Introduction
The successful bonding of composite resins to acid-etched enamel has become a routine part of current orthodontic practice; therefore, the ability to obtain stronger bond strengths must remain a focus for research.
Wetness was considered having an effect on the shear bond strength of composites to enamel and dentin surfaces for many years.1 However, recent developments of primers and composites have succeeded to enforce the bond strength in a humid environment.2, 3 Yet, most orthodontists believe in a dry field as the keynote factor for success in the bonding process. Various methods have been used in the past to dry the tooth surface after etching viz dabbing with a blotting paper, using compressed air, using warm air from a hair dryer or using a warm air tooth dryer4.
Batchelder et al5, in a study designed to evaluate the effects of varying the source and purity of drying air, found higher shear bond strengths for specimens dried with warm air than those dried with room-temperature compressed air. The source of warm air was a 1,750-W commercial heatgun, and the temperature of the air, as measured near the enamel site, was 50°C. Galan et al6 also found significantly increased shear bond strengths with the use of warm air, but did not report the source or temperature of the air or the time elapsed between placement of the composite resin and testing.
Many orthodontists have used warm air to dry etched enamel in their studies.7-12 However, no study has been done to assess the effectiveness of warm air to dry the etched enamel surface, while bonding orthodontic brackets. The purpose of this study was to test, in vivo, the effect of using warm air for drying the tooth surface after etching, on the shear bond strength of orthodontic brackets. This shear bond strength was also compared to the shear bond strength of brackets bonded after using compressed air from the dental 3-way syringe for drying the etched enamel.
Materials And Methods
A group of 15 patients with 30 pairs of premolars to be removed for orthodontic purposes agreed to participate in this investigation. The patients' ages ranged from 13 to 17 years. Only teeth without caries, demineralization, or restorations were used. The selected premolars were cleaned with a non-fluoride pumice to remove plaque and pellicle. All these premolars which were to be extracted were etched with 37% phosphoric acid for 40 seconds and rinsed.
Control Group
After etching and rinsing, the premolars in the left side of the mouth (30 in number) were dried with moisture free compressed air using the dental 3-way syringe. (Figure 1).
 | Figure 1 : Dental 3-way Syringe
 |
Experimental Group
After etching and rinsing, the premolars in the right side of the mouth (30 in number) were dried with warm air using a commonly used hair dryer (Crown pvt ltd, 750 W, 110 V and 50 hertz) for 10 seconds/tooth. (Figure 2).
 | Figure 2 : Warm Air Dryer Used In The Study
 |
After drying, a thin layer of Transbond XT primer (3M Unitek) was applied to the enamel surface and light cured for 10 seconds. Brackets were bonded onto the center of the buccal surface of teeth with Transbond XT (3M Unitek), a light cured composite adhesive. Before curing, the excess resin material was removed with a sharp scaler without disturbing bracket position; the adhesive was light cured for a total of 40 seconds, following manufacturer’s instructions. One hour after bonding, the experimental teeth were removed and stored at 100% relative humidity until analysis. All extractions were done without putting pressure on the bonded brackets. (Figure 3).
 | Figure 3 : Teeth Immediately After Extraction
 |
Metallic first premolar brackets (Dentaurum equilibrium 2) were used in the study. The same light-cured composite adhesive resin, Transbond XT paste (3M Unitek),and the same light source, Monitex Bluelex LD-105 LED light curing unit, were used to bond brackets in both the groups.
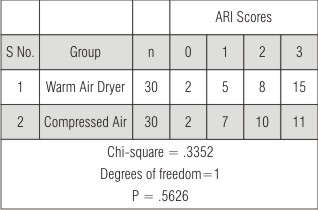
The teeth were embedded in acrylic resin placed in cuboidal aluminum blocks. (Figure 4).
 | Figure 4 : Ready Samples With Color Coding Done: Yellow – Control Group, Blue – Experimental Group
 |
A mounting jig was used to align the facial surfaces of the teeth perpendicular with the bottom of the mold. This kept the buccal surface of the tooth parallel to the applied force during the shear test.
Bond Strength Testing
Shear bond strength was tested immediately after the teeth were extracted and mounted. Shear bond strength test was done with a JJ Lloyd Universal testing machine (Figure 5) having a capacity of 20000 N (2040 kg).
 | Figure 5 : Universal Testing Machine
 |
The aluminium block with mounted premolar and its bonded bracket were positioned in the jig, so that the labial surface is parallel to the force during the shear strength test. A steel rod with a flattened end was used to apply load at the bracket. The brackets were shear tested to failure using a load cell of 12N (1.22 Kg) and a crosshead speed of 1.0 mm / min. The force producing failure was recorded in Newton by a computer attached to the machine and converted into force per unit area (MPa) by dividing the measured force values by the surface area of the bracket. The surface area of the mesh was approximately 9.608 mm2 as measured with digital vernier calipers.
Adhesive Remnant Index:
The percentage of the surface of the bracket base covered by adhesive was determined using Stereomicroscope with an eye piece magnification of 16x. The percentage of the area still occupied by adhesive remaining on the tooth after debonding was obtained by subtracting the area of adhesive covering the bracket base from 100%. Later each tooth was assigned an adhesive remnant index (ARI) value according to Artun and Bergland. (Figure 6).13
Score 0: No adhesive left on the tooth
Score 1: Less than ½ of adhesive left on the tooth
Score 2: More than ½ of adhesive left on the tooth
Score 3: All adhesive left on the tooth
Statistical Analysis
Descriptive statistics that included the mean, standard deviation, and minimum and maximum values were calculated for each of the 2 test groups.
The Student t test was used to determine whether significant differences were present in the bond strength between the 2 groups. The chi-square test was also used to determine significant differences in the ARI scores between the groups. For the statistical analysis, ARI scores of 0 and 1 and of 2 and 3 were combined. Significance for all statistical tests was predetermined at a probability value of .05 or less.
Results
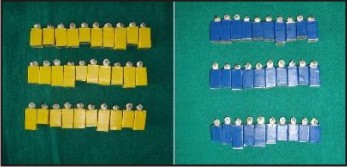
The descriptive statistics for the shear bond strengths of the 2 groups are presented in (Table I).
 | Table I – Descriptive Statistics And Results Of Student T Test That Compared Shear Bond Strengths In Megapascals (MPa) Of The 2 Groups.
 |
the results of the Student t test indicated that the shear bond strength when warm air was used was significantly higher (P= 0.0000; mean= 16.4 ± 2.48 MPa) than when normal temperature compressed air was used (mean= 13.1 ± 1.82 MPa).
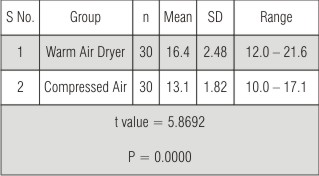
The results of the chi-square comparisons for ARI indicated no significant difference (P=0.5626) between the 2 groups. With the use of warm air, there was a higher frequency of ARI scores of 3, which indicated more composite remained on the teeth (Table II).
 | Table II – Frequency Distribution Of The ARI Scores And The Result Of The Chi-square Comparisons Between The 2 Groups
 |
Discussion
The mechanical properties of composites have been extensively researched in the laboratory, but the clinical situation has not been accurately replicated.14 Some researchers have suggested that this is the result of changes that occur because of exposure to the oral environment.15-19 Biodegradation is the result of a combination of disintegration and dissolution in saliva, chemical and physical degradation, wear caused by chewing food, erosion by the food itself, and bacterial activity.20 Øilo20 reviewed the degradation of composite materials in the mouth and stated that it is such a complex interaction of processes that it cannot be reproduced in vitro. Despite this, the majority of research into dental composites continues in vitro because it is difficult to expose the materials to (and retrieve them from) the oral environment without interfering with the environment itself or taxing the compliance of subjects.
One approach to this problem is to investigate materials with teeth that have already been designated for removal, such as premolars in an orthodontic patient. A material can be applied to a tooth and left in situ for a predetermined time; the tooth can then be extracted, ideally with as little disruption to the material as possible, allowing experiments to be carried out on the material. Technically, the experiments are ex vivo, but the tooth experiences all the in vivo conditions until removal. This approach has been used earlier21 and the same approach was used in the present study.
The bond strength of composite resin to teeth is reported to be weakened by the presence of moisture.22-25 However, the study of Ichiki et al26 found that the bond strength to etched enamel was independent of air drying duration and that a drying time of 5 seconds would be sufficient to dry the etched tooth for bonding.
Higher shear bond strengths were obtained with the warm air dryer compared with the conventional air syringe in the present study. This difference may be due to residual tooth heat that facilitated the polymerization of the bonding agent and/or composite resin. Another possible reason could be due to the effect of warm air on the patient’s breath. Warm air could dry out the humidity from the patient’s exhaled air, thus preventing possible moisture contamination of the bonding agent and/or composite resin. This effect obviously cannot be appreciated in an in vitro study.
The chi square comparison between the ARI values of the 2 groups did not return a significant difference but the stereomicroscopic photographs revealed primarily cohesive failures in the experimental group. This indicates that the bonding of the bonding agent to the tooth was not the weak link in the system, but, instead the strength of the resin itself or the bond of the bonding agent to the filled resin was at fault. On one hand this signifies a stronger bond between the adhesive and the tooth surface. But on the other hand it also points towards the need to remove the remnant adhesive which remains on the tooth surface after debonding the bracket. This carries the risk of removing some healthy tooth structure along with additional chair time.
Conclusion
It can be concluded from the present study that warm air-drying after enamel etching significantly improves shear bond strength compared to conventional air-drying using a dental 3-way syringe. The results are similar to some of the previous studies.6, 27, 28 The ARI scores also signify a cohesive failure. So the usage of warm air can effectively prepare the tooth surface for bonding of orthodontic brackets and is a simple and reliable solution to drying problems. It also provides more comfort for the patient by producing a gentle flow of warm air.
References
1. Iwami Y, Yamamoto H, Kawai K, Ebisu S. Effect of enamel and dentin surface wetness on shear bond strength of composites. J Prosthet Dent 1998 Jul; 80(1):20-6.
2. A. Mavropoulos, A. Karamouzos, G. Kolokithas, and A. E. Athanasiou. In vivo evaluation of two new moisture-resistant orthodontic adhesive systems: a comparative clinical trial. J Orthod., June 1, 2003; 30(2): 139 - 147.
3. Littlewood SJ, Mitchell L, Greenwood DC, Bubb NL, Wood DJ. Investigation of a hydrophilic primer for orthodontic bonding: an in vitro study. J Orthod. 2000 Jun; 27(2):181-6.
4. Cooley RL, Young JM, Train TE. Evaluation of an air operated tooth dryer. Quintessence Int 1989; 20: 577-88.
5. Batchelder KF, Richter RS, Vaidyanathan TK. Clinical factors affecting the strength of composite resin to enamel bonds. J Am Dent Assoc. 1987 Feb; 114(2):203-5.
6. Galan D, Williams PT, Kasloff Z. Effect of warm-air drying and spreading on resin bonding. Am J Dent. 1991 Dec; 4(6): 277-80.
7. Peter G Mouser. A technique for direct bonding of unerupted teeth as an aid to orthodontics. Aust Dent J 1980; 25(3): 121-4.
8. F. Heravi, R. Naseh. A comparative study between bond strength of rebonded and recycled orthodontic brackets. Dent Res J 2006; 2(2):
9. K S Coups-Smith, P E Rossouw, K C Titley. Glass Ionomer Cements as luting agents for orthodontic brackets.Angle Orthod 2003; 73: 436–444.
10. G J Ward, E Mizrahi, P E Cleaton-Jones. Electrothermal bonding: shear bond strength of orthodontic brackets after two weeks. British journal of orthodontics 1998; 25: 123-6.
11. T Yamada, D C Smith, R Maijer. Tensile and shear bond strengths of orthodontic direct-bonding adhesives. Dent Mater 1998; 4(5): 243-50.
12. D R Beech, T Jalaly. Clinical and laboratory evaluation of some othodontic direct bonding systems. J Dent Res 1981; 60: 972.
13. Artun J, Bergland S. Clinical trials with crystal growth conditioning as an alternative to acid etch enamel treatment. Am J Orthod 1984; 85: 333-40.
14. Sunna S, Rock WP. Clinical performance of orthodontic brackets and adhesive systems: a randomized clinical trial. Br J Orthod 1998; 25: 283-7.
15. So¨derholm K-JM, Mukherjee R, Longmate J. Filler leachability of composites stored in distilled water or artificial saliva. J Dent Res 1996; 75: 1692-9.
16. Matasa CG. Microbial attack of orthodontic adhesives. Am J Orthod Dentofacial Orthop 1995; 108: 132-41.
17. Munksgaard EC, Freund M. Enzymatic hydrolysis of (di)methacrylates and their polymers. Scand J Dent Res 1990; 98: 261-7.
18. Lee S-Y, Greener EH, Menis DL. Detection of leached moieties from dental composites in fluids simulating food and saliva. Dent Materials 1995; 11: 348-53.
19. Meng CL, Wang WN, Tarng TH, Luo YC, Lai JS, Arvystas MG. Orthodontic resin under water immersion. Angle Orthod 1995; 65:209-14.
20. Øilo G. Biodegradation of dental composites/glass ionomer cements. Adv Dent Res 1992; 6: 50-4.
21. Rezk-Lega F, Øgaard B, Arends J. An in vivo study on the merits of two glass ionomers for the cementation of orthodontic bands. Am J Orthod Dentofacial Orthop 1991; 99: 162-7.
22. Vicente A, Mena A, Ortiz AJ, Bravo LA. Water and saliva contamination effect on shear bond strength of brackets bonded with a moisture-tolerant light cure system. Angle Orthod. 2009 Jan; 79(1): 127-32.
23. Zeppieri IL, Chung CH, Mante FK. Effect of saliva on shear bond strength of an orthodontic adhesive used with moisture-insensitive and self-etching primers. Am J Orthod Dentofacial Orthop. 2003 Oct; 124(4): 414-9.
24. Cacciafesta V, Sfondrini MF, De Angelis M, Scribante A, Klersy C. Effect of water and saliva contamination on shear bond strength of brackets bonded with conventional, hydrophilic, and self-etching primers. Am J Orthod Dentofacial Orthop. 2003 Jun; 123(6): 633-40.
25. Webster MJ, Nanda RS, Duncanson MG Jr, Khajotia SS, Sinha PK. The effect of saliva on shear bond strengths of hydrophilic bonding systems. Am J Orthod Dentofacial Orthop. 2001 Jan; 119(1): 54-8.
26. Ichiki K, Fukushima T, Yoshida Y et al. Corelation between air-drying duration and bond strength of composite resins to teeth. J Prosthet Dent 1990; 63: 525-9.
27. S M Dunne, B J Millar, B Davies. A survey of dental airlines and an examination of tooth-drying techniques. Prim Dent Care 1996; 3(2): 61-4.
28. James D Allen, Larry C Breeding, David H Pashley. Effect of warm air on the shear bond strength of composite resins. Quintessence Int 1992; 23: 289-96. |