample size under the grade 1 which implies less than half of the adhesive left on the tooth surface after debonding,30% of the total sample size under grade2 which implies more than half of the cement left on the tooth surface after debonding and 50% of the total sample size under grade 3 which implies the whole of the adhesive left on the tooth surface along with distinct impression of the bracket base after debonding.
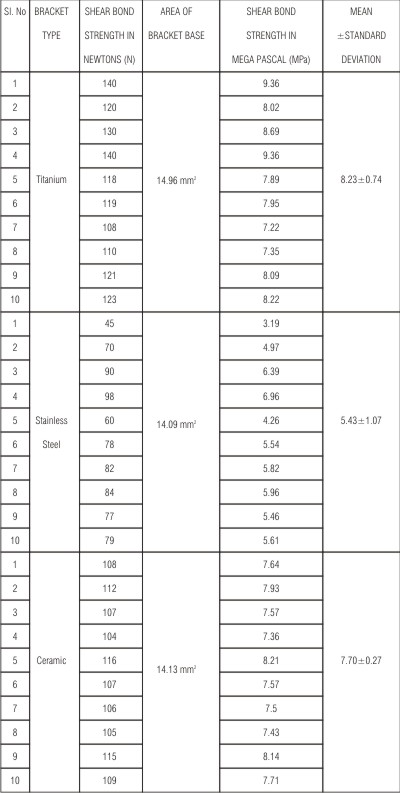 | Table I Shear Bond strength of various brackets in megapascals along with the mean and standard deviation for the individual group of brackets.
 |
 | Table II Adhesive Remnant Index (ARI Scores), sample size and Percentile Distribution
 |
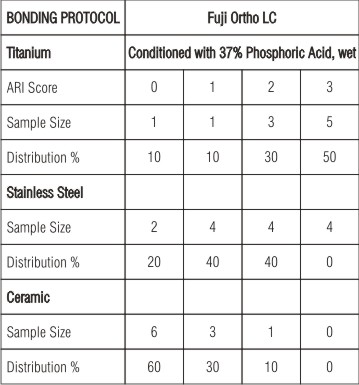
The Scanning Electron microscopic study (Photograph II, III) at 750X magnification clearly shows the adhesive left on the enamel surface without any exposure of the underlying enamel lying under the bracket base.
 | Sem Photograph - II : Showing Tooth Surface After Debonding Titanium Brackets
 |
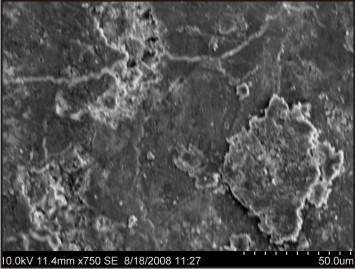 | Sem Photograph - III : Showing Enamel Surface After Debonding Titanium Brackets
 |
Group II: Stainless steel brackets with 80 gauge microetched woven mesh bonding pad (Gemini) showed mean shear bond strength of 5.43+1.07 MPa (Table I). The ARI scoring index (Table II ) shows, 20 % of the total sample size under the grade 0 which implies that there was no adhesive left on the tooth on debonding the bracket, in the above mentioned 20% of the sample size,40% of the total sample size under the grade 1 which implies less than half of the adhesive left on the tooth surface after debonding,40% of the total sample size under grade2 which implies more than half of the cement left on the tooth surface after debonding and 0% of the total sample size under grade 3 which implies that this group had no samples with the whole of the adhesive left on the tooth surface along with distinct impression of the bracket base after debonding.
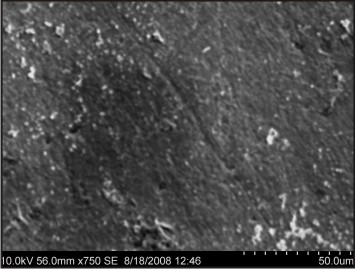
The Scanning Electron microscopic study (Photograph VI, V) at 750X magnification shows the exposure of the enamel surface lying under the bracket base with clear microporosities which have resulted due to the conditioning of the enamel surface prior to the bonding proceedure.
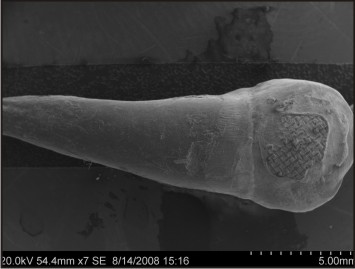 | Sem Photograph - IV : Showing Tooth Surface After Debonding Stainless Steel Bracket
 |
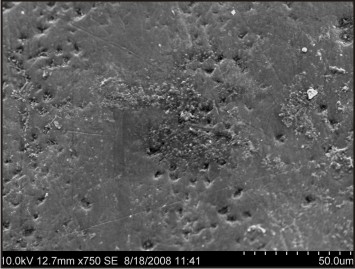 | Sem Photograph - V : Showing Enamel Surface After Debonding Stainless Steel Bracket
 |
Group III: 3M unitek ceramic brackets with machined integral micro etched base having mechanical undercuts (clarity) showed mean shear bond strength of 7.70± 0.27 Mpa (Table I) .The ARI scoring index (Table II) shows, 60 % of the total sample size under the grade 0 which implies that there was no adhesive left on the tooth on debonding the bracket, in the above mentioned 60% of the sample size,30% of the total sample size under the grade 1 which implies less than half of the adhesive left on the tooth surface after debonding,10% of the total sample size under grade2 which implies more than half of the cement left on the tooth surface after debonding and 0% of the total sample size under grade 3 which implies that this group had no samples with the whole of the adhesive left on the tooth surface along with distinct impression of the bracket base after debonding. The Scanning Electron microscopic study (Photograph VI, VII) at 750X magnification shows the exposure of the enamel surface lying under the bracket base with clear loss of the enamel in the form of gouging, scratching and gross surface irregularities of the enamel surface.
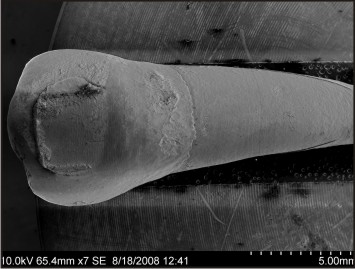 | Sem Photograph - VI : Showing Tooth Surface After Debonding Ceramic Bracket
 |
 | Sem Photograph - VII : Showing Enamel Surface After Debonding Ceramic Bracket
 |
Discussion
This study was undertaken to identify the ideal bracket materials that provide clinically practical ,adequate shear bond strengths and produce minimal or no damage to enamel during orthodontic treatment and debonding.The bond between enamel and orthodontic bracket is unique in dentistry in that it is intended to be temporary. The bond is required to remain intact for upto 2 years withstanding both orthodontic forces and the forces of occlussion, but then must be broken with minimum amount of trauma to the tooth and the patient.After debonding, the enamel underlying the bracket will be exposed to the oral environment for the remainder of the life of the tooth. It is therefore essential that the whole cycle of bond, treatment, and debonding preserves the integrity of the enamel as far as possible.
Bracket material along with the base design is an important variable which can effect the bond strength of bracket bases to enamel. There are currently three bracket materials available, and they are: metal, ceramic and titanium brackets .Each of these bracket types employs different mechanisms of retention that are incorporated into their base designs. . In metal brackets the bond strength to the bracket base and tooth surface is primarily achieved by mechanical mechanisms. Various base designs that impart mechanical retentive properties to metal bracket bases are Perforated Bases, Foil mesh bases, Integral bases, Sintered bases, Photoetched bases and sandblasting. The disadvantage of aesthetics associated with metal brackets was addressed with the introduction of ceramic brackets in1986 and they had been gaining popularity ever since. Ceramic brackets derived addition to the tooth surface through mechanical retention, chemical bonding or both.
The high tensile strength and low fracture toughness of ceramic brackets resulting in the failure of ceramic brackets during orthodontic mechanotherapy and this lack of the peel of the bracket base away from the tooth surface upon the application of the shear stress was a consistent cause of the trauma of a enamel surface during the debonding procedure.
To overcome the disadvantages of corrosion, nickel allergy, aesthetics associated with stainless steel and low fracture toughness, increased frictional resistance and a thicker bracket profile associated with ceramic brackets, Titanium alloys have been approved and encouraged as orthodontic brackets by various orthodontic manufacturer’s.
Reynolds4 suggested that minimum bond strength of 6-8 MPa was adequate for most orthodontic needs. Retief5 indicated that bond strength as high as 13.8 MPa can cause bond failures at enamel adhesive interface and detrimental loss of enamel. Ideally during debonding one would require that the entire adhesive remain on the bracket and be removed cleanly from the tooth without fracture of enamel and adhesive. This implies clinicians should avoid using bracket adhesive combinations that can result in significantly greater bond strength as high as 13.8 Mpa.
ARI was useful in determining the bond failure sites by ranking the amount of resin remaining on scanned tooth images after debonding. O ‘Brein et al6 suggested that the ARI score depended on many factors , which include the bracket base design and adhesive type , and not only the bond strengths at the interfaces.
Hence this study was undertaken to identify the ideal bracket type with its individual base design that provides clinically acceptable shear bond strength and minimal or no damage to enamel during debonding .Three different groups of bracket materials were tested (titanium, stainless steel, ceramic) for the mean shear bond strength in an universal Instron testing machine. Each group is comprised of 10 samples. The amount of adhesive remaining on the tooth surface after debonding was quantified by visual inspection and graded on ARI scoring index (Artun and Bergland)3 for each group of bracket materials. The debonded enamel surface was examined by scanning electron microscope to indentify the enamel damage upon debonding the individual group of brackets.
In the present study Titanium brackets with laser structured bases showed the highest mean shear bond strength values (8.23±0.74) (Table I). The ARI scoring index had 50% of the total sample size under Grade 3 which indicated that the Titanium brackets had a bracket failure more at the adhesive bracket interface (Table II). The results agree with the previous studies that the laser structured bracket base retention mechanism provided the strongest tensile bond strength and the use of Discovery retention mechanism with resin reinforced glass ionomer cement is sufficient to obtain clinically optimal bond strength.
The findings on the ARI score indicate a greater trend for all of the adhesive resin to remain on the tooth surface after debonding(50% of the teeth had an ARI score of 3 and 30% of the teeth had an ARI score of 2). These findings indicate that the weakest point of this system is the adhesive bracket interface which has an advantage of causing less damage to the enamel surface.
Stainless steel brackets with 80 gauge microetched woven mesh bonding pads showed the lowest mean shear bond strength values (5.43±1.07) (Table I). The ARI scoring index had 0% of the total sample size under Grade 3, 40% of the total sample size under Grade 2, 40% of the total sample size under GradeI and 20% of the sample size under Grade (Table II).The low shear bond strength with stainless steel could be due to a number of variables as explained by (Maijer and Smith1981)7:-
1. Weld spots in the integral woven foil mesh base could reduce the retentive area.
2. Corrosion of the mesh bases following leakage at the resin mesh interface.
3. Lack of resin penetration into the woven foil mesh bonding pad.
4. Stress concentration at the resin mesh interface.
The findings on the ARI score indicate a greater trend for less than half the adhesive resin to remain on the tooth surface after debonding (40% of the teeth had an ARI score of 2 and 40% of the teeth had an ARI score of 1). These findings conclude that the bond failure with stainless steel brackets occurred at the mesh base resin interface. An advantage of this location of the bond failure in the present system is the minimal enamel damage underlying the debonded bracket base as illustrated by SEM photograph V. Hence this study goes in accordance with the previous literature (Bishara and Soliman 2004) 8 which states machined integral bases were more retentive than foil mesh bases.
In the present study ceramic brackets with machined integral mico etched base showed the mean shear bond strength values (7.70±0.27) (Table I). The ARI scoring index had 60% of the total sample size under Grade 0 which indicated that the ceramic brackets had a bracket failure more at the enamel adhesive interface (Table II). There was no statistically significant difference in the mean shear bond strength of ceramic and stainless steel brackets. (p value 0.05). The clarity bracket used in this study offers a mechanical bond with the adhesive .The retentive grooves in the base of brackets have sharp edge angles and there are crosscuts to prevent the bracket from sliding along the undercut grooves. This can lead to high localized stress concentrations and result in the brittle failure of adhesive. The ARI scoring index indicates a great trend for the adhesive to remain on the base of the bracket with 60% of the sample size being scored under the Grade 0. 40% of the sample size was scored under grade 1 and 2 which implies part of adhesive left on the bracket base and part of the adhesive on the tooth surface. This finding can be explained by the brittle failure of the adhesive under the mechanically retained base of the ceramic brackets (Bishara, and Timothy1990)9. The enamel damage in the form of scrathes, gouging and surface irregularities (SEM photograph VI, VII) was more with the clarity brackets when compared to the stainless steel (SEM photograph IV, V) and titanium bracket materials (SEMphotograph II, III). This study supports the previous publication by (Odegaard and Segner1998)10 that the bond strength between the ceramic bracket and adhesive in the shear mode is stronger than that between the adhesive and enamel.
Metal lined clarity ceramic brackets is collapsible under the application of shear stress when compared to the traditional ceramic bracket which are highly brittle and lack the peel effect upon debonding. Mean shear bond strength of ceramic bracket in this study did not significantly deviate from the values obtained with the traditional ceramic brackets depending upon mechanical retention from the previous literature (Samir E.Bishara1997)11 However the sample size experiences the enamel damage has drastically decreased from the traditional ceramic group due to collapsible nature of clarity brackets.
Hence it can be inferred from the result of present study that Discovery titanium bracket with laser structured bases offer higher mean bond strength values and a bracket failure more at the bracket base adhesive interface. Hence Titanium base cement combinations are ideal in the invivo environments because this combination produces clinically acceptable mean shear bond strength with minimum or no enamel damage on debonding.
Although the mean shear bond strength was not significantly difference between ceramic and stainless steel brackets, the mode of bond failure in the adhesive seen with the stainless steel brackets is an advantage since there is no detrimental loss of enamel.
Since greater shear bond strength are associated with chemical retained ceramic brackets when compared to mechanically retained ceramic brackets. Although the shear bond strength values had been drastically reduced with mechanically retained clarity brackets as compared to the chemically retained ceramic bracket bases, certain amount of enamel damage during debonding with the bracket failure more at enamel-adhesive interface is still an issue. Hence the need for an alternate mode of debonding like laser, electrothermal and ultrasonic debonding than mechanical means is necessary for ceramic brackets to maintain the integrity of the enamel .Thus, when aesthetic is a prime concern , mechanically retained ceramic brackets and alternate modes of debonding are best advised to patient. This study can be persued with different adhesives ranging from epoxy resins to modified Glass ionomer cement as the shear bond strength can be influenced by variety of factors other than bracket base design like cement particle size of the adhesive , chemical composition of the adhesive, type of cement, enamel treatment and long storage time.
Conclusion
The following conclusion can be started from this invitro investigation:-
1. The Dentaurum discovery titanium brackets with laser structured bases had the higest mean shear bond strength values with modified glass ionomer cement, stainless steel brackets with foil mesh bases had lowest bond strength values, and clarity ceramic brackets with integral machine undercuts had bond strength values which ranged between titanium and stainless steel.
2. The ARI Scoring index indicated bond failure more at the adhesive bracket base interface with Titanium brackets, within the adhesive with stainless steel brackets and at enamel –adhesive interface at clarity ceramic brackets.
3. Scanning Electron Microscopic observation of debonded enamel surface shows no enamel damage with Dentaurum Discovery Titanium brackets, minimal enamel exposure in form of porosities with stainless steel brackets and detrimental enamel loss with clarity ceramic brackets.
Hence it can be concluded that Dentaurum Discovery Titanium brackets –Resin modified glass ionomer cement combination would be an ideal option when compared to stainless steel and ceramic bracket- Resin modified glass ionomer cement.
When aesthetic is a primary concern , mechanically retained clarity ceramic brackets can be used in combination with Resin modified glass ionomer cement with alternate mode of debonding rather than mechanical , to prevent damage to enamel upon debonding the brackets.
Bibliography
1. Buonocore A simple method of increasing the adhesion of acrylic filling materials to enamel surface J Dent Res. 1955; 34: 849–853.
2. Bowen Compatibility of various materials with oral tissues the components in composite Restorations. J Dent Res. 1979 (1493–1503).
3. Jon Artun Sven Begland clinical trials with crystal growth conditioning as an alternative to acid etch enamel treatment Am J Othodontics & Dentofacial orthopedics Volume 1984 May (333- 340)
4. Reynolds I A review of direct orthodontic bonding British journal of orthodontics vol 1979(171-178)
5. Retief Failure at the dental adhesive-etched enamel interface Journal of oral rehabilitation 1974(265-271)
6. Brien, Read, Sandison, and Roberts Visible light-activated direct-bonding material Am J Othodontics & Dentofacial orthopedics Volume 1989 Apr (348 - 351).
7. Maijer and D. C. Smith Variables influencing bond strength of metal orthodontic bracket bases. Am J Othodontics & Dentofacial orthopedics Volume 1981 april (145 – 197).
8. Bishara Soliman, and john F. Laffon The effect of variation in the mesh – base design on the shear bond strength of orthodontic brackets Angle Othodontics Volume74, 2004 (400-404)
9. Bishara, Timothy, and Trulove Different debonding techniques for ceramic brackets Am J Othodontics & Dentofacial orthopaedic Volume 1990 Aug (145 - 153).
10. Odegaard and Segner. Shear bond strength of metal brackets compared with new ceramic bracket Am J Othodontics & Dentofacial orthopaedic Volume1988 Sep (201 - 206).
11. Samir Bishara Evaluation of debonding characteristics of a new collapsible ceramic bracket Am J Othodontics & Dentofacial orthopaedic Volume1997 Nov (552 - 559).
12. Jost-Brinkmann, Stein, Miethke, and Nakata Thermodebonding of metal and ceramic brackets Am J Othodontics & Dentofacial orthopedics Volume 1992 Nov(421-426).
13. Corey . Conral , Robert N. Staley, Jane Jakobsen Bond strength of resin modified glass ionomer with five orthodontic brackets Journal of clinical orthodontics Volume 2000May(286- 289).
14. David . Hamula and Waren Hamula pure titanium orthodontic brackets Journal of clinical orthodontics Volume 1996 March(140-144).
15. Pulido and Powers .Bond strength of orthodontic direct-bonding cement plastic bracket systems in vitro Am J Othodontics & Dentofacial orthopedics Volume1982 Feb (87 - 92). |