Introduction
The hard dental tissues including enamel, dentin and cementum, are critical to the integrity of the dentition. Loss of these tissues can have significant consequences for the patient. Tooth wear refers to gradual loss of dental hard tissues by a disease process other than dental caries. Attempts have been made to distinguish between pathological and physiological loss of tooth tissues (1, 2).Tooth wear can be regarded as pathological if the teeth become so worn that they do not function effectively or seriously mar the appearance before they are lost for other causes. Tooth wear is mostly result of three processes: abrasion, attrition and erosion. A further process (abfraction) might potentiate wear by abrasion and/or erosion. Tooth wear in an individual is likely to be multifactorial as individual wear mechanisms rarely act alone but interact with each other. However, in recent years the contribution of erosion to tooth wear is increasing due to change in lifestyle and eating habits (1). Epidemiological data, and studies in vitro and in situ, suggest that, of the three individual wear processes, erosion is the most common threat for tooth surface loss (2,3,4).
Multifaceted nature of tooth tissue loss in non carious conditions
There are various forms of non-caries destructive processes leading to a loss of tooth structure. These include abrasion, demastication, attrition, erosion, abfraction, and resorption. Non-caries tooth structure loss is almost never caused by any one of the above processes alone. A brief overview of these will help in further understanding-
Abrasion: Term 'abrasion' is derived from the Latin verb abrader, abrasi, abrasum (to scrape off) and describes the wearing of a substance or structure through mechanical processes, such as grinding, rubbing and scraping (5). Dental abrasion is a pathological wearing of teeth resulting from abnormal mechanical processes involving foreign objects or substances repeatedly introduced in the mouth and contacting the teeth. The main etiological factors are oral hygiene procedures.
1. Brushing: aggressive horizontal brushing, use of hard bristles, force and time spent on brushing, tooth brush design, length, number, and diameter of tufts.
2. Dentifrices: type of dentifrice ie powder or paste, size and hardness of the particle, ph and amount of dentifrice used.
3. Use of excessive dental floss, tooth picks or interdental brushes causes proximal abrasion.
Other factors include occupational habits like placement of pins or nails between teeth or holding pipe stem between teeth. Tooth brush abrasion is most common form of abrasion and is usually seen as a sharp, V-shaped notch in the cervical third of the facial aspect of teeth.
Demastication: A special form of abrasion is demastication describes the wearing away of tooth substance during the mastication of food with the bolus intervening between opposing teeth (5). Abrasion is mainly on the occlusal side and is influenced by the individual food. Most of the wear is physiological but become pathological if patient is habitual of eating very hard substances like beetle nut.
Attrition: Term 'attrition' is derived from the Latin verb atterere, attrivi, attritium, describing the action of rubbing against something (5). Attrition in dentistry is physical wear of teeth as a result of contact of teeth with each other with no foreign substance intervening. Although physiological as teeth come in contact with each other during function but becomes abnormal if patients have parafunctional movements like bruxism. Normal physiological attrition is usually present on occlusal surfaces with a characterstic feature of antagonistic plane facets and sharp margins, enamel and dentin usually wear at same rate (6). Attrition also includes proximal surface wear at the contact area because of physiological tooth movement.
Abfraction: Term 'abrasion' is derived from the Latin verb frangere, fregi, fraction (to break) is used to describe a special form of wedge shaped defects at the cementoenamel junction of a tooth (5). Abfraction is a loss of tooth surface at the cervical areas of teeth caused by tensile and compressive forces during tooth flexure. These forces are focussed on the CEJ where they provoke microfracture in enamel and dentin. The weakened cervical region would then be susceptible to abrasion and erosion (7, 8). Abfaction usually involve single tooth with excrusive interferences or eccentric occlusal loads and appear as wedge shaped defects having sharp rims at CEJ.
Erosion: Term 'erosion, is derived from the Latin verb erodere, erosi, erosum (to gnaw, to corrode), describes the process of gradual destruction of the surface of something usually by electrolytic or chemical processes (5). Dental erosion is defined as the progressive, irreversible loss of hard dental tissues due to a chemical process not involving bacteria (9, 10). The acids responsible for erosion are not products of the intraoral flora; they stem from dietary, occupational or intrinsic sources.
Resorption: Resorption is the process of biological degradation and assimilation of substances or structures previously produced by the body. In dental terms, it refers to the biological removal of dental hard tissue by cementoclastic, dentinoclastic and ameloclastic activity. This can be either a physiological process, as in the case of root absorption of deciduous teeth, or a pathological process such as resorption owing to trauma, cysts or neoplasms. Resorption is of no relevance in the context of erosion which occurs at the surface of a tooth, but in the context of differential diagnosis it cannot be omitted from the list of non-carious destructive processes.
Mechanism:
Tooth erosion is a multifactorial condition and has a complex aetiology. Every factor plays a role in inducing or preventing erosion. Over time, the interaction of all these factors may lead to either progression or protection of the surface. Dental hard tissues are largely composed of mineral crystals of hydroxyapatite with the formula Ca10(PO4)6(OH)2. Dental hydroxyapatite (HAP) is often described as "calcium deficient" and "carbonated" because some calcium ions may be substituted by sodium, magnesium and potassium, and some phosphates (PO4) by carbonates (CO3) (11). Because of these substitutions the mineral in enamel and dentin is much more acid soluble than HAP which in turn is much more soluble than fluorapatite (FAP) which has the formula Ca10 (PO4)6F2 (12). Dentin and enamel have similar mineral compositions, although the carbonate content of enamel is approximately 3% while in dentine it is 5-6%, making dentin mineral even more acid soluble (11). Chemical erosion of the teeth occurs either by the hydrogen ion derived from strong/weak acids, or by anions which can bind or complex calcium (chelators). The hydrogen ions, H+, are derived from acids as they dissociate in water and H+ ion itself can attack the tooth mineral crystals and directly dissolve by combining with either the carbonate ion or the phosphate ion, as shown in equation (11).
Ca10-x Nax (Po4)6-y (Co3)z (OH)2-u Fu +3H+
-------------->
(10-x) Ca+2 + xNa+ + (6-y) (HPO4-2) + z(HCO3-) + H2O +uF-
The effect of direct attack by the hydrogen ion is to combine with the carbonate and/or phosphate releasing all of the ions from that region of the crystal surface leading to direct surface etching.
Depending on the ph and duration of exposure of chemicals having acidic ph there can be either direct removal of hard tissue by complete dissolution or creation of a thin softened layer few millimetres below the surface: a process known as softening (1,13). This softened layer is vulnerable to subsequent mechanical wear or further progress in softening causes its complete dissolution (14). In dentin exposed to acid there is first dissolution at the junction of the peritubular and intertubular dentin, then loss of the peritubular dentine and widening of the tubule lumina (15) and finally formation of a superficial layer of demineralised collagenous matrix (16. While it persists, this layer might mechanically protect the underlying residual dentin and might also affect chemical reactions between the latter and the oral fluids, but it is itself vulnerable to mechanical and proteolytic damage and will ultimately be lost (1,17). Normal tooth brushing scarcely abrade the normal enamel but it becomes vulnerable to tooth brush abrasion and even friction of tongue after acidic attack (18,19,20,21). Similarly softened dentin is also susceptible to mechanical wear (18, 22). Thus acid attack to enamel and dentin make them more vulnerable and other tooth wear process like attrition and abrasion become more severe.
Types of erosion : Tooth erosion can be extrinsic ,intririsic , or idiopathic.
Extrinsic erosion: Extrinsic erosion is the result of exogenous acids. Dietary acids, however, are the principal causative factor for extrinsic tooth erosion (5,10,18). Other important factors include oral administration of some medicines-such vitamin C preparations, acid used to dissolve smallrenal calculi and iron tonics. Occupational exposure due to industries, swimming pools, wine tasters etc (5).
The most frequently consumed erosive acids are fruit acids and phosphoric acid contained in fresh fruits, fruit juices and soft drinks (5,6). Most fruits and fruit juices have a very low pH (high acidity) as shown in table (23, 24).
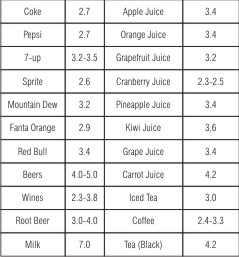 | Table 1. Common Beverages and Juices pH (23,24).
 |
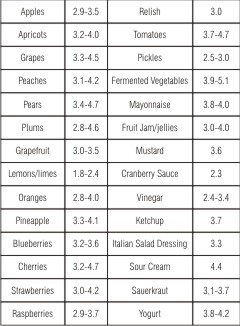 | Table 2. Common Food Stuffs and Their pH (23,24)
 |
This finding is of concern, particularly since children and adolescents are the primary consumers of these drinks (25,26). The erosive potential of beverages does not depend on pH alone (27, 28) and pH is not a direct indicator of erosive potential, as other chemicals accompanying the strong acid in a particular exogenous product may modify the erosive potential. Yoghurt is one of the products with pH around 4.0 but no evidence of causing erosion for most people. This is likely to be because of the high concentration of calcium and phosphate ions present, inhibiting the erosive demineralisation of apatite through the 'common ion effect'. So other components of beverages, such as calcium, phosphates, and fluoride, may lessen erosive potential. Also, factors such as frequency and method of intake of acidic beverages as well as proximity of tooth brushing after intake may influence susceptibility to erosion. For example, drinking through a straw lessens the contact time of the beverage with the teeth compared to drinking from a cup.
Intrinsic erosion: Intrinsic erosion is the result of endogenous acid, or gastric acid contacting the teeth during recurrent vomiting, regurgitation or reflux. Unlike dietary acids, the pH and titratability of gastric juice is significantly greater and so the level of destruction is normally more severe (29). The pH of gastric acid is around 1.2, and the pH of exogenous acids vary between 2.5 - 4.0. Eating disorders of psychosomatic origin such as nervous vomiting, anorexia nervosa or bulimia are often the cause of regurgitation or vomiting, which in these cases is self-induced. Causes of somatic origin include pregnancy, alcoholism, Disulfiram treatment for alcoholics and gastrointestinal disorders such as gastric dysfunction, chronic obstipation(a condition of extreme and persistent constipation caused by obstruction in the intestinal system), hiatus hernia, duodenal and peptic ulcer and gastro-oesophageal reflux disease (GORD or GERD).
Due to its profound effect on erosion Gastro-oesophageal reflux disease (GORD) warrants additional mention. GORD is a common condition, estimated to affect 7% of the adult population on a daily basis and 36% at least one time a month (30). Reflux is the passive or effortless movement of regurgitated acid into the mouth. This is caused by increased abdominal pressure, inappropriate relaxation of the lower esophageal sphincter or increased acid production by the stomach (31). Signs and symptoms associated with reflux are heartburn, retrosternal discomfort, epigastric pain and dysphasia. However, symptoms are not reliable indicators of the presence or absence of GORD. Patients may be symptom free despite continuation of reflux and are described as silent refluxers (32) and dental erosion may be the only clinical sign that reflux is occurring. Excessive intake of alcohol, carbonated drinks and certain foods such as spicy food, and fatty food can provoke GORD. Alcohol can result in gastritis and provoke GORD. Alcoholics also have poor diet control and tend to eat more acidic foods and drinks. Neurologically impaired children have significantly higher levels of gastric reflux than healthy children with over 70% of children with cerebral palsy having abnormal reflux activity (33).
Idiopathic erosion is the result of unknown origin, i.e. an erosion-like pathology where neither tests nor anamnesis are capable of providing an etiologic explanation.
Factors involved on progression or arrest of erosion: Biological factors and behavioural factors have major influences on the progress or arrest of erosion. Biologic factors incudes saliva, tooth composition and structure, dental anatomy, occlusion and the anatomy of soft tissues in relation to the teeth, physiological soft tissue movements such as swallowing pattern.
Saliva: Salivary function is an important factor in the etiology of erosion. The erosive effects of acids are exacerbated by decreased salivary gland function. Saliva is a significant factor in the prevention of dental erosion since it helps to directly neutralize and clear acids, as well as forming a protective coat over the teeth and promoting remineralization. Buffering capacity of saliva refers to its ability to resist a change in pH when an acid is added to it. This property is largely due to the bicarbonate content of the saliva which is in turn dependent on salivary flow rate. Patients with erosion were found to have lower salivary buffer capacity when compared with controls in several studies (34,35,36,37) The pellicle is derived from specific salivary proteins and lipids that bind to the surface of the tooth (38, 39). Pellicle forms a diffusion barrier, similar to a lipid/protein membrane, and protects the very outer surface against direct acid attack. The plaque bacteria build upon the pellicle, forming a further diffusion barrier. On smooth accessible surfaces there is often little or no plaque leaving only the pellicle as the first barrier to acid erosion. At the gingival margin there is almost always plaque and crevicular fluid access thereby protecting a narrow band from erosion.
Tooth composition and structure: The composition of human teeth is known to be highly variable with respect to trace element concentrations and clinical studies have shown marked differences in the response of various human teeth to acidic beverages.
Dental anatomy, occlusion and the anatomy of soft tissues in relation to the teeth: The shape and contour of teeth and their prominence in the mouth relative to drinking identified as factors that may modify the erosion process. Acid-eroded enamel is considered more susceptible to attrition, and thus, dental occlusion is likely to play an important role in the manifestation of erosion-induced tooth wear patterns. Conversely, tooth wear, primarily caused by parafunctional habits such as bruxism, will be greatly accelerated in the presence of an erosive challenge to the teeth.
Anatomy of the soft tissues and physiological soft tissue movement: The anatomy of oral soft tissues in relation to the teeth and physiological soft tissue movements will influence the tooth sites that acidic substances will contact and will influence the clearance pattern of acidic substances from the mouth. Friction from the tongue even can cause erosion.
Behavioural factors: Behaviour can be strongly influenced by socio-economic status. Some studies have indicated that people involved in strenuous exercise may be at risk of dental erosion because of their more frequent ingestion of acidic sports drinks, fruit juices and other acidic beverages. Ironically, healthier diets including the consumption of more fruits and vegetables may be an important factor in the aetiology of dental erosion. As a matter of fact lactovegetarian diet has been associated with a higher prevalence of dental erosion. Further, individuals with eating disorders such as anorexia nervosa and bulimia may compound their erosion risk from regurgitation with the consumption of large quantities of fruits, juices and carbonated soft drinks in addition to wilfully purging ingested food.
Diagnosis of erosion
Detailed familiarity with the current understanding of dental erosion etiology and a differential diagnosis are critical before any dietary or behavioral pattern can be associated with the observation of tooth structure loss.
Medical history must include information regarding any systemic conditions that influence the salivary flow, use of any chronic medication, gastric reflux, heartburn, acid mouth taste frequent vomiting and so forth. A thorough case history may involve consultation with the patient's physician.
Since high intake of acidic foods and beverages have been strongly associated with erosion. Therefore a thorough diet record of each and every patient must be noted down. Detailed information regarding oral hygiene practices must be noted including method, types and frequency.
Dental history regarding jaw parafunction and bruxism should also be taken. Patient's occupation and recreational habits must also be recorded in the history.Intraoral photographs for documentation and study models to monitor progression are equally necessary. Salivary tests including unstimulated and stimulated flow rate as well as buffering capacity should be performed. A thorough case history will also undoubtedly involve consultation with the patient's physician
Clinical appearance
Erosive lesions can appear on any surface depending on the area of tooth that comes directly under the acidic attack. For example patient suffering from GORD, palatal surface of upper anterior teeth is most commonly involved, sucking a lemon against anterior teeth will involve facial surfaces.
Dental erosion must be distinguished from other forms of wear, as it contribute to general tissue loss by surface softening, thus enhancing physical wear processes. Loss of shine or luster of enamel and appearance of glazed surface are early signs of erosion. Further attack leads to flattening of convexities of teeth, cusps become more rounded and overall appearance of teeth becomes more flattened. Edges of restorations may appear to rise above the level of the adjacent tooth surfaces. Appearance of concavities on the smooth surfaces, grooving or cupping occur on incisal/occlusal surfaces with discrete areas of exposed dentine, which increase in area as the erosion progresses.There may also be incisal chipping and teeth may appear darker as dentine is exposed and increase in enamel translucency at incisal edges.In severe cases, the whole tooth morphology disappears and the vertical crown height can be significantly reduced. Depending on severity hypersensitivity appear as first symptom to patients, further tooth loss can even cause pulp exposures.
The concavities must be differentiated from the wedge shaped defects caused by abrasion which have sharp margins and cuts at right angle into the enamel and their depth clearly exceeds the width while concavities of erosive lesions are more wide compared to their depth with indulating borders. A typical appearance of erosive lesion is appearance of chamfered enamel margin coronal to CEJ ie presence of intact enamel along the ingival margin. The preserved enamel margin may be due to presence of plaque which act as diffussion barrier and also the neutralization of acid by sulcular fluid having ph betweeen 7.5-8.0.
Management of erosion: A complete clinical management involves the identification of cause for erosion, preventive management and restorative management. Identification of the etiology is important as a first step in management of erosion. A detailed questionnaire should be asked to patient to identify the etiologic factors. Refer patients or advise them to seek appropriate medical attention when intrinsic causes ie GORD, vomiting, or salivary dysfunction are involved. If excessive dietary intake of acidic foods or beverages is discovered, patient education and counseling are important.
Since erosion, attrition and abrasion often occur simultaneously all causative components must be taken into consideration when planning preventive strategies. Preventive programmes comprise of dietary advice, fluoride regimes, stimulation of salivary flow rate, use of buffering medicaments and correct use of oral hygiene products.
Dietery advise include indentification of acidic food in patient diet, their amount and frequency. Acidic drinks should be drunk quickly rather than sipped and use of straw is beneficial and should not be hold or swished in mouth.
Toothbrushing should be delayed for at least 20 minutes after an erosive attack and possibly up to 60 minutes because of the increased risk of abrasive wear on the softened/eroded surface (40,41) Instead use of fluoride mouth rinse, baking soda solution or simply rinsing with water is better.
Avoidance of acidic food and drink between meals, at bedtime and during the night is highly recommended. Milk related products have ph close to normal and should be preferred compared to soft drinks. Finishing a meal with milk or cheese is also useful as this will help bring the oral environment back to a neutral ph (42) Patient should be instructed to use appropriate oral hygiene techniques like use of a soft toothbrush and low abrasion fluoride containing toothpaste as high abrasive toothpastes may destroy the pellicle (43). Toothpastes or mouthwashes with a too low pH should be avoided. Fluoride mouth rinses, varnishes and desensitising agents aids in remineralisation and decrease sensitivity (44, 45). Fluoride application 2-4 times by dentist and use of topical fluoride at home by patient is recommended. The application of concentrated topical fluoride gels and varnishes before the erosive challenge is likely to take place was found experimentally to provide some inhibition of demineralisation of both roots and crowns (46). Recent laboratory and clinical studies have shown that toothpaste containing 5000 ppm fluoride was signifcantly more efective than one containing 1450 ppm fluoride in reducing enamel loss caused by orange juice (47,48).
Saliva provides buffering capacity that resists acid attacks. This buffering capacity increases with salivary flow rate. Saliva is also supersaturated with calcium and phosphorus, which inhibits demineralization of tooth structure. Stimulation of salivary flow by use of a sugarless lozenge, candy or gum is recommended. the use of a non-acidic sugar-free lozenge may be more advisable, since gum chewing may have an abrasive effect on softened tooth structure. Neutralize acids in the mouth by dissolving sugar-free antacid tablets 5 times a day, particularly after an intrinsic or extrinsic acid challenge. Consider application of composites and direct bonding where appropriate to protect exposed dentin (49).
Use of protective devices. Insertion of a close fitting occlusal guard at high risk times such as during sleeping (for GORD patients), swimming in poorly maintained swimming pool (for professional swimmers) or voluntary vomiting (for anorexia/bulimia patients)may be considered.
Restorative management
The longevity of dental restorations depends on the durability of the material per se and its wear resistance (8), the durability of the interface between tooth substance and restoration, the level of tooth destruction, its location and load.
Under acidic conditions all dental restorative materials show a degradation over time (surface roughness, decrease of surface hardness, substance loss). However, it seems that ceramic and composite materials show a good durability. Conventional glass-ionomer cements are not recommended as permanent restorations because of their disintegration in acidic conditions (38).
In past the severely eroded dentition was usually rehabilitated by the provision of extensive crown and bridge work or removable overdentures. However due to improvements in composite restorative materials, and in adhesive techniques, it has become possible to rehabilitate mild and moderate eroded dentitions in a less invasive manner and the use of modern direct restorative materials can provide excellent longevity, even in load-bearing situations (52,53). The advantage of direct composite restorations is that they are adaptable to the defect and repair is straightforward. Several case reports demonstrate the successful rehabilitation of (erosive) worn dentitions using adhesive techniques (54-56).The restorative treatment plan should be adapted to the degree of tooth substance loss e.g. loss of vertical dimension. These options also include cast alloy restorations for palatal and occlusal erosion, sandblasted nickel-chromium alloys or heat treated gold are usually used where aesthetics is not important. The castings can be cemented with a resin based material that can bond to both metal oxide and tooth surface.
Initially, erosive tooth wear limited to the enamel can be restored with direct composites or in more advanced cases, porcelain veneers can be considered as treatment of choice. Restorations inserted in this stages not only fulfil the esthetic needs but also prevent further progression of erosive leasions and take care of any hypersensitivity present.
However cases of advanced erosion poses a problem for their reconstruction as there is not enough space for the restorative material on the occlusal side. As long as there is only a loss of 1-2mm of interocclusal space, the teeth can be reconstructed directly with composite materials (57). Patients tolerate such a small increase in the vertical dimension usually without any problem. However further loss of interocclusal space may require more extensive treatment however to prevent an invasive, full mouth rehabilitation, it can be convenient to gain interocclusal space with orthodontic measures, especially if mainly groups of teeth (e.g. all teeth in the anterior region) are involved in erosive tooth wear. The orthodontic treatment can be achieved with fixed or removable appliances, such as the Dahl appliance (57,58). Following orthodontic treatment, the eroded teeth can then be reconstructed (57, 59).
However if extensive tooth tissue loss is present, occlusal reconstruction may be necessary, particularly for older patients. Endodontic and periodontic therapy, surgical crown lengthening, placement of foundations, and orthodontic repositioning of the teeth may be required before crowns and other prostheses can be constructed. An acrylic full arch maxillary splint or nightguard may be needed to limit the adverse effects of concomitant tooth grinding once restorative treatment is complete.
Recall and maintenance care
Failure to monitor the patient may result to relapse of condition, therefore it is essential that a recall care regime matched to the patient's requirements should be established, to check patient compliance, monitor wear, reinforce advice, and for encourage to maintain changed behaviour. it is important to combine active treatment with preventive measures and recall at regular intervals to ensure the long-term success.
Conclusion
Tooth wear and erosion are modern day problems for dentistry. Early diagnosis and accurate detection of possible risk factors including their interplay are essential to halt the process of tooth wear. Long-term success is only possible when the cause is eliminated. An incorrect diagnosis regarding the contributions of abrasion, attrition, abfraction and erosion to specific lesions will result in inappropriate or ineffective treatment. Due to its major impact on tooth wear, management of erosion is becoming increasingly significant in the long-term maintenance of the dentition . Such management indeed is complex and may require interdisciplinary long-term strategy including liaison with physicians.
References:
1. Lussi A. Dental Erosion: From diagnosis to therapy. Monographs Oral Sci. 2006; vol 20.
2. Smith BG, Knight JK: An index for measuring the wear of teeth. Br Dent J 1984;156:435-438.
3. Nunn JH: Prevalence and distribution of tooth wear; in Addy M, Embery G, Edgar WM, Orchardson R (eds): Tooth Wear and Sensitivity. London, Martin Dunitz, 2000, pp 93-104.
4. Zero DT, Lussi A: Etiology of enamel erosion: intrinsic and extrinsic factors; in Addy M, Embery G, Edgar WM, Orchardson R (eds): Tooth Wear and Sensitivity. London, Martin Dunitz, 2000, pp 121-140.
5. Imfeld T: Dental erosion. Definition, classification and links. Eur J Oral Sci 1996;104:151-155.
6. Gandara BK, Truelove EL. Diagnosis and management of dental erosion. J Contemp. Dent. Prac. 1999;1(1):1-17.
7. Grippo JO: Abfractions: a new classification of hard tissue lesions of teeth. J Esthet Dent 1991;3:14-19.
8. Grippo JO, Simring M, Schreiner S: Attrition, abrasion, corrosion and abfraction revisited. J Am Dent Assoc 2004;135:1109-1117.
9. Pindborg JJ. In: Pathology of Dental Hard Tissues. Copenhagen: Munksgaard 1970:312-321.
10. Eccles JD. Dental Erosion and Diet. J Dent 1974;2:153-159.
11. Featherstone JDB: The science and practice of caries prevention. J Am Dent Assoc 2000;131:887-899.
12. Featherstone JDB, Lussi A. Understanding the chemistry of dental erosion. In Lussi A (ed). Dental Erosion: From diagnosis to therapy. Monographs Oral Sci. 2006;2006;20:66-76.
13. Koulourides T: Experimental changes of mineral density; in Harris RS (ed): Art and Science of Dental Caries Research. New York, Academic Press, 1968, pp 355-378.
14. Eisenburger M, Hughes J, West NX, Jandt K, Addy M: Ultrasonication as a method to stud enamel demineralization during acid erosion. Caries Res 2000;34:289-294.
15. Meurman JH, Drysdale T, Frank RM: Experimental erosion of dentine. Scand J Dent Res 1991;99:457-462.
16. Kinney JH, Balooch M, Haupt DL, Marshall SJ, Marshall GW: Mineral distribution and dimensional changes in human dentine during demineralization. J Dent Res 1995;74:1179-1184.
17. Hunter ML, West NX, Hughes JA, Newcombe RG, Addy M: Relative susceptibility of deciduous and permanent dental hard tissues to erosion by a low pH fruit drink in vitro. J Dent 2000;28:265-270.
18. Davis WB, Winter PJ: The effect of abrasion on enamel and dentine after exposure to dietary acid.Br Dent J 1980;148:253-256.
19. Attin T, Koidl, Buchalla W, Schaller HG, Kielbassa AM, Hellwig E: Correlation of microhardness and wear in differently eroded bovine dental enamel. Arch Oral Biol 1996;42:243-250.
20. Jaeggi T, Lussi A: Toothbrush abrasion of erosively altered enamel after intraoral exposure to saliva: an in situ study. Caries Res 1999;33:455-461.
21. Eisenburger M, Shellis RP, Addy M: Comparative study of wear of enamel induced by alternating and simultaneous combinations of abrasion and erosion in vitro. Caries Res 2003;37:450-456.
22. Attin T, Buchalla W, Putz B: In vitro evaluation of different remineralization periods in improving the abrasion resistance of previously abraded bovine dentine against tooth-brushing abrasion. Arch Oral Biol 2001;46:871-874.
23. Clark DC, Woo G, Silver JG, Sweet D, Grisdale JC. The infuence of frequent ingestion of acids in the diet on treatment for dentin sensitivity. J Can Dent Assoc. 1990 Dec;56(12):1101-3.
24. Lussi A, Jaeggi T. Chemical factors in Lussi A (ed). Dental Erosion: From diagnosis to therapy. Monographs Oral Sci. 2006;20:77-87.
25. Asher F, Read MJF. Early enamel erosion in children associated with excessive consumption of citric acid. Br Dent J 1987;162:384-87.
26. Millward A, Shaw L, Smith AJ, et al. The distribution and severity of tooth wear and the relationship between erosion and dietary constituents in a group of children. Int J Paediatr Dent 1994;4:151-57.
27. Grenby TH, Phillips A, Desai T, et al. Laboratory studies of the dental properties of soft drinks. Br J Nutr 1989;62:451-464.
28. Grenby TH. Lessening dental erosion potential by product modification. Eur J Oral Sci 1996;104:221-228.
29. Bartlett DW, Coward PY: Comparison of erosive potential of gastric juice and a carbonateddrinkin vitro. J Oral Rehabil 2001;28:1045-1047.
30. Nebel OT, Fornes, MF and Castell DO. Symptomatic gastroesophageal reflux: incidence and precipitating factors. Am J Dig Dis 1976; 21:953-956.
31. Gaynor MD. Otolaryngologic manifestations of gastroesophageal reflux. Am J Gast 1991;86:801-808.
32. Bartlett DW, Evans DF, Anggiansah A, et al. A study of the association between gastro-oesophageal reflux and palatal dental erosion. Br Dent J 1996; 181:125-131.
33. Reyes AL, Cash AJ, Green SH and Booth IW. Gastro-oesophageal reflux in children with cerebral palsy. Child: care, health and development 1993;19: 109-118.
34. Meurman JF, Toskala J, Nuutinen P, et al. Oral and dental manifestations in gastroesophageal reflux disease. Oral Surg Oral Med Oral Pathol 1994; 78:583-589.
35. Gudmundsson K, Kristleifsson G, Theodors A, et al. Tooth erosion, gastroesophageal reflux, and salivary buffer capacity. Oral Surg Oral Med Oral Pathol 1995;79:185-189.
36. Bevenius J, L'Estrange P. Chairside evaluation of salivary parameters in patients with tooth surface loss: a pilot study. Aust Dent J 1990;35:219-221.
37. Johansson A, Kiliaridis S, Haraldson T, Omar R, Carlsson GE. Covariation of some factors associated with occlusal tooth wear in selected high-wear sample. Scand J Dent Res 1993;101:398-406.
38. Mandel ID: The role of saliva in maintaining oral homeostasis. J Am Dent Assoc 1989;119:298-304.
39. Moreno EC, Kresak M, Hay DI: Adsorption of molecules of biological interest onto hydroxyapatite. Calcif Tissue Int 1984;36:48-59.
40. Davis WB, Winter PJ. The effect of abrasion on enamel and dentine after exposure to dietary acid. Br Dent J 1980; 148: 253-256.
41. Attin T, Knöfel S, Buchalia W, Tütüncü R. In situ evaluation of different remineralisation periods to decrease brushing abrasion of demineralised enamel. Caries Res 2001; 35: 216-222.
42. Gedalia I, Ionat-Bendat D, Ben-Mosheh S and Shapira L. Tooth enamel softening with a cola type drink and rehardening with hard cheese or stimulated saliva in situ. J.Oral Rehab 1991; 18: 501-506.
43. Hunter ML and West NX. Mechanical tooth wear: the role of individual toothbrushing variables and toothpaste abrasivity. In: Tooth Wear and Sensitivity. Eds Addy M, Embery G, Edgar W.M., Orchardson R. Pub. by Martin Dunitz Ltd., 2000.
44. Ganss C, Klimek J, Schäffer U, Spall T. Effectiveness of two fluoridation measures on erosion progression in human enamel and dentine in vitro. Caries Res 2001; 35: 325-330.
45. Pashley D Potential treatment modalities for dentine hypersensitivity: in office products. In: Tooth Wear and Sensitivity. Eds Addy M, Embery G, Edgar W.M., Orchardson R. Pub. by Martin Dunitz Ltd., 2000.
46. Mok TB, McIntyre J, Hunt D.: Dental erosion: in vitro model of wine assessor's erosion. Aust Dent J. 2001;46:263-8.
47. Ren Y-F, Fadel N, Liu X, Malmstrom H. Prevention of dental erosion by 5000 ppm fluoride treatment in situ. J Dent Res. 2010;89(Special Issue B):#2596.
48. Ren Y-F, Zhao Q, Malmstrom H, Barnes V, Xu T. Assessing fluoride treatment and resistance of dental enamel to soft drink erosion in vitro: applications of focus variation 3D scanning microscopy and stylus proflometry. J Dent. 2009;37(3):167-76.
49. Azzopardi A, Bartlett DW, Watson TF and Sherriff M. The surface effects of erosion and abrasion on dentine with and without a protection layer. Br Dent J 2004; 194:351354.
50. Soderholm KJ, Richards ND: Wear resistance of composites: a solved problem? Gen Dent 1998;46:256-263.
51. Yip HK, Lam WTC, Smales RJ: Fluoride release, weight loss and erosive wear of modern aesthetic restoratives. Br Dent J 1999;187:265-270.
52. Gaengler P, Hoyer I, Montag R: Clinical evaluation of posterior composite restorations: the 10-year report. J Adhes Dent 2001;3:185-194.
53. Manhart J, Garcia-Godoy F, Hickel R: Direct posterior restorations: clinical results and new developments. Dent Clin North Am 2002;46:303-339.
54. Hastings JH: Conservative restoration of function and aesthetics in a bulimic patient: a case report. Pract Periodontics Aesthet Dent 1996;8:729-736.
55. Aziz K, Ziebert AJ, Cobb D: Restoring erosion associated with gastroesophageal reflux using direct resins: case report. Oper Dent 2005;30:395-401.
56. Bartlett DW: Three patient reports illustrating the use of dentine adhesives to cement crowns to severely worn teeth. Int J Prosthodont 2005;18:214-218.
57. Jaeggi T, Grüninger A, Lussi A. Restorative Therapy of Erosion in Lussi A (ed). Dental Erosion: From diagnosis to therapy. Monographs Oral Sci. 2006;20:200-214.
58. Dahl BL, Krogstad O: The effect of partial bite raising splint on the occlusal face height. An X-ray cephalometric study in human adults. Acta Odontol Scand 1982;40:17-24.
59. Bartlett DW: The role of erosion in tooth wear: aetiology, prevention and management. Int Dent J2005;4:277-284. |