INTRODUCTION
Postpalatal seal (PPS), also known as the the posterior palatal seal area or the post dam area, is a valve seal area present at the posterior border of the maxillary removable dental prosthesis. The PPS area is defined as the soft tissue area at or beyond the junction of the hard and soft palates on which pressure, within physiologic limits, can be applied by a complete denture to aid in its retention [1].
The first Anatomical land mark of the PPS [2] extends medially from one tuberosity to another. This landmark travels laterally across the hamular notch and anteriolaterally up to a distance of 3.0 to 4.0 mm, to end in the muco-gingival junction of the posterior part of maxillary ridge known as the Pterygo-maxillary seal. At the bony level, the PPS area encompasses horizontal plate of the palatine bone, the maxillary tuberosity and the hamular process of the medial pterygoid plate. The Second land mark contains the two types of imaginary "vibrating lines" across the posterior part of the palate that divide the immovable and the movable tissue of the hard and soft palate. The Anterior vibrating line lay between immovable hard palate tissue and movable the soft palate tissue. It is generally cupid bow-shaped. Posterior vibrating line is located at the junction of the aponeurotic part of the soft palate that shows limited and marked movement. It is usually straight, with a slight curvature anteriorly [2, 3]. The third land mark is fovea palatini. They are two indentations, oval to round in shape, being unique to human race and in 50% cases are located anterior to the anterior vibrating line [4] at a distance of about 1.3 mm. In rest 50% cases, fovea palatini are located either on or behind the anterior vibrating line [5]. Fovea palatine can be used only as a guide for the placement of posterior border of maxillary denture.
The PPS lies between anterior and posterior vibrating line. The preferred Choice of PPS [2, 6, 7, 8, 9] can be a butterfly shaped and continued upto 3.0 to 4.0 mm anteriolareral to the tuberosity, approximating mucogingival junction. The depth of PPS ranges from 1.0 to 1.5 mm. but it should be 0.5 to 1.0 mm at median raphe. Silverman [10] advocated that complete denture could be extended up to an average of 8.2 mm dorsally over to the vibrating flexion line. The relationship between soft palate and hard palate is called palatal throat form [8]. Terrel (Figure 1), [11] advocated a peculiar form of PPS which extends on either side from the posterior palatine area in those soft tissues between the hard palate and base of the alveolar ridge. Terrel referred it, as additional seal palatal seal.
Present article highlights a literature of review and case report onto the posterior palatal seal. This article is linked to the retention and the stability of the maxillary denture which deals with an additional seal.
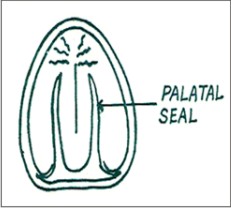 | Figure 1: Additional PPS As Palatal Seal Suggested By Terrel
 |
CASE REPORT
About a few months back, a fifty-year-old female patient was referred to the deptt. of Prosthodontics, by a private practitioner. Patient had a complaint of retention and stability with maxillary complete denture. The Patient suffered edentulism from the last six months. On intraoral examination, she had a U-shaped, medium vaulted and long enough anterio-posterior hard palate and a Class III soft palate with a 70° angle to the hard palate (Figure 2). A Class II palatal throat form was also reported [8]. Authors suggested a short clinical trial as a chair side procedure to enhance the seal area. This was accomplished by an additional reverse palatal seal in the mid line of posterior denture border region.
 | Figure 2: Primary PPS And Additional Reverse Cupid Bow-shaped PPS As A Pink And Violet Band, Respectively
 |
INTRAORAL TECHNIQUE
1. The initial steps for registering the reverse PPS was done through the marking of a band of Gentian violet 1% w/v [12] (Figure 2) over the soft palate beyond the fovea palatini, after drying the mucosa. This area of advocated PPS was performed by asking "ah" in a vigorous manner unless patient felted and initiated gagging reflex. This gave an extended area of PPS. Again, a primary butterfly- shaped PPS was marked by indelible pencil as a pink band.
2. The posterior border of the denture was roughened and prepares a 45-degree bevel joint [13] along with retentive keys. The sticky staged auto polymerizing resin was applied on the bevel joint. Auto polymerizing resin of the dough stage was added centrally and posteriorly to the bevel joint on the posterior border near about a width of a 5.0 to 6.0 mm. The prosthesis was inserted in the patient mouth and the patient asked to perform normal respiratory movements to inhale and to exhale until the material was cured. A light messaging pressure from the first finger was also applied.
3. Polished trial maxillary denture prosthesis had a width up to 2.0 to 5.0 mm which was suggested PPS. It is replica of the Gentian violet band (Figure 3). The patient was examined and reviewed. The result was much satisfactory (Figure
4). Authors gave the prosthesis to the patient and advised for revisit the department after one week for the final replacement of material in the prosthesis. Extended PPS was replaced with light polymerized dual cure denture reline material, intra orally [14].
 | Figure 3: Reverse PPS Over To Complete Denture
 |
 | Figure 4: Upper Maxillary Denture Insertion With Reverse PPS.
 |
DISCUSSION
Trial prosthesis was advised whether the extended PPS would be tolerated or not. The causes of disappointing retention in PPS region can be depend on the two factors. First factor was the involuntarily movements between the sot tissue of the hard and soft palate, at the time of primary PPS recording [3]. That recorded PPS gave unacceptable result in processed denture. That is not in clinician hand but the physiological reflexes of patient decide. Second factor was the polymerization shrinkage of the polymers [15]. The displacement of the soft tissue in the glandular area is a critical factor in the effectiveness of PPS [2, 5]. The clinically suggested compressible area was present to some extent beyond the fovea palatini and centrally around the mid line of Class III soft palate near posterior border of the maxillary denture. This area could not be registered, at the time of initial stages of a PPS registration because of the unwillingly movements between the hard and soft palate. The area exists just away from the primary palatal seal. This glandular area provides an additional reverse cupid bow- shape PPS to a trial maxillary denture. The marking of advocated PPS band was done by the Gentian violet (crystal violet, Methyl Violet 10B, hexamethyl pararosaniline chloride) is a bactericide and an agent. The Gentian violet was used by surgeons for the skin marking before suegery. The use of dough staged auto polymerizing resin in comparison of light cure denture resin is more economical for the trial prosthesis.
CONCLUSION
Precision is achieved, not when there is nothing more to add but when there is nothing left to take away. Extension of PPS in complete denture had been made with both intra and extra oral methods. In this case report, incorporation of the additional PPS has been done intra orally in trial maxillary denture with the auto polymerizing resin. It has increased the retention in the current, different configurated palate. Extended PPS does not initiate the gagging reflex. Used area for the addition is delineated with Gentian violet dye. Authors replace additional seal with the light polymerized reline resin in final prosthesis. Recommended area is significant to the aforesaid palatal classification. It offers a high quality of maxillary denture. Authors validate their finding and recommend further studies involving significant number of the patients.
REFERENCES
1. The Glossary Prosthodontics terms. 8th edition. J Prosthet Dent 2005; 94:10-92.
2. Winkler S. Essentials of complete denture prosthodontics. 2nd edition. St. Lois; 1994:107-122.
3. Brian MW, Robert F. Accurate location on postpalatal seal area on maxillary complete denture cast. J Prosthet Dent 2006; 96:454-5.
4. Lye TL. Significance of fovea palatine in complete denture. J Prosthet Dent 1975; 33:504.
5. Chen MS. Reliability of the fovea palatini for determing the posterior border of the maxillary denture. J Prosthet Dent 1980; 43;133-177.
6. Zarb GA, bolender Charles L. Text book of prosthodontic treatment for edentulous patients. 12th ed. St. Louis: Mosby; 2004:342-346
7. Ahal R, Bhargava K. Posterior palatal seal Part I and II. Journal of Indian Dental Association 1994; 65: 221-233.
8. Nallaswamy D, Ramaingagam K, Bhatt V. Text book of prosthodontics. 1ist edition. Delhi Jaypee brothers: 2003:25-27.
9. Hardy IR, Kapur kk. Posterior border seal & its rationale and importance. J Prosthet Dent 1958; 8:386-7.
10. Silverman SJ. Dimension and displacement patterns of PPS. J Prosthet Dent 1971; 25: 470-488.
11. Terrell WH. A precision technique that produces dentures that fit and function. J Prosthet Dent 1951; 1:353-377.
12. Sheila A, Henneman SA , kohn SF. Methods in cell science; Methylene blue staining of tissue culture monolayers: 1975.
13. Ward JE, Moon PC, Levine RA, Behrendt CL. Effect of repair surface design, repair material, and process method on the transverse strength of repaired acrylic denture resin. J Prosthet Dent 1992; 67:815-20.
14. Sato Y, et al.Immediate maxillary denture base extension for posterior palatal seal. J Prosthet Dent 2000; 83:371-3.
15. Anusavice K J. Phlillips'science of dental materials. 11th ed. St. Louis Saunders. 2007; 739-741. |