Introduction.
Fibrous dysplasia is a rare bone condition characterized by the replacement of healthy bone by fibrous tissue and different grades of bone metaplasia.1 It accounts for approximately 2% of bone tumours.2 If only one bony is involved, it is termed monostotic fibrous dysplasia. If more than one bone is involved, it is termed polyostotic fibrous dysplasia. Monostotic fibrous dysplasia is less serious than polyostotic form.3
Clinical presentation.
A 63 year old male patient reported to department of oral and maxillofacial surgery with complaint of swelling in left cheek region. The swelling had attained the current size after a gradual and slow growth since past 15 years. Patient had undergone the surgery for the same, 15 years back, but soon the lesion recurred. Patient also complained of an opening on the face with pus discharge in the region of the swelling. The swelling was painful but the severity of the pain increased 2 months before he reported to us. On examination, a 3.5 inch by 2.5 inch large swelling was seen on left cheek region. The swelling was hard, non tender and well demarcated from surrounding bone (Figure 1).
 | Figure 1: Pre Operative Frontal Photograph.
 |
On intra oral examination, the swelling was seen involving left maxillary alveolar ridge and hard palate with a dimension of 2 inch by 2 inch. (Figure 2)
 | Figure 2: Pre Operative Intra Oral Photograph
 |
The intraoral swelling was in continuation with extraoral swelling. There was a sinus opening in the left cheek region with pus discharge.
On attempted aspiration with an 18 gauge needle, the needle failed to penetrate the lesion. The clinical findings were suggestive of a benign tumour of the left maxilla. Infection control and pain control was achieved with antibiotics and analgesic therapy. Further radiological investigations were undertaken to establish the diagnosis. Orthopantamograph and Paranasal sinus view radiographs revealed a mixed radiopacity and radiolucency, giving a ground glass appearance involving whole of left maxillary sinus till the orbital floor. Computed tomography scan of the lesion revealed increased density with enlarged maxillary alveolus, marked deformity with bony expansion and mixed pattern ranging from cystic through ground glass to heavily mineralized tissue. The central area predominantly along the inferior aspect was showing typical "cotton wool appearance".(Figure 3)
 | Figure 3: C.T. Showing Space Occupying Lesion In Left Maxillary Region.
 |
The extent of the lesion was as follows:
Superior:
The lesion had caused deformity of orbital floor, which was pushed up with no evidence of infiltration of extraconal space.
Inferior:
Convex bulge at roof of oral cavity with erosion and expansion of hard palate.
Medial:
The lesion was encroaching ipsilateral nasal cavity. The nasal turbinates were eroded with bowing of nasal septum towards right.
Posterior:
The lesion was obviating pterygomaxillary fissure. The pterygoid plates were preserved.
Anterior:
There was contour bulge with thickening of the overlying soft tissue.
This large expansile bony lesion arising from alveolar process of left maxilla was having clinical and radiological presentation of fibrosseous lesion and Paget's disease.
Differential diagnosis
The clinical and radiological appearance of this maxillary swelling mimics a number of clinical entities. Metabolic bone diseases such as hyperparathyroidism produces similar pattern, but bone lesions in hyperparathyroidism are most likely to be polyostotic, bilateral and does not cause bone expansion. In our case, biochemical values, suggestive of hyperparathyroidism, such as serum calcium level, parathormone level were within normal limits, so, hyperparathyroidism was ruled out. Paget's disease was other consideration for this clinical and radiological presentation. Paget's disease is most commonly seen in elderly patients and maxilla is most common site of occurrence, as in seen in our case. Ground glass appearance or frosted glass appearance was seen in radiographs, which gives the radiological picture of fibrous dysplasia. Serum alkaline phosphatase was within normal limits, which is usually raised in Paget's disease.
Diagnosis.
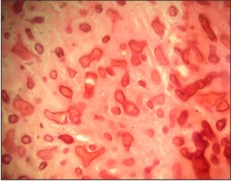
Incisional biopsy was planned and performed under local anaesthesia. Haematoxylin and eosin section revealed bony trabeculae evenly placed in fibrillar connective tissue. Chinese letter pattern was seen in the bony trabeculae. Collagen fibres of trabeculae were seen extending into the fibrous tissue. (Figure 4) A Correlatating clinical, radiological and histopathological finding, diagnosis of recurrent monostotic fibrous dysplasia of maxilla was established.
 | Figure 4: High Power Magnification Showing Chinese Letter Pattern.
 |
Management.
Hemimaxillectomy of left maxilla was planned under general anaesthesia. Weber fergusson incision was placed and flap was raised. The lesion was exposed and it was seen to be well demarcated from surrounding normal bone, which was an unlikely finding of fibrous dysplasia. The osteotomy cuts were placed to separate the maxilla from the surrounding maxillofacial skeleton. The maxilla was separated by deepening the cut with chisel. The defect was lined with collagen sheets (biological dressing) and sutured. Surgical stent was placed. An intermediate obturator was fabricated after 14 days. Further prosthodontic rehabilitation was done with permanent obturator after 2 months of surgery. (Figure 5)
 | Figure 5: Post Operative Photograph
 |
Discussion.
Monostotic fibrous dysplasia accounts to 80-85% of all fibrous dysplasias and jaws are most commonly affected sites.4 Monostotic fibrous dysplasia may occur at any age, but are most common in children and young adults.5
Surgery is the main stay of treatment for fibrous dysplasia, but the technique of surgery is controversial. The different modalities of treatment could be conservative recontouring of the lesion or radical excision of the lesion followed by autogenous grafting. In a review of treatment for fibrous dysplasia, success rate of conservative surgery was 74% initially and up to 86% after successive surgery.2 In another retrospective study of 12 cases of fibrous dysplasia of the maxillofacial bones, no relapse was found in any cases treated with radical excision, whereas three of the seven cases treated with conservative excision relapsed after few years.6
A clinicoradiological analysis of symptomatic craniofacial fibro-osseous lesions was done. The objective was to outline the clinical and radiological aspects of symptomatic craniofacial fibro-osseous lesions and to study the appropriate surgical management. It was concluded that treatment of craniofacial fibro-osseous lesion is highly individualized. A conservative approach may not be able to treat all cases of craniofacial fibro-osseous lesions. A more radical approach that includes a craniofacial resection or a total maxillectomy may be warranted in few cases.7, especially tumours invading the vital structures as in our case; it was invading the orbital rim and orbital floor.
In another retrospective study on 68 patients of craniomaxillary fibrous dysplasia, no disease recurrence was observed in cases treated with complete excision. Recurrence was seen in cases treated with conservative remodelling. In another case of remodelling, infection was seen, which resolved on antibiotic therapy. Palatal fistula was seen in two cases. This author prefers conservative approach only in polyostotic cases and mccune Albright syndrome and in most cases of monostotic or monofocal fibrous dysplasia, aggressive but definitive treatment was recommended.8
In another review regarding the management of aggressive midface and orbital fibrous dysplasia, aggressive resection and various degrees of reconstruction to optimize function was recommended. While fibrous dysplasia is classified as a benign process, local expansion can cause significant functional and aesthetic deformities. Each lesion should be thoroughly evaluated and, vital structures are involved or threatened, total of subtotal resection should be considered.9
In another description of 28 craniomaxillofacial fibrous dysplasia, patients were treated as early as the symptoms occurred. The principles of surgical treatment were based on zones of involvement.
Zone 1 :
Fronto-orbital, zygoma and upper maxillary region
Zone 2 :
Hair bearing skull
Zone 3 :
Central cranial base
Zone 4 :
Tooth bearing zone.
Radical surgeries were performed in
Zone 1
and conservative reshaping in
Zone 2,
Zone 3 and Zone 4.10
Conclusion and summary.
In a debate between, radical and conservative approach for the treatment of fibrous dysplasia of maxilla, a new dimension emerges, which can be termed curative. Curing the lesion is the prime concern for the surgeon, for which any customized approach tailored to the individual patient is adopted.
Funding : none
Conflict of interest: none
References:
1. Carreto sanchez J, Balderrama caballero DH, Relea calataynd MF (1997) Monostotic fibrous dysplasia of the upper maxilla. A case report. Acta otorrinolaringol Esp 48(7): 579-82.
2. Pinsolle V, Rinel J, Michelet V, Majoufre C, Pinsolle J (1998) Treatment of fibrous dysplasia of the craniofacial bones. Report of 25 cases. Ann Chir Plast Esthet 43(3):234-9.
3. Shafer WG, Hine MK, Levy BM (2003) A text book of oral pathology, sect 5, chap 1.WB Saunders co. philadelphia
4. Neville B.W, Damm DD, Allen CM, Bouquot JE (2002) Oral and maxillofacial pathology, chapter 14. WB Saunders co. philadelphia
5. Bhaskar SN. Synopsis of oral pathology, part 3, chap 11. The C.V. Mosby Company. St. Louis
6. Garau V, Tartaro GP, Aquino S, Colella G (1977) Fibrous dysplasia of the maxillofacial bones. Clinical considerations. Minerva Stomatol 46(10): 497-505.
7. Panda NK, Parida PK, Sharma R, Jain A, Bapuraj JR(2007) A clinicoradiologic analysis of symptomatic craniofacial fibro-osseous lesions. Otolaryngol Head and Neck Surg. 136(6):928-33.
8. Vasentini V, Cassoni A, Marianetti TM, Terenzi V, Fadda MT, Lanetti G (2009) Craniomaxillofacial fibrous dysplasia: Conservative treatment or radiacal surgery? A retrospective study on 68 patients. Plast Reconstr Surg. 123(2):653-60.
9. Frodel JL, Funk G, Boyle J, Richardson M (2000) Management of aggressive midface and orbital fibrous dysplasia. Arch Facial Plast Surg. 2(3): 187-95.
10. Chen YR, Noordhoff MS (1990) Treatment of craniomaxillofacial fibrous dysplasia: how early and how extensive. Plast. Reconst surg. 86(5):835-44.
|